
Effect of diabetes on the prognosis, serum inflammatory factors, and quality of life of patients with lower extremity arteriosclerosis obliterans after vascular intervention: a retrospective comparative cohort study
Introduction
Lower extremity arteriosclerosis obliterans (LEASO) is a common disease in vascular surgery. As a result of arteriosclerosis, the intima of blood-supplying arteries in the lower limbs is thickened, the lumen is narrowed or blocked, and the blood supply of diseased limbs is insufficient, resulting in intermittent claudication, resting pain, and even ulceration or necrosis of the lower limbs. LEASO is a chronic progressive disease with clinical manifestations such as systemic arteriosclerosis in the lower limbs (1). In China, the incidence rate of LEASO is increasing every year; according to the latest epidemiological statistics, the number of patients in China may be as high as 45.3 million (2). The reality of LEASO treatment in China is unclear owing to a lack of bulk data statistics. Meanwhile, in Western countries with developed medical systems, many LEASO patients still require amputation due to delayed diagnosis and treatment (3).
Diabetes mellitus (DM) is a group of metabolic diseases characterized by hyperglycemia. With the aging of the population and changes in lifestyle, the prevalence of DM has risen sharply and is now a serious global public health problem. According to the results of the Global Burden of Disease (GBD) study, compared with 2007, the incidence and mortality rates of DM worldwide increased by 27.3% and 25.6%, respectively, in 2017 (4). From 1990 to 2017, the global DM burden showed an upward trend, with the fastest increase in developed regions such as Western Europe (5). In terms of incidence, China is currently one of the fastest-growing countries, with about 11% of the population suffering from DM, of which the proportion of type 2 diabetes mellitus (T2DM) is over 90% (6).
Diabetic vascular disease is a common complication of DM and is typically divided into macrovascular and microvascular disease. The former primarily affects cerebral arteries, coronary arteries, peripheral arteries of limbs, etc., while the latter mainly causes diabetic retinopathy, diabetic nephropathy, and neuropathy. Diabetic lower extremity arterial disease is a common vascular complication of type 2 diabetes, which seriously affects the quality of life of diabetic patients. It has been reported that the incidence of LEASO in diabetic patients accounts for about 20–50% of those with type 2 diabetes (7). Compared with simple LEASO patients, the symptoms of distal limb ischemia are the main symptoms in the early stage of LEASO in diabetic patients, which can manifest as intermittent claudication and rest pain. However, most patients often experience peripheral neuropathy, which cause symptoms to be masked or atypical.
Patients with severe ischemia are prone to developing diabetic foot and often lose the opportunity to save the limb. Amputation caused by diabetic foot ranks first among all types of non-traumatic amputations, and dry gangrene caused by LEASO is the primary cause of diabetic foot amputation (8). LEASO in diabetic patients is complicated and difficult to treat. Although it can be temporarily relieved by medical treatment alone, if the problem of lower extremity arterial disease cannot be effectively resolved, patients will often require amputation due to severe limb necrosis and infection. With the development of endovascular treatment materials and technologies, the clinical effect of vascular intervention for the treatment of LEASO has been continuously improved and has become the primary method for the treatment of such diseases, however, studies in various countries have found that the treatment success rate and effect are different, and the treatment effect is affected by many factors, such as age, gender, smoking and other risk factors, and there are many disputes about whether DM affects the efficacy of intravascular interventional therapy for LEASD (9,10). Therefore, this study retrospectively analyzed the clinical data of 233 patients with LEASO who received percutaneous transluminal angioplasty (PTA), aiming to explore the clinical efficacy and safety of vascular interventional therapy. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-827/rc).
Methods
Research participants
This study retrospectively analyzed 223 LEASO patients (256 limbs) treated with PTA in the Blood Hernia Minimally Invasive Surgery Ward of Xuzhou Central Hospital from January 2017 to December 2021. Each limb was analyzed as a separate case (Figure 1).
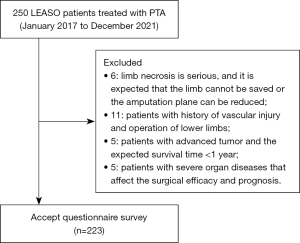
Patients who received PTA and/or stent placement for LEASO were eligible for inclusion in this study. The exclusion criteria were as follows: (I) patients with serious limb necrosis such that it was expected that the limb could not be saved or the amputation plane could be reduced; (II) patients with a history of vascular injury and lower limb surgery; (III) patients with advanced tumors and an expected survival time <1 year; and (IV) patients with severe organ diseases that affect the surgical efficacy and prognosis.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and was approved by the Ethics Committee of Xuzhou Central Hospital (No. 2017019). Informed consent was obtained from the included patients.
Treatment methods
The patients were treated with PTA based on conventional conservative treatment. The blood glucose in the diabetes group was preoperatively controlled (fasting blood glucose <7.5 mmol/L, 2 h postprandial blood glucose <11.0 mmol/L). Antegrade puncture was performed in patients with a normal proximal end of the ipsilateral iliac and femoral arteries. Contralateral femoral artery retrograde puncture was applied in patients with ipsilateral iliac and proximal femoral artery lesions. After systemic heparinization, angiography was performed on the arteries of the affected extremities. In general, femoral and popliteal artery lesions were treated with 5–6 mm diameter balloons, iliac artery lesions with 7–8 mm diameter balloons, and inferior genicular artery lesions with 2–4 mm diameter balloons. The balloon length was selected according to the length of the lesion segment Following successful balloon dilatation, angiography was performed again. If the elastic retraction was obvious or the dissection was formed, the stent was placed. Patients with multi-segmental lesions were treated according to the principle of “far before near”. Vasodilator and antiplatelet therapy were continued postoperatively (clopidogrel 75 mg/d for 6 months, and aspirin 100 mg/d for life). Ulcer patients should be treated with wound management.
Perioperative management
Low molecular weight heparin was used for routine anticoagulation for 1 week postoperatively. Also, aspirin was taken orally for a long period after discharge, and clopidogrel was taken orally for stent implantation for 6 months.
Postoperative follow-up
The patients were followed up once every 3, 6, and 12 months after surgery and once every year thereafter.
Observation index
Ankle-brachial index (ABI)
We measured the brachial artery systolic blood pressure (BSBP) on both arms respectively and took the average value. If the systolic pressure on both sides was greater than 10 mmHg, we took the higher value after repeated measurement. Next, we measured the ipsilateral dorsal artery systolic blood pressure (DSBP) and took the higher value as the ankle systolic pressure. We then divided the measured DSBP by the BSBP on the same side to obtain the ABI value.
Detection of inflammatory factors
Before and after treatment, 3 mL of fasting venous blood was collected from patients in the two groups, centrifuged at a speed of 3,500 r/min for 10 min, and serum interleukin-6 (IL-6) and tumor necrosis factor-α (TNF-α) were detected by enzyme-linked immunosorbent assay (ELISA). Also, serum C-reactive protein (CRP) was detected by immunoturbidimetry.
Technical success
Technical success was indicated by postoperative angiography showing that the lumen of the diseased vessels was unblocked, the blood flow velocity was fast, and the restenosis rate was <30%; or more than one of the three inferior genicular arteries was unblocked to below the ankle and the blood flow velocity was normal.
Resting pain relief
The degree of pain was scored using the visual analog score (VAS).
Clinical success
No further intervention was given from the first PTA and/or stent implantation to the follow-up time point.
Quality of life
Medical outcomes were evaluated using the 36-item Short-Form Health Survey (SF-36) (11): there are eight dimensions in SF-36: physical functioning (PF), role-physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional (RE), and mental health (MH). The scale comprehensively summarizes the respondents’ quality of life from the above eight aspects. Each index score is 0–100 points, and the score directly reflects the health status; the higher the score, the higher the quality of life of the patient.
Statistical analysis
After the questionnaire was classified and numbered, the data were statistically analyzed using social science software version 23.0 (SPSS company, Chicago, Illinois, USA). The mean ± standard deviation (SD) is used to describe the measurement data of normal distribution, and the frequency and percentage are used to describe the classification data. The t-test of independent samples was used for inter group comparison. Chi square test was used to compare the frequency data between groups. Binary logistic regression analysis was used for multivariate analysis.
All statistical tests conducted were two-tailed with P<0.05 used as the level of statistical significance.
Results
Basic patient characteristics
In the diabetic group, there were 64 male patients (82.1%) and 14 female patients (17.9%), aged (73.10±4.83) years. In the non-diabetic group, there were 127 male patients (87.6%) and 18 female patients (12.4%), aged (73.28±4.56) years. There were no significant differences in age, sex, complications, and Rutherford stage ratio between the two groups (P>0.05), as shown in Table 1.
Table 1
| Factor | Diabetic group | Non-diabetic group | t/χ2 | P |
|---|---|---|---|---|
| Age (years), mean ± SD | 73.10±4.83 | 73.28±4.56 | 0.276 | 0.783 |
| Gender, n (%) | 1.264 | 0.261 | ||
| Male | 64 (82.1) | 127 (87.6) | ||
| Female | 14 (17.9) | 18 (12.4) | ||
| Complication, n (%) | ||||
| Hyperhomocysteinemia | 15 (19.2) | 22 (15.2) | 0.604 | 0.437 |
| Hyperlipidemia | 25 (32.1) | 37 (25.5) | 1.079 | 0.299 |
| Hypertension | 38 (48.7) | 67 (46.2) | 0.128 | 0.720 |
| Coronary heart disease or cardiovascular and cerebrovascular disease | 22 (28.2) | 20 (13.8) | 6.891 | 0.009 |
| Rutherford stage, n (%) | 2.112 | 0.715 | ||
| 2 | 4 (5.1) | 10 (6.9) | ||
| 3 | 9 (11.5) | 24 (16.6) | ||
| 4 | 27 (34.6) | 49 (33.8) | ||
| 5 | 9 (11.5) | 19 (13.1) | ||
| 6 | 29 (37.2) | 43 (29.7) |
Comparison of vascular lesion sites of the lower limbs between the two groups
Compared with the non-diabetic group, the diabetic group had a lower proportion of lesions in the superior genicular artery and a higher proportion in the inferior genicular artery (P<0.05), as shown in Table 2.
Table 2
| Factor | Superior genicular artery | Inferior genicular artery | ||||
|---|---|---|---|---|---|---|
| Femoral artery | Popliteal artery | Arteriae tibialis anterior | Posterior tibial artery | Peroneal artery | ||
| Diabetic group, n (%) | 61 (67.03) | 42 (46.15) | 56 (61.54) | 45 (49.45) | 53 (58.24) | |
| Non-diabetic group, n (%) | 130 (78.79) | 110 (66.67) | 70 (42.42) | 61 (36.97) | 65 (39.39) | |
| c2 | 15.326 | |||||
| P | 0.0041 | |||||
Comparison of the technical success rate between the two groups
In the diabetic group, the technical success rate was 85.71%, and the 10 unsuccessful cases (13 limbs) were middle and long segment occlusive lesions under the knee. In the non-diabetic group, the technical success rate was 91.52%, and the 10 unsuccessful cases (14 limbs) were long segment occlusive lesions There was no significant difference between groups (χ2=2.092, P=0.148).
Comparison of the ABI between the two groups
The ABI of the diabetic group was 0.31±0.12 before treatment and 0.75±0.16 after treatment, while that of the non-diabetic group was 0.33±0.15 and 0.80±0.20, respectively. There were no significant differences between the two groups before and after treatment (P>0.05). Compared with that before treatment, the ABI of the two groups increased markedly after treatment (P<0.001), as shown in Table 3.
Table 3
| Factor | Diabetic group | Non-diabetic group | t | P |
|---|---|---|---|---|
| Preoperative ABI | 0.31±0.12 | 0.33±0.15 | 0.979 | 1.861 |
| Postoperative ABI | 0.75±0.16 | 0.80±0.20 | 0.329 | 0.064 |
| t | 18.518 | 22.231 | ||
| P | <0.001 | <0.001 |
ABI, ankle-brachial index.
Comparison of the serum inflammatory factors between two groups before and after treatment
Before treatment, the CRP, IL-6, and TNF-α levels in the diabetic group were (9.23±1.59) mg/L, (2.98±0.12) µg/L, and (48.05±10.87) ng/L, respectively, and after treatment were (5.07±0.41) mg/L, (1.85±0.44) µg/L, and (12.86±1.47) ng/L, respectively. As for the non-diabetic group, the pre-treatment values of these serum inflammatory factors were (9.07±1.67) mg/L, (2.99±0.11) µg/L, and (48.65±9.57) ng/L, respectively, and were (2.98±0.27) mg/L, (1.08±0.21) µg/L, and (7.87±1.19) ng/L, respectively, post-treatment. There were no statistically significant differences in the levels of these inflammatory factors between the diabetic and non-diabetic groups before and after treatment (P>0.05). As shown in Table 4, the levels of these inflammatory factors in both groups after treatment were significantly lower than those before treatment (P<0.05).
Table 4
| Variable | Preoperative | Postoperative | |||
|---|---|---|---|---|---|
| Diabetic group | Non-diabetic group | Diabetic group | Non-diabetic group | ||
| CRP (mg/L) | 9.23±1.59 | 9.07±1.67 | 5.07±0.41a | 2.98±0.27ab | |
| IL-6 (μg/L) | 2.98±0.12 | 2.99±0.11 | 1.85±0.44a | 1.08±0.21ab | |
| TNF-α (ng/L) | 48.05±10.87 | 48.65±9.57 | 12.86±1.47a | 7.87±1.19ab | |
Compared with before treatment, aP<0.05; compared with the Diabetic group, bP<0.05. CRP, C-reactive protein; IL-6, interleukin-6; TNF-α, tumor necrosis factor-α.
Comparison of perioperative complications between the two groups
As shown in Table 5, we compared the diabetic and non-diabetic groups in terms of the following perioperative complications: bleeding, 2.6% vs. 2.1% (χ2=0.057, P=0.812); hematoma, 2.6% vs. 2.1% (χ2=0.057, P=0.812); pseudoaneurysm, 1.3% vs. 0.7% (χ2=0.200, P=0.655); acute stent thrombosis, 1.3% vs. 2.1% (χ2=0.178, P=0.673); and blood flow-restricted dissection, 3.8% vs. 3.4% (χ2=0.023, P=0.897).
Table 5
| Variable | Diabetic group | Non-diabetic group | c2 | P |
|---|---|---|---|---|
| Hemorrhage, n (%) | 2 (2.6) | 3 (2.1) | 0.057 | 0.812 |
| Hematoma, n (%) | 2 (2.6) | 3 (2.1) | 0.057 | 0.812 |
| Pseudoaneurysm, n (%) | 1 (1.3) | 1 (0.7) | 0.200 | 0.655 |
| Acute stent thrombosis, n (%) | 1 (1.3) | 3 (2.1) | 0.178 | 0.673 |
| Flow-limiting dissection, n (%) | 3 (3.8) | 5 (3.4) | 0.023 | 0.897 |
Follow-up results
At 12 months postoperatively, the number of clinical successes in the diabetic group was 72 (79.12%), and there were no deaths. As for the non-diabetic group, the number of clinical successes was 147 (89.09%), and there were no deaths. The difference between the groups was statistically significant (P<0.05). Sixty-nine (75.82%) cases were relieved of rest pain in the diabetes group, while 142 (86.06%) cases were relieved by rest pain in the non-diabetic group, and this difference was statistically significant (P<0.05).
In the diabetic group, there were a total of 12 amputations (13.19%), including 2 (2.20%) above-knee amputations and 10 (10.99%) below-knee amputations. There were a total of 8 amputations in the non-diabetic group (4.84%), which included 4 (2.42%) above-knee amputations and 4 (2.42%) below-knee amputations. The amputation and below-knee amputation rates in the diabetic group were higher than those in the non-diabetic group, and the difference between the groups was statistically significant (P<0.05), as shown in Table 6.
Table 6
| Variable | Diabetic group | Non-diabetic group | χ2 | P |
|---|---|---|---|---|
| Clinical success rate, n (%) | 72 (79.12) | 147 (89.09) | 4.715 | 0.030 |
| Resting pain relief rate, n (%) | 69 (75.82) | 142 (86.06) | 4.242 | 0.039 |
| Amputation rate, n (%) | 12 (13.19) | 8 (4.84) | 5.662 | 0.017 |
| Upper knee amputation rate, n (%) | 2 (2.20) | 4 (2.42) | 0.013 | 0.009 |
| Below knee amputation rate, n (%) | 10 (10.99) | 4 (2.42) | 8.322 | 0.004 |
Comparison of the quality of life of patients between the two groups
At 12 months post-treatment, the scores of the SF-36 dimensions in the two groups were significantly increased (P<0.05), and the scores of BP, GH, and MH in the non-diabetic group were markedly higher than those in the diabetic group (P<0.001), as shown in Table 7.
Table 7
| Variable | Before intervention | After intervention | |||
|---|---|---|---|---|---|
| Diabetic group | Non-diabetic group | Diabetic group | Non-diabetic group | ||
| PF | 55.87±3.99 | 55.74±4.08 | 69.15±6.91a | 70.79±5.97a | |
| RP | 56.21±3.79 | 56.44±3.95 | 70.31±4.92a | 70.47±4.97a | |
| BP | 47.63±5.58 | 46.54±6.00 | 61.05±5.66a | 63.34±5.34ab | |
| GH | 51.95±5.29 | 51.34±5.56 | 63.63±6.80a | 68.73±5.90ab | |
| VT | 53.82±5.75 | 53.01±4.79 | 67.56±4.58a | 66.57±4.74a | |
| SF | 54.99±4.86 | 55.56±4.44 | 68.45±5.52a | 68.29±4.28a | |
| RE | 50.4±5.78 | 50.76±4.25 | 67.59±5.04a | 66.79±4.83a | |
| MH | 57.81±4.54 | 56.77±4.34 | 60.96±5.1a | 68.95±5.98ab | |
Compared with before treatment, aP<0.05; compared with the control group, bP<0.05. SF-36, 36-item Short-Form Health Survey; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health.
Analysis of the influencing factors of clinical success rate
According to the clinical success rates at 12 months postoperatively, the patients were divided into a clinical success group (n=219) and a clinical failure group (n=37). The ages, genders, Rutherford stages, diabetic vs. non-diabetic status, and serum inflammatory factors of the two groups were analyzed by logistic regression analysis. The analysis showed that Rutherford stage, diabetic vs. non-diabetic status, and CRP were independent factors affecting clinical success, as shown in Table 8.
Table 8
| Related factor | B | Ward | P | OR | 95% CI |
|---|---|---|---|---|---|
| Rutherford stage | 3.175 | 6.213 | 0.01 | 20.124 | 2.039–4.786 |
| Diabetes | 3.787 | 9.481 | 0.004 | 44.893 | 4.289–114.067 |
| CRP | 2.264 | 7.315 | 0.038 | 14.523 | 2.963–83.165 |
OR, odds ratio; CI, confidence interval; CRP, C-reactive protein.
Discussion
The vascular diseases of diabetes LEASO often involve the whole vascular system, and the treatment of diseases below the popliteal artery is particularly difficult (12). Most LEASO patients are elderly and are accompanied by multiple organ dysfunction. The traditional surgical treatment usually needs to be performed under epidural or general anesthesia. However, due to the risks of anesthesia, significant surgical trauma, intraoperative heparin anticoagulation, collateral artery injury during surgery, greater intraoperative bleeding, and a relatively long operation time, the rates of perioperative mortality and complications are relatively high in elderly diabetic and high-risk patients. Moreover, some patients with restenosis or occlusion after arterial bypass surgery of the lower limbs cannot tolerate invasive surgical treatment again due to poor general conditions or unsuitability for reoperation due to more extensive vascular diseases of the lower limbs. For these patients, conservative treatment is adopted. Consistent with other reports, diabetes has been considered an independent predictor of the failure of percutaneous intervention for lower extremity vascular diseases (13). Most patients with LEASO are older than 70 years old, often accompanied by diabetes, hypertension, renal insufficiency, and coronary heart disease (14,15). Lee et al. (16) found that compared with non-diabetic LEASO patients, diabetic patients with LEASO tend to have more severe ischemic symptoms, especially Rutherford stages 5 and 6. These patients often delay seeing a doctor due to peripheral neuropathy and therefore develop diabetic foot. Diabetic patients with renal insufficiency, coronary heart disease, and cerebrovascular disease significantly outnumber non-diabetic patients. This study found that patients in the diabetic group had more complications than those in the non-diabetic group; however, owing to the small number of included patients, the data did not indicate that this difference was statistically significant.
Patients with diabetes often suffer from lower extremity vascular disease, neuropathy, and infection. Lower extremity vascular disease mostly occurs in the legs and feet, and most of them are long segment artery stenoses or occlusions (17). Comparing the pathological characteristics of the two groups in this study, the proportion of inferior genicular artery lesions in the diabetic group was significantly higher than that in the non-diabetic group, and the proportion of middle and long segment occlusive lesions in the diabetic group was markedly higher than that in the non-diabetic group.
For peripheral vascular diseases, especially in diabetic patients, there are often poor conditions such as autologous great saphenous vein, outflow tract occlusion, concomitant cardiovascular disease, chronic obstructive pulmonary disease, and so on (18). At present, endovascular treatment is the first-line option. Multiple factors affect the patency of subgenual disease in diabetes patients due to small vessel diameter and diffuse lesions. The success rate of endovascular treatment is low and the restenosis rate is high. In this study, the technical success rate of the diabetic group (85.71% vs. 91.52%) was lower than that of the non-diabetic group, but the difference was not statistically significant, suggesting that diabetes did not affect the treatment success rate. In patients with diabetes, blood vessels are often severely calcified, especially below the knee, which will affect the success rate of surgery to a certain extent. At the same time, diabetes patients with LEASO have severe limb ischemia symptoms and are often complicated with diabetic foot. Following endovascular treatment, multiple interventions are usually required, which reduces the clinical success rate. In this study, the clinical success rate of the diabetic group was significantly lower than that of the non-diabetic group (79.12% vs. 89.09%).
The ABI decreased with the reduction of arterial blood supply to the lower extremities, and the decrease was positively correlated with the degree of ischemia in the lower extremities. The ABI has been widely used for the early diagnosis, condition evaluation, intraoperative examination, and treatment effect follow-up of arteriosclerosis obliterans (ASO). It has the advantages of being non-invasive, safe, repeatable, and highly accurate. In this study, the changes in ABI before and after surgery in ASO patients were measured to compare the postoperative hemodynamic response. It was found that the postoperative ABI of the two groups was significantly increased, suggesting that endovascular therapy was effective in improving the blood supply of the affected limbs and did not affect the postoperative hemodynamic response due to the complication of diabetes. However, whether diabetes affects the efficacy of ASO patients remains controversial at home and abroad. Mutirangura et al. (10) believed that there was no significant difference in the short-term efficacy between patients with and without diabetes after intracavitary therapy. Some scholars also believe that compared with non-diabetic patients, diabetes significantly affects the long-term survival and limb salvage rates of ASO patients treated with endovascular therapy (19).
CRP is an important inflammatory mediator; when its levels are high, it can damage blood vessels and cause lipid deposition in the arterial intima, which leads to the occurrence of atherosclerosis (20). TNF-α, as a pro-inflammatory factor, can promote the secretion of IL-6, cause damage to endothelial cells, cause thrombosis, and lead to blood vessel stenosis and occlusion (21). The results of this study showed that the serum levels of IL-6, CRP, and TNF-α in the diabetic group were significantly higher than those in the control group, which is consistent with the results of Wen et al. (22). Their research also suggested that the levels of IL-6, CRP, and TNF-α were involved in the occurrence and development of LEASO, and were reliable indicators for evaluating the severity of LEASO. In this study, the levels of inflammatory factors (IL-6, CRP, and TNF-α) after surgery were lower than those before surgery (P<0.05), indicating that endovascular intervention can reduce the levels of inflammatory factors in patients with LEPAO.
Since it cannot be completely cured, LEASO is a chronic disease. The goal of treatment is to enable patients to live their own lives through active management of the disease, including the prevention of cardiovascular events, improvement of quality of life, and promotion of people’s better participation in life and production (23). The quality of life of patients with LEASO is related to numerous factors, including gender, age, physical function status, complications, and relevant treatment measures (24). The disease has a serious impact on patients both physically and psychologically, which does not only depend on the severity of the disease (ABI) and the success of clinical interventions. Considering that patients with arteriosclerosis obliterans have psychological and emotional disorders, clinicians should provide comprehensive management for patients with arteriosclerosis obliterans of the lower limbs based on PTA treatment, so that they may eliminate bad living habits, actively monitor and control risk factors, and encourage patients to take appropriate physical exercise and participate in social activities. This will facilitate improvement of the physical and mental health of patients and comprehensively enhance their quality of life.
Conclusions
The short-term efficacy of PTA in treating diabetic patients with LEASO is similar to that of non-diabetic patients, but the long-term clinical success rate and quality of life of diabetes patients are still worse than those of non-diabetic patients. Standardized postoperative anti-inflammatory treatment and blood glucose control are important for long-term efficacy.
This study had some limitations that should be noted. Firstly, the subjects were all from one city, so there may be some regional bias. Secondly, the study was limited to one hospital and was therefore not representative. Further multi-center experimental research should be carried out on this topic.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-827/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-827/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-827/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of this work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and was approved by the Ethics Committee of Xuzhou Central Hospital (No. 2017019). Informed consent was obtained from the included patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Conte MS, Bradbury AW, Kolh P, et al. Global vascular guidelines on the management of chronic limb-threatening ischemia. J Vasc Surg 2019;69:3S-125S.e40.
- Wang Z, Wang X, Hao G, et al. A national study of the prevalence and risk factors associated with peripheral arterial disease from China: The China Hypertension Survey, 2012-2015. Int J Cardiol 2019;275:165-70. [Crossref] [PubMed]
- Nickinson ATO, Coles B, Zaccardi F, et al. Missed Opportunities for Timely Recognition of Chronic Limb Threatening Ischaemia in Patients Undergoing a Major Amputation: A Population Based Cohort Study Using the UK's Clinical Practice Research Datalink. Eur J Vasc Endovasc Surg 2020;60:703-10. [Crossref] [PubMed]
- Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet 2020;395:200-11. [Crossref] [PubMed]
- Khan MAB, Hashim MJ, King JK, et al. Epidemiology of Type 2 Diabetes - Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health 2020;10:107-11. [Crossref] [PubMed]
- Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia 2018;61:1249-60. [Crossref] [PubMed]
- Johnston LE, Stewart BT, Yangni-Angate H, et al. Peripheral Arterial Disease in Sub-Saharan Africa: A Review. JAMA Surg 2016;151:564-72. [Crossref] [PubMed]
- Ning G, Bloomgarden Z. Diabetes in China: prevalence, diagnosis, and control. J Diabetes 2013;5:372. [Crossref] [PubMed]
- Song YH, Zheng XT. Progress and prospect of the treatment of lower extremity arteriosclerosis obliterans. Zhonghua Wai Ke Za Zhi 2021;59:967-71. [PubMed]
- Mutirangura P, Ruangsetakit C, Wongwanit C, et al. Comparative study of the management of diabetic versus nondiabetic patients with atherosclerosis obliterans of the lower extremities. Vascular 2008;16:333-9. [Crossref] [PubMed]
- Newnham EA, Harwood KE, Page AC. Evaluating the clinical significance of responses by psychiatric inpatients to the mental health subscales of the SF-36. J Affect Disord 2007;98:91-7. [Crossref] [PubMed]
- Klinkert P, Schepers A, Burger DH, et al. Vein versus polytetrafluoroethylene in above-knee femoropopliteal bypass grafting: five-year results of a randomized controlled trial. J Vasc Surg 2003;37:149-55. [Crossref] [PubMed]
- Muradin GS, Bosch JL, Stijnen T, et al. Balloon dilation and stent implantation for treatment of femoropopliteal arterial disease: meta-analysis. Radiology 2001;221:137-45. [Crossref] [PubMed]
- Kim SJ, Kim W, Kim JB, et al. Determinants of procedural success and patency following subintimal angioplasty in patients with TASC C and D femoropopliteal arterial disease. Circ J 2010;74:1959-64. [Crossref] [PubMed]
- Sun J, Deng Q, Wang J, et al. Novel Insight Into Long-Term Risk of Major Adverse Cardiovascular and Cerebrovascular Events Following Lower Extremity Arteriosclerosis Obliterans. Front Cardiovasc Med 2022;9:853583. [PubMed]
- Lee MS, Rha SW, Han SK, et al. Comparison of diabetic and non-diabetic patients undergoing endovascular revascularization for peripheral arterial disease. J Invasive Cardiol 2015;27:167-71. [PubMed]
- Takahara M. Diabetes Mellitus and Lower Extremity Peripheral Artery Disease. JMA J 2021;4:225-31. [Crossref] [PubMed]
- Menard MT, Belkin M. Infrapopliteal intervention for the treatment of the claudicant. Semin Vasc Surg 2007;20:42-53. [Crossref] [PubMed]
- Abularrage CJ, Conrad MF, Hackney LA, et al. Long-term outcomes of diabetic patients undergoing endovascular infrainguinal interventions. J Vasc Surg 2010;52:314-22.e1-4.
- Li W, Liu X, Liu L, et al. Relationships of Serum Bone Turnover Markers With Metabolic Syndrome Components and Carotid Atherosclerosis in Patients With Type 2 Diabetes Mellitus. Front Cardiovasc Med 2022;9:824561. [Crossref] [PubMed]
- Liu S, Wang C, Guo J, et al. Serum Cytokines Predict the Severity of Coronary Artery Disease Without Acute Myocardial Infarction. Front Cardiovasc Med 2022;9:896810. [Crossref] [PubMed]
- Wen S, Li B, Jin Y, et al. Relation between serum inflammatory factors and lower-limb arteriosclerosis obliterans. Int J Clin Exp Med 2017;10:7965-72.
- He Y, Xie C, Xia Y, et al. Humanistic care interventions in patients with lower extremity arteriosclerosis obliterans. Am J Transl Res 2021;13:10527-35. [PubMed]
- Keeling AN, Naughton PA, O'Connell A, et al. Does percutaneous transluminal angioplasty improve quality of life? J Vasc Interv Radiol 2008;19:169-76. [Crossref] [PubMed]
(English Language Editor: A. Kassem)


