
Illness uncertainty and its associated factors in coronary heart disease patients with heart stent implantation: a cross-sectional study
Introduction
Disease uncertainty refers to the lack of ability to determine the significance of disease-related events (such as disease process, hospitalization, treatment, prognosis, etc.), the inability to assess the value of events, and the inability to accurately predict the outcome of related events (1), It reduces patient compliance, increases postoperative complications, and increases healthcare costs (2-4). Many studies have shown (5-7): marital status, age, education level, social status, social support, coping style, disease-related knowledge, etc. are significant influencing factors of uncertainty. At present, the heart stent implantation is widely used in patients with coronary heart disease. Medical staff usually pay more attention to the operation itself, and few people pay attention to the psychological needs of patients. Due to lack of disease-related knowledge, fear of recurrence of symptoms, and doubts about the effect of surgery, patients cannot form a correct cognitive framework for the disease, which in turn leads to a sense of uncertainty (8). In addition, uncertainty also stimulates sympathetic nerves, causing positive inotropic responses such as accelerated heartbeat and increased blood pressure (9,10), further increasing the burden on the heart (11,12), making it more prone to adverse life events. As a result, it has a series of negative effects on patients’ lifestyle compliance, self-management level, and quality of life (2-4). According to the literature review, there are few studies on the factors affecting the illness uncertainty of coronary heart disease patients and their correlation with self-management and quality of life. Therefore, it is necessary to explore the status and influencing factors of disease uncertainty in patients with cardiac stent implantation, and to provide a scientific basis for taking targeted nursing interventions in the future, thereby reducing disease uncertainty, improving self-management level, and improving prognosis and quality of life is paramount. We present the following article in accordance with the STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-528/rc).
Methods
Study design
This study adopted a cross-sectional study design and simple random sampling was used. A survey design was used with questionnaires from January to July 2021. Data collection on background information of demographics, uncertainty in illness, self-management behaviour and the quality of life were conducted to explore the level of illness uncertainty and its associated factors in coronary heart disease patients with heart stent implantation.
Setting and samples
Participants were recruited from one hospital located in Shanghai. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Huadong Hospital (No. 20200082). The participants and their family members were informed of the study’s objective and were ensured of the principles of confidentiality and voluntariness. Written informed consent was provided by the patients. The selection criteria of the sample of participants were (I) clinically diagnosed with coronary heart disease (CHD) and underwent cardiac stenting at an appropriate time, (II) with a clear mind and able to read and answer the questionnaire independently or with the researcher’s help, and (III) ≥18 years of age. The exclusion criteria were as follows: (I) comorbidity of other severe cardiovascular diseases, (II) subject to major personal or family events such as divorce or significant financial issues, and (III) difficulty to communication (severe mental or cognitive disorder) and unable to complete the questionnaire. The sample size was estimated based on the sample size calculation formula: N = Z2 × (P × (1–P))/E2, (where N is the sample size, Z is the statistic, E is the error value, and P is the probability value; when the confidence interval is 95%, Z=1.96). Combined with literature (13), heart disease is uncertain. The overall sense is at a moderate level, the probability P value is 60%, when the allowable error value is 10%, plus the 10–15% loss to follow-up rate, resulting in a required sample size of 92 cases at least for this study, and 191 coronary heart disease patients with heart stent implantation included in this study.
Data collection
The data were collected from January to July 2021. Data collection included demographic information, uncertainty in illness, self-management behaviour and the quality of life. The members of the intensively-trained research team (with five members including one doctor, three masters, and one master candidate in terms of academic degree; or two chief physicians and professors of nursing, two nurses-in-charge, and one attending doctor in terms of professional title; four were from the Cardiovascular Department and one from the Nursing Management Department; with an average of 16.8±12.3 years of experience in the field) distributed the questionnaires to the participants, guided them to answer the questionnaires independently with unified expressions, collected all questionnaires on the spot, and checked the answers. Based on the inclusion and exclusion criteria, 191 coronary heart disease patients with heart stent implantation were recruited from one hospital in Shanghai, whereas 23 invalid questionnaires were removed, from which a total of 168 eligible questionnaires were obtained, and the valid response rate was 87.9%.
Questionnaires
This study used a General Information Questionnaire, the validated Chinese Version of Mishel’s Uncertainty in Illness Scale (MUIS), Coronary Self-Management Scale (CSMS) and the 36-item Short Form Health Survey Scale (SF-36).
Demographical and disease-related characteristics
After determining the typical associated factors for illness uncertainty by reviewing previous literature, the research team independently designed the General Information Questionnaire, which covered 11 items: gender, age, culture, retirement, marriage, number of stents, degree of improvement of subjective symptoms, frequency of angina pectoris, nurse support during hospitalization, care of family members after discharge, and nurse follow-up after discharge.
MUIS
Professor Sheila Sheu (Taipei) translated and revised the MUIS in Chinese (14). The content validity index was 0.92, and internal consistency reliability (Cronbach’s α value) was 0.87 (where the uncertainty reliability coefficient was 0.85, and the complexity reliability coefficient was 0.66) (14). Two dimensions were rated in this scale, with 10 questions in the complexity dimension (questions #5, 6, 7, 9, 10, 17, 19, 20, 23, and 25) and 15 questions in the uncertainty dimension (questions #1, 2, 3, 4, 8, 11, 12, 13, 14, 15, 16, 18, 21, 22, and 24). The questions were answered using a 5-point Likert scale, with 1 to 5 points indicating strongly disagree to strongly agree. Questions #6, 7, 9, 23, and 25 were scored in reverse. A participant could score 25–125 points in total on the scale. In the complexity dimension, a participant could score 10–50 points, and in the uncertainty dimension, a participant could score 15–75 points. The total score of illness uncertainty was the sum of the total score in the complexity dimension and the uncertainty dimension. A low score ranged from 25 to 58.3 points, a moderate score ranged from 58.4 to 91.7 points, and a high score ranged from 91.8 to 125 points (15-17).
CSMS
Professor Ren Hongyan of Chongqing Medical University designed the CSMS (18) according to the “three tasks in self-management” put forward by Corbin and Stratus (19). This scale covered seven dimensions: general life management, bad habit management, disease knowledge management, symptom management, first aid management, treatment compliance management, and emotional cognition management, and had 27 questions. Cronbach’s α value was 0.913, indicating good internal consistency reliability and content validity (20). The seven factors extracted by the factor analysis method in this study were in good agreement with the standard dimensions and could cumulatively explain 67.6% of the variation. Except for the question about maintaining daily life routines, all questions had only one common factor. The factor loading for the question on communicating disease information and feelings to others was 0.481, and that for the question about developing life and exercise schedules to fight the disease was 0.418, while the same for all other questions were greater than 0.5 and were of medium to high strength. The correlation analysis showed that the correlation coefficient between the score of each dimension and the total score of the scale was greater than that between different dimensions, indicating a good structural validity. The criterion-related validity of each dimension was tested, and correlation coefficient analyses were conducted. The results showed that the correlation coefficient of the second type was 0.271, indicating a weak correlation, and the same of the other two types were greater than 0.4, meeting the ideal standard and indicating a sound criterion-related validity (21).
The 5-point Likert scale was adopted for scoring, and the options were designed as follows. (I) For questions with strong objectivity and easy to be quantified, including compliance with advice on quitting smoking, compliance with advice on limiting salt intake, compliance with advice on limiting alcohol intake, participation in recommended activities and exercises, recording of angina pectoris attack information (times, degree, and duration of attacks), regular re-examination, and regular inoculation of recommended vaccines, five levels of quantitative sequencing options were designed. (II) For general questions, including compliance with advice on limiting fat and cholesterol intake and consuming a balanced diet, multiple indicators were used for evaluation (13) and then converted into the score of the corresponding question following the 5-level scoring principle. (III) For the other questions, options of “never”, “seldom”, “sometimes”, “often”, and “always” were provided, which were assigned 1, 2, 3, 4, and 5 points, respectively. The sum of the scores of all questions in a dimension was the total score of the dimension, and the sum of scores in all dimensions was the total score on self-management. A higher total score indicated better self-management.
SF-36
The SF-36 Scale in Chinese was translated in 1991 by the Teaching and Research Office of Social Medicine, School of Medicine, Zhejiang University, and was used to evaluate the quality of life of patients with heart stent implantation. The scale was a general maladjustment scale (22) with 36 questions that covered eight dimensions related to health quality evaluation: (I) physical functioning (PF), with 10 questions; (II) role-physical (RP), with four questions; (III) bodily pain (BP), with two questions; (IV) General Health (11), with five questions; (V) validity (VT), with four questions; (VI) social function (SF), with two questions; (VII) role-emotional (RE), with three questions; and (VIII) mental health, with five questions. There was a question about health transition (HT) in the scale that was not scored, but was used to evaluate the patient’s health changes over the past year. When this scale was being scored, the original score value was converted into a percentile score according to the corresponding weight, and such a score indicated the quality of life of a patient (23). The results showed good internal consistency, reliability, and validity (24).
Statistical analysis
The software SPSS 20.0 (IBM Corp., Armonk, NY, USA) was used for data analysis. According to the Kolmogorov-Smirnov test results, the continuous variables that conformed to the normal distribution were presented as mean ± standard deviation and were analyzed using the independent-samples t-test (two-group comparisons) and one-way analysis of variance (ANOVA; multiple groups). Categorical variables were presented as the number of cases (n) and percentage (%). All continuous variables in the correlation analysis conformed to the bivariable normal distribution. Pearson’s bivariable correlation analysis was used to analyze the correlation between illness uncertainty, self-management capability, and quality of life. A multivariable linear regression analysis (enter method) was used to identify the associated factors for illness uncertainty. The indexes with significant statistical differences were included in the univariate analysis, and the stepwise regression method was used to fit the multiple linear regression equation. Two-sided P values ≤0.05 were deemed statistically significant.
Results
Sociodemographic characteristics
A total of 191 questionnaires were distributed, and 168 (87.9%) valid questionnaires were collected. Among the 168 participants, 125 were males (74.4%), and 43 were females (25.6%). The age of the participants was 66.7±10.3 (range, 32 to 88) years. 78 had completed lower than junior high school (46.4%), 37 had completed senior high school (22.0%), 53 had completed higher than junior college (31.5%). Of the participants, 142 were retired (84.5%), 26 were unretired (15.5%). 143 participants were married (85.1%), 25 participants were non-married status (including such as unmarried/divorced/widowed) (14.9%). In terms of the number of heart stents, 100 participants had one stent (59.5%), 48 participants had two stents (28.6%), 18 participants had three stents (10.7%), and 2 had four stents (1.2%). A total of 36 participants thought that they received very great guidance and support from the nurses during hospitalization (21.4%), 67 reported great guidance and support (39.9%), 38 moderate guidance and support (22.6%), and 27 a little or little guidance and support (16.1%). Regarding care and support from children or spouses, 36 participants thought that they received very great care and support (21.4%), 70 received great care and support (41.7%), 30 received some care and support (17.9%), and 32 received little or no care or support (19.0%). Of all participants, 32 were aware of very great improvement in their symptoms (19.0%), 79 were aware of great improvement (47.0%), 22 were aware of some improvement (13.1%), and 35 were aware of little or no improvement (20.8%). A total of 42 participants expressed that they had received very great support from follow-up nurses after discharge (25.0%), 66 received great support (39.3%), 31 received general support (18.5%), and 29 received a little or little support (17.3%). Frequent angina pectoris attacks were reported by 21 participants (12.5%), 46 had occasional angina pectoris attacks (27.4%), and 101 never had angina pectoris attacks (60.1%) (Table 1).
Table 1
| Variable | Total, n (%) | Score on uncertainty in illness (mean ± SD) | P value |
|---|---|---|---|
| Gender | 0.346 | ||
| Male | 125 (74.4) | 79.2±14.3 | |
| Female | 43 (25.6) | 81.6±13.4 | |
| Age (years) | 0.158 | ||
| 18–50 | 9 (5.4) | 87.4±17.9 | |
| 51–70 | 103 (61.3) | 80.2±13.9 | |
| >70 | 56 (33.3) | 78.0±13.6 | |
| Educational background | 0.003 | ||
| Lower than Junior high | 78 (46.4) | 83.5±14.9 | |
| Senior high | 37 (22.0) | 78.9±13.1 | |
| Higher than Junior college | 53 (31.5) | 75.1±12.0 | |
| Retired | 0.035 | ||
| Yes | 142 (84.5) | 78.9±13.5 | |
| No | 26 (15.5) | 85.2±15.8 | |
| Marital status | 0.025 | ||
| Married | 143 (85.1) | 78.8±13.9 | |
| Non-married status | 25 (14.9) | 85.6±13.6 | |
| Number of stents | 0.000 | ||
| 1 | 100 (59.5) | 71.5±8.0 | |
| 2 | 48 (28.6) | 89.2±11.9 | |
| 3 | 18 (10.7) | 98.7±7.6 | |
| 4 | 2 (1.2) | 104.5±9.2 | |
| Guidance and support from nurses during hospitalization | 0.000 | ||
| Very great | 36 (21.4) | 71.2±7.0 | |
| Great | 67 (39.9) | 71.7±7.1 | |
| General | 38 (22.6) | 89.2±13.8 | |
| A little/little | 27 (16.1) | 98.3±7.0 | |
| Care and support from children or spouse | 0.000 | ||
| Very great | 36 (21.4) | 70.3±5.2 | |
| Great | 70 (41.7) | 72.0±8.4 | |
| Some | 30 (17.9) | 89.5±11.5 | |
| Little/no | 32 (19.0) | 98.6±7.4 | |
| Self-awareness of improvement of symptoms | 0.000 | ||
| Very great | 32 (19.0) | 70.1±5.9 | |
| Great | 79 (47.0) | 72.0±7.2 | |
| Some | 22 (13.1) | 93.5±12.8 | |
| Little/no | 35 (20.8) | 97.8±5.9 | |
| Angina pectoris attacks | 0.000 | ||
| Frequent | 21 (12.5) | 97.9±5.0 | |
| Occasional | 46 (27.4) | 90.2±13.7 | |
| Never | 101 (60.1) | 71.4±7.1 | |
| Support from follow-up nurses after discharge | 0.000 | ||
| Very great | 42 (25.0) | 69.3±7.7 | |
| Large | 66 (39.3) | 73.0±5.9 | |
| General | 31 (18.5) | 92.9±13.7 | |
| A little/little | 29 (17.3) | 96.8±6.6 | |
P≤0.05 were deemed statistically significant. SD, standard deviation.
Scores of illness uncertainty
The average score of illness uncertainty was 79.8±14.1 points, which was of a moderate level. High scores on uncertainty in illness were achieved by 32.7% of participants. The average score in the uncertainty dimension was 39.8±11.1 points, and that in the complexity dimension was 40.0±4.7 points, both of a low level (Table 2). According to Table 1, participants who had completed lower levels of education had higher uncertainty; participants that had retired; participants that had married; participants with fewer heart stents and angina pectoris attacks, more care and support from children or spouses, and awareness of greater improvement of symptoms had lower uncertainty; participants receiving more guidance from nurses during hospitalization or more support from follow-up nurses after discharge had lower uncertainty (all P<0.05) (Table 1).
Table 2
| Item | Score, mean ± SD | Average score on the questions, mean ± SD | Low level, n (%) | Medium level, n (%) | High level, n (%) |
|---|---|---|---|---|---|
| Total score on uncertainty in illness | 79.8±14.1 | 2.9±0.5 | 4 (2.4) | 109 (64.9) | 55 (32.7) |
| Uncertainty | 39.8±11.1 | 2.5±0.7 | 160 (95.2) | 8 (4.8) | – |
| Complexity | 40.0±4.7 | 3.3±0.4 | 168 (100.0) | – | – |
SD, standard deviation.
Correlation between illness uncertainty and self-management capability
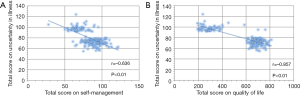
In participants with heart stent implantation, the illness uncertainty and self-management capability were negatively correlated (r=−0.636, P<0.01), namely, better self-management resulted in lower uncertainty. In particular, the illness uncertainty was most strongly correlated with the dimension of disease knowledge management (r=−0.684, P<0.01) (Table 3, Figure 1).
Table 3
| Item | Total scores | Correlation analysis (r value) | ||
|---|---|---|---|---|
| Total score on uncertainty in illness | Uncertainty | Complexity | ||
| Total score on self-management | 13,955 | −0.636** | −0.641** | −0.388** |
| Bad habit management | 2,249 | −0.407** | −0.405** | −0.262** |
| Symptom management | 1,828 | −0.486** | −0.469** | −0.347** |
| Emotional cognition management | 2,321 | −0.249** | −0.299** | −0.039 |
| First aid management | 1,560 | −0.391** | −0.382** | −0.267** |
| Disease knowledge management | 2,451 | −0.684** | −0.650** | −0.511** |
| General life management | 2,489 | −0.171* | −0.210** | −0.015 |
| Treatment compliance management | 1,057 | −0.111 | −0.175* | 0.081 |
*, P<0.05; **, P<0.01. P≤0.05 were deemed statistically significant.
Correlation between illness uncertainty and quality of life
In patients with heart stent implantation, illness uncertainty and quality of life were negatively correlated (r=−0.857, P<0.01), namely, a better quality of life was associated with lower uncertainty. Illness uncertainty was most strongly correlated with the dimension of health transition (Table 4, Figure 1).
Table 4
| Item | Total scores | Correlation analysis (r value) | ||
|---|---|---|---|---|
| Total score on uncertainty in illness | Uncertainty | Complexity | ||
| Total score on quality of life | 95,691.50 | −0.857** | −0.826** | −0.612** |
| Physical functioning | 8,285 | −0.741** | −0.704** | −0.554** |
| Role physical | 9,950 | −0.711** | −0.689** | −0.500** |
| Bodily pain | 10,350 | −0.678** | −0.673** | −0.439** |
| General health | 11,515 | −0.756** | −0.720** | −0.562** |
| Validity | 11,735 | −0.735** | −0.713** | −0.514** |
| Social function | 10,675 | −0.730** | −0.715** | −0.495** |
| Role emotional | 10,367.50 | −0.673** | −0.630** | −0.527** |
| Mental health | 10,564 | −0.745** | −0.706** | −0.561** |
| Health transition | 12,250 | −0.789** | −0.771** | −0.540** |
**, P<0.01. P≤0.05 were deemed statistically significant.
Associated factors for illness uncertainty
The Linear regression analysis results showed that self-awareness of improvement of symptoms [beta: 0.204 (1.128 to 4.499), P=0.001], support from follow-up nurses after discharge [beta: 0.204 (1.271 to 4.306), P=0.000], any degree of care and support from children or spouse [beta: 0.23 (1.639 to 4.704), P=0.000], number of stents [beta: 0.205 (1.908 to 5.955), P=0.000], guidance and support from nurses during hospitalization [beta: 0.181 (1.126 to 4.021), P=0.001] were protecting factors against illness uncertainty and educational background [beta: −0.08 (−2.457 to −0.128), P=0.03] were risk factors for illness uncertainty (Table 5).
Table 5
| Independent variable | Partial regression coefficient, B (95.0% CI) | Std. error | Standardized coefficients, beta | t | Sig. | Collinearity statistics | |
|---|---|---|---|---|---|---|---|
| Tolerance | VIF | ||||||
| Constant | 49.756 (45.828 to 53.684) | 1.989 | – | 25.014 | 0.000 | – | – |
| Self-awareness of improvement of symptoms | 2.814 (1.128 to 4.499) | 0.853 | 0.204 | 3.297 | 0.001 | 0.334 | 2.99 |
| Support from follow-up nurses after discharge | 2.788 (1.271 to 4.306) | 0.769 | 0.204 | 3.628 | 0.000 | 0.405 | 2.471 |
| Care and support from children or spouse | 3.172 (1.639 to 4.704) | 0.776 | 0.23 | 4.088 | 0.000 | 0.401 | 2.491 |
| Number of stents | 3.932 (1.908 to 5.955) | 1.025 | 0.205 | 3.837 | 0.000 | 0.446 | 2.242 |
| Guidance and support from nurses during hospitalization | 2.574 (1.126 to 4.021) | 0.733 | 0.181 | 3.511 | 0.001 | 0.479 | 2.088 |
| Educational background | −1.293 (−2.457 to −0.128) | 0.59 | -0.08 | −2.192 | 0.03 | 0.949 | 1.053 |
Std, standard deviation; Std. error, standard error; Sig, significance; VIF, variance inflation factor; B, regression coefficient.
Discussion
Analysis of the current situation and causes of uncertainty of disease in patients with cardiac stent implantation
In this study, the average score of the disease uncertainty in patients after a PCI was 79.83±14.05, it was generally at a moderate level (Table 2); more than one third of the patients were in a state of high uncertainty, which is consistent with the findings of multiple studies (25-28). The main sources of disease uncertainty among patients are as follows. (I) The patient is unfamiliar with the surgical process of coronary angiography and does not understand the principle of PCI in comparison to coronary angiography; therefore, many concerns exist about the prognosis of the disease. (II) The patient is not mentally prepared for the disease and lacks an understanding of his/her own disease. Some patients may still experience precordial fullness and pain in the surgical site after PCI, which increases the patient’s anxiety and worries about surgical efficacy. (III) The relative information on most questions can only be obtained through television, newspapers, the internet, and other media, sources which lack professionalism and accuracy, and lack access to reliable medical information and can lead to an unclear understanding of the development and prognosis of the disease. (IV) Some patients cannot get help from family support in time, lack of follow-up by specialist nurses after discharge; therefore, their questions cannot be readily solved or answered when their condition changes. (V) Postoperative patients are limited in their daily physical activities (such as no smoking, control of high-fat diet and regular exercise) and are forced to change their habits, which increases a sense of uncertainty. It is suggested that symptoms management, follow-up and health education to postpone the development of disease may be useful measures to alleviate the illness uncertainty of the patients.
Coronary heart disease self-management and disease uncertainty
It can be seen from Table 3 that there is a moderate negative correlation between uncertainty and self-management ability in patients with coronary heart disease (r=−0.636), that is, the stronger the self-management ability, the smaller the uncertainty. This is consistent with related research (29). In this study, the higher the level of coronary heart disease self-management ability, the lower the disease uncertainty score, and the patients with high self-management ability may have sufficient confidence in symptom management. Although coronary heart disease cannot be cured, it can be controlled by controlling the inducing factors, regular exercise and healthy diet adjustments, regular physical examinations, and adjustment of medication are related to slowing down the progression of the disease. This study also found that among all dimensions, the dimension of disease knowledge management was the most important, and it had the strongest correlation with the total score of uncertainty, ambiguity, and complexity, all of which were moderately negatively correlated (P<0.05). This shows that a healthy lifestyle and good self-management after surgery are very important, but because patients lack disease-related knowledge, lack of awareness of the disease, and uncertainty about the treatment plan, it is easy to have a sense of uncertainty about the disease. In this study, the more knowledge the patient has about coronary heart disease, the more the patient understands the necessity of the diagnosis and treatment procedures during hospitalization, and the necessity of monitoring the heart and collecting various specimens. Various auxiliary examinations of the heart are the basic basis for treatment and medication. ECG monitoring can dynamically observe the changes of vital signs during coronary heart disease attack, know the importance of outpatient follow-up, actively learn self-help during angina pectoris attack, and the more complex information the patient has in diagnosis and treatment, the lower the uncertainty score; on the contrary, patients lack the above-mentioned knowledge of coronary heart disease. Some patients have poor compliance with smoking, blood lipid control, and long-term medication during the treatment and rehabilitation process. When encountering sudden changes in the condition, self-response measures are ineffective, and the sense of uncertainty increases. This suggests that medical staff should strengthen the health education of patients with coronary heart disease, use easy-to-understand language combined with multimedia or pictures to enhance patients’ understanding of health information, make up for their lack of disease knowledge, and improve self-management level of patients.
Quality of life and disease uncertainty
In this study, it was found that the uncertainty of disease and the quality of life in patients with cardiac stent implantation were highly negative (r=−0.857, P<0.01), as shown in Table 4, that is, the better the quality of life, the smaller the uncertainty, which is related to Relevant studies (30,31) confirmed the consistent results obtained. This study also found that unpredictability in the sense of disease uncertainty was highly negatively correlated with quality of life (r=−0.826, P<0.01), that is, unpredictable intensity, nature, duration, etc. of angina pectoris and unpredictable disease prognosis and stenting. The higher the degree of restenosis, the worse the quality of life of the patients. Among them, the health change dimension has the strongest correlation with the total score of uncertainty and uncertainty, which are all negatively correlated (r=−0.789, P<0.01). This may be related to the fear of symptoms such as pain, suffocation, and a sense of impending death that accompany the onset of the disease in patients undergoing PCI for coronary heart disease, inability to understand the complex treatment and care during hospitalization, and failure to follow a healthy lifestyle. Repeated attacks of angina pectoris, in-stent restenosis or coronary artery blockage due to irregular medication, and lack of self-rescue methods for angina pectoris make the patient unable to maintain a healthy state, thus unable to form a correct cognitive framework for his disease, leading to a sense of uncertainty production. Therefore, in the process of caring for patients with coronary heart disease, nurses should pay special attention to changes in healthy behaviors, teach them self-help, regular follow-up, and correct and scientific healthy behaviors such as diet, smoking cessation, medication, exercise, etc., to help them face the life, establish and strengthen the confidence to overcome the disease, so as to improve the quality of life.
Factors influencing the sense of uncertainty about disease
As can be seen from Table 5, the results of stepwise linear regression analysis showed that the improvement of subjective symptoms, the support of follow-up nurses after discharge, the care and support of family members after discharge, the number of stents, whether there was guidance and support from nurses during hospitalization, and the educational level were selected for the model. And the P value is less than 0.05, which has a significant impact on the total score of uncertainty. Among them, the level of social support (such as the care and support of family members, the guidance of nurses during hospitalization and after discharge) affects the uncertainty of illness, and the relationship between the two also supports Mishel’s theory of illness uncertainty. Social support can directly or indirectly affect the feeling of uncertainty. The uncertainty of the disease may be related to the fact that patients with a high level of social support can obtain more information. Such patients have a higher degree of understanding of the disease. Clinical attention should be paid to the degree of social support of the patient, and targeted information support should be given to understand the disease. Information needs of the disease (32), strengthen health education, help patients understand the occurrence, development, diagnosis and treatment process and prognosis of the disease, reduce the degree of lack of information, and reduce the uncertainty of the disease (33). Support from medical staff is an important resource who will give direct guidance to patients with chronic diseases during their hospitalization (34). Most of participants get knowledge form their medical staff through various forms to improve their ability of self-care ability (35). Secondly, coronary heart disease patients with higher education level have higher thirst for knowledge, and have wider access to health information. They can obtain the information they need through the Internet or others, and can better and comprehensively understand the obtained information, to form a systematic and correct understanding of their own diseases, so patients with high education level are more willing to adopt healthy behaviors, and they are confident that they can control the development of the disease, which is conducive to self-management, thereby reducing the uncertainty of the disease. Relevant study (7) show that health education can improve the self-management level of patients with low education level, and their quality of life can be significantly improved, thereby reducing the uncertainty of the disease. Furthermore, the degree of improvement of subjective symptoms and the number of stents affect the illness uncertainty. Patients have little knowledge about the surgical procedure of coronary angiography and the principles of stent implantation for coronary artery disease. Some patients may still experience precordial pain after surgery, the subjective symptoms did not improve, and then there were doubts about the treatment effect, resulting in increased illness uncertainty. Therefore, the responsible nurse should fully inform the patient of the possible conditions when implementing the perioperative education, especially for the patients with multiple stents implanted, should strengthen the postoperative inspection, and promptly communicate the patient’s condition with the treating physician if any abnormality is found, to be a good transmitter of effective communication between doctors and patients.
Conclusions
Illness uncertainty after cardiac stent implantation, degree of subjective symptom improvement, support from follow-up nurses after discharge, care and support from family members after discharge, number of stents, presence or absence of nurse guidance and support during hospitalization, and level of education were factors influencing disease uncertainty in patients with cardiac stent implantation. This study demonstrated that self-management and quality of life in patients with coronary heart disease were inversely related to the uncertainty of disease in patients after stenting. Therefore, for patients with coronary heart disease after PCI (especially patients with a large number of stents), family members should give adequate care; doctors and nurses should provide adequate health education to patients to help patients establish healthy behavior habits and enhance their self-esteem management ability, thereby reducing patient uncertainty, thereby improving the long-term prognosis of PCI and improving the patient’s quality of life. This study has several limitations, and due to the cross-sectional study design, the dynamics of disease uncertainty and its long-term effects on patients were not followed up. Follow-up studies will design longitudinal cohorts to explore the trajectory of postoperative patient uncertainty and the effectiveness of corresponding nursing interventions. Second, this study lacks the uncertainty assessment of the patient’s family: as the clinical practice model shifts from patient-centered care to family-centered care, we should focus on the communities formed by critically ill patients and their families, who are social main source. Support for patients can provide not only day-to-day assistance, but even nursing roles, provide transportation between home and hospital, and help manage symptoms and medication side effects (36). Our future work will expand the application of MUIS to assess the uncertainty of patients’ family members, and reduce illness uncertainty in coronary heart disease patients with heart stent implantation by guiding supportive communication between patients and their family members, joint problem solving and emotion-centered coping strategies.
Acknowledgments
Funding: This study was supported by a grant from the general project from the Fuxing Nursing Researching Program of Fudan University (No. FNF201943).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-528/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-528/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-528/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Huadong Hospital (No. 20200082). The participants and their family members were informed of the study’s objective and were ensured of the principles of confidentiality and voluntariness. Written informed consent was provided by the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mishel MH, Braden CJ. Finding meaning: antecedents of uncertainty in illness. Nurs Res 1988;37:98-103, 127. [Crossref] [PubMed]
- Anema C, Johnson M, Zeller JM, et al. Spiritual well-being in individuals with fibromyalgia syndrome: relationships with symptom pattern variability, uncertainty, and psychosocial adaptation. Res Theory Nurs Pract 2009;23:8-22. [Crossref] [PubMed]
- Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina and Caucasian breast cancer survivors: a comparative study. Oncol Nurs Forum 2010;37:93-9. [Crossref] [PubMed]
- Bailey DE Jr, Landerman L, Barroso J, et al. Uncertainty, symptoms, and quality of life in persons with chronic hepatitis C. Psychosomatics 2009;50:138-46. [Crossref] [PubMed]
- Chung ML, Moser DK, Lennie TA, et al. Perceived social support predicted quality of life in patients with heart failure, but the effect is mediated by depressive symptoms. Qual Life Res 2013;22:1555-63. [Crossref] [PubMed]
- Papadopoulou C, Kotronoulas G, Schneider A, et al. Patient-Reported Self-Efficacy, Anxiety, and Health-Related Quality of Life During Chemotherapy: Results From a Longitudinal Study. Oncol Nurs Forum 2017;44:127-36. [Crossref] [PubMed]
- Zahodne LB, Nowinski CJ, Gershon RC, et al. Self-Efficacy Buffers the Relationship between Educational Disadvantage and Executive Functioning. J Int Neuropsychol Soc 2015;21:297-304. [Crossref] [PubMed]
- Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch 1990;22:256-62. [Crossref] [PubMed]
- Watkins LL, Blumenthal JA, Davidson JR, et al. Phobic anxiety, depression, and risk of ventricular arrhythmias in patients with coronary heart disease. Psychosom Med 2006;68:651-6. [Crossref] [PubMed]
- Watkins LL, Blumenthal JA, Carney RM. Association of anxiety with baroreflex cardiac control in patients after acute myocardial infarction. Am Heart J 2002;143:460-6. [Crossref] [PubMed]
- Anderson JL, Adams CD, Antman EM, et al. Guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction. J Am Coll Cardiol 2007;50:e1-e157. [Crossref] [PubMed]
- King SB III, Smith SC Jr, Hirshfeld JW Jr, et al. 2007 Focused update of the ACC/AHA/SCAI 2005 Guideline update for percutaneous coronary intervention. Circulation 2008;117:261-95. [Crossref] [PubMed]
- Moreland P, Santacroce SJ. Illness Uncertainty and Posttraumatic Stress in Young Adults With Congenital Heart Disease. J Cardiovasc Nurs 2018;33:356-62. [Crossref] [PubMed]
- Sheu S, Hwang SL. Validation of Chinese Version of Mishel’s Uncertainty in Illness Scale. Nurs Res (Taiwan) 1996;4:59-68.
- Mishel MH. Parents’ perception of uncertainty concerning their hospitalized child. Nurs Res 1983;32:324-30. [Crossref] [PubMed]
- Landis BJ. Uncertainty, spiritual well-being, and psychosocial adjustment to chronic illness. Issues Ment Health Nurs 1996;17:217-31. [Crossref] [PubMed]
- Gold-Spink Esher TG, Theodos V. Uncertainty in Illness and Optimism in Couples With Multiple Sclerosis. Int J Rehab Health 2000;5:157-64. [Crossref]
- Ren HY, Ping T, Zhao QH. Development and evaluation of coronary artery disease self-management scale. Journal of Army Medical University 2009;31:1087-90.
- Zheng SJ, Cheng SZ, Jiang Y. associated factors for diet and lifestyle compliance of patients with type-2 diabetes. Chin J Behav Med Sci 2007;16:401-3.
- Pullen C, Walker SN, Fiandt K. Determinants of health-promoting lifestyle behaviors in rural older women. Fam Community Health 2001;24:49-72. [Crossref] [PubMed]
- Zhang YY. The role of nurses in secondary prevention of coronary heart disease. Mol Cardiol China 2005;5:795-7.
- The World Health Organization Quality of Life Assessment (WHOQOL). development and general psychometric properties. Soc Sci Med 1998;46:1569-85. [Crossref] [PubMed]
- Sammarco A, Konecny LM. Quality of life, social support, and uncertainty among Latina breast cancer survivors. Oncol Nurs Forum 2008;35:844-9. [Crossref] [PubMed]
- Eastwood JA, Doering L, Roper J, et al. Uncertainty and health-related quality of life 1 year after coronary angiography. Am J Crit Care 2008;17:232-42; quiz 243. [Crossref] [PubMed]
- Schiele SE, Emery CF, Jackson JL. The role of illness uncertainty in the relationship between disease knowledge and patient-reported outcomes among adolescents and adults with congenital heart disease. Heart Lung 2019;48:325-30. [Crossref] [PubMed]
- Wei X, Zhou L, Zheng X, et al. Status and associated factors of Uncertainty in Illness in Patients with Cardiac Surgery. Genomics and Applied Biology 2019;38:4208-12.
- Kim O, Yeom EY, Jeon HO. Relationships between depression, family function, physical symptoms, and illness uncertainty in female patients with chronic kidney disease. Nurs Health Sci 2020;22:548-56. [Crossref] [PubMed]
- Ding D, Huang J, Westra J, et al. Immediate post-procedural functional assessment of percutaneous coronary intervention: current evidence and future directions. Eur Heart J 2021;42:2695-707. [Crossref] [PubMed]
- Zhang Y, Kwekkeboom K, Petrini M. Uncertainty, Self-efficacy, and Self-care Behavior in Patients With Breast Cancer Undergoing Chemotherapy in China. Cancer Nurs 2015;38:E19-26. [Crossref] [PubMed]
- McCormick KM. A concept analysis of uncertainty in illness. J Nurs Scholarsh 2002;34:127-31. [Crossref] [PubMed]
- Meredith Wallace Uncertainty and Quality of life of older Men who undergo waiting for prostate cancer. Prostate Cancer 2003;30:303-9.
- Kasteleyn MJ, Gorter KJ, van Puffelen AL, et al. What follow-up care and self-management support do patients with type 2 diabetes want after their first acute coronary event? A qualitative study. Prim Care Diabetes 2014;8:195-206. [Crossref] [PubMed]
- Zhao S, Zhao H, Wang L, et al. Education is critical for medication adherence in patients with coronary heart disease. Acta Cardiol 2015;70:197-204. [Crossref] [PubMed]
- Cao L, Liu J, Hao L. Effects of chronic disease resource utilization on medication compliance of elderly patients with essential hypertension in Jiaozuo region. General Nursing 2018;16:912-5.
- Ning Y, Wan Z, Hou F, et al. Research progress of disease uncertainty in patients with coronary heart disease. Journal of Nursing Advancement 2015;30:230-3.
- Pan J, Fu X, Luo Y. Study on correlation between uncertainty in illness and patients’ quality of life for family of patients with chronic heart failure. Nursing and Rehabilitation Journal 2020;19:10-4.
(English Language Editor: J. Jones)


