
Effect of personalized nursing based on quantitative evaluation strategies on remission of first-episode schizophrenia comparing to usual care: a systematic review and meta-analysis
Introduction
Schizophrenia is a common serious psychiatric disease in clinical practice. During an attack of this disease, a patient’s personal sensations, perceptions, emotions, and behaviors are abnormal. Some patients experience hallucinations and cannot distinguish between hallucinations and reality. Patients may be sluggish, withdraw, display excessive behavioral reactions, find it difficult to maintain normal social contacts, and have their quality of life seriously reduced, and both patients and their families are greatly affected (1,2).
According to statistics, about 23 million patients have been diagnosed with schizophrenia worldwide, and its lifetime prevalence is about 3.8–8.4% (3). In Asian populations, the disorder accounts for approximately 50% of all psychiatric disorders (4). The disease is characterized by repeated course migration, complex and variable symptoms, and high recurrence and disability rates (5). The drug control of symptoms is the main clinical treatment (5). Drug treatment has a good effect on positive symptoms, such as delusions and hallucinations, but its effect on negative symptoms, such as withdrawal and apathy, is limited. During the treatment, patients’ social skills are poor, treatment compliance is poor, and self-management ability is poor too, all are the factors which could affects the drug treatment (6). Also, the detachment of patients’ mental activity from reality and patients’ tendency to violence are also major problems in nursing that causing nursing difficulties (6).
Quantitative evaluation and personalized nursing are two important areas in the field of nursing. Quantitative evaluation can digitize the patient’s condition, rehabilitation status and other contents, while personalized nursing emphasizes the discovery of patients’ different nursing needs and the formulation of differentiated schemes. The nursing model of the combination of the two has been gradually applied in different fields, and its application in psychiatry is also gradually being discussed (7). However, there are controversies in the reports of the effects of this care model among studies. In the controlled clinical studies implemented by Wang et al. (8) and Jiang et al. (9), the total Positive and Negative Syndrome Scale (PANSS) score of patients after personalized care under a quantitative evaluation strategy was significantly lower than usual care. However, in another study by Li et al. (10), there was no significant difference between the reduced value of PANSS score after nursing comparing to the usual care. Thus, we conducted a combined meta-analysis to resolve the controversies and examine the significance of personalized nursing care with quantitative evaluation strategies in the treatment of schizophrenia. We present the following article in accordance with the PRISMA reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-605/rc).
Methods
Inclusion of studies
We determined inclusion criteria based on the Participants, Interventions, Comparisons, Outcomes, and Study (PICOS) framework (11). All the subjects in all the studies were patients with confirmed first-episode schizophrenia. The studies were all randomized controlled trials (RCTs), non-RCTs (e.g., cohort, case-control, cross-sectional, and heterogeneity studies) were excluded. The patients were randomly divided into the following 2 groups: (I) the experimental group; and (II) the control group. There was no significant difference in the baseline data between the 2 groups, and the same drug intervention and treatment were administered. However, the nursing methods administered to the 2 groups differed. The control group received routine nursing care, while the experimental group received personalized nursing with a quantitative evaluation strategy.
The nursing methods for the experimental group comprised the following 2 aspects: (I) a “quantitative evaluation strategy”; and (II) “personalized nursing”. Under the quantitative evaluation strategy, a scale or method was used for enrollment, and the disease severity of each patient was scored, quantified, and graded according to the quantitative results. The PANSS is a common quantification method. Under the PANSS, patients with a score of >120 points are assessed as having severe symptoms, patients with a score of 80–120 points are assessed as having moderate symptoms, patients with a score of 60–80 points are assessed as having mild symptoms, and patients with a score of <60 points are assessed as having no obvious schizophrenic symptoms. Under the personalized nursing approach, different nursing methods are applied to patients depending on the severity grade (e.g., for severe patients, the nurse-patient ratio is increased, the frequency of the hospitalization patrol is increased, and an enhanced version of health education and rehabilitation training is adopted).
Literature search strategy
We used the mainstream medical databases of PubMed, Medline, Embase, China National Knowledge Infrastructure (CNKI), and Wanfang as the literature sources. The search period included articles published from the establishment of the databases to January 2022, and different search strategies were adopted for different databases. For example, for the PubMed database, the following search method was adopted:
- Search quantitative evaluation strategy [Title/Abstract] OR schizophrenia [Title/Abstract]
- Search rating [Title/Abstract] OR schizophrenia [Title/Abstract]
- Search personalized nursing [Title/Abstract] OR schizophrenia [Title/Abstract]
- Search individualized nursing [Title/Abstract] OR schizophrenia [Title/Abstract]
- Search #1 OR #2 OR #3 OR #4
- Search (schizophrenia [MeSH Terms]) OR nursing [Title/Abstract].
Literature selection and data extraction
Next, 2 researchers worked together to screen the articles according to the inclusion criteria. After finalizing the included articles, the full text of each article was obtained and read, and the required data were extracted, and recorded in a table. The extracted data included the (I) the baseline data of the included patients, including the gender composition ratio (%), age composition ratio (%), initial PANSS score (mean ± variance), education level (%), residence, and family psychiatric history; and (II) the publication data, including the journal name, first author name, and region; and (III) the outcome data.
Outcome indicators
Due to the different outcome indicators reported in each article, we could not perform a meta-analysis for all of the outcome indicators; thus, only the following 4 most common indicators were analyzed: (I) PANSS score after nursing (the scores measured by the PANSS were divided into a positive symptom score, a negative symptom score, and a general psychotic symptom score, we only counted the total scores of the 3 aspects); (II) treatment compliance rate. (Patient compliance was assessed subjectively or objectively. Under the subjective method, the medical staff subjectively assessed the patients. Under the objective method, the patients were assessed using a scale); (III) quality of life after nursing. Each study used different scales to assess patients’ quality of life after care. Quality of life can be divided into material life, physical health, mental health, and social function, but we only analyzed patients’ physical health scores; and (IV) social function after nursing {the social dysfunction scale [Social Disability Screening Schedule (SDSS)] score after nursing was used} (12).
Literature quality assessment and risk of bias
The Cochrane risk of bias 2.0 tool (13) was used to assess the risk of bias for the included studies. The risk of bias tool comprises 6 separate aspects, each judged by 3 levels of risk of bias, which are “low risk”, “some concern of risk”, and “high risk”.
Statistical methods
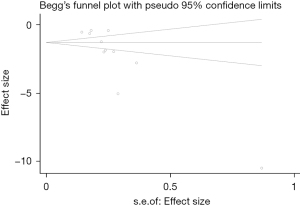
The I2 test and Q test were used to analyze the heterogeneity among the different studies. An I2 value <50% or a P value ≥0.1 indicated no statistically significant heterogeneity; the PANSS score and SDSS score were continuous variables, and the mean difference (MD) and 95% confidence interval (CI) were used as the effect sizes; the odds ratio (OR) effect size was used for the dichotomous categorical variable of treatment compliance, and the 95% CI was used as the CI; due to the use of different scales of life treatment in each article, we used the standard mean difference (SMD) and 95% CI as effect sizes. If there was no statistically significant heterogeneity in the articles, the fixed-effects model was adopted. Conversely, if there was statistically significant heterogeneity in the articles, the random-effects model was adopted. The forest plot shows the merging process of the effect size; the heterogeneity source was investigated by a subgroup analysis and a meta-regression analysis. A sensitivity analysis was performed using the one-by-one exclusion method. Publication bias was quantitatively determined by Begg’s test. P value <0.05 bilaterally could be considered statistically significant.
Results
Literature screening process and results
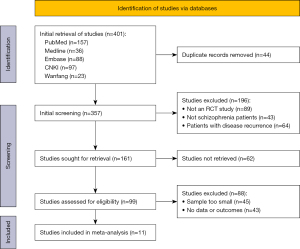
Initially, we retrieved 401 articles, but ultimately only 11 articles were included in the meta-analysis (8,9,14-22). Figure 1 shows the selection flow chart.
Basic characteristics of literatures
A total of 1,251 patients with schizophrenia were included in this study. All of the studies were RCTs, the subjects of 4 studies were children (aged <18 years) (8,14-16) and the subjects of the remaining 7 studies were adults. A total of 4 studies (16,17,20,21) included patients with an average baseline PANSS score <80, and the remaining 7 studies included patients with an average baseline PANSS scores ≥80. A total of 6 studies (8,9,14-16,18) assessed patients’ disease severity using the PANSS, and the remaining 5 studies were assessed by other means (see Table 1).
Table 1
| First author, year | Type of study | Control group | Experimental group | Population (E/C) | Baseline PANSS total score () | Method for quantifying disease severity | Outcome indicators | |||
|---|---|---|---|---|---|---|---|---|---|---|
| M/F | Age (y, ) | M/F | Age (y, ) | |||||||
| Wang et al. 2018 (8) | RCT | 27/13 | 10.29±1.42 | 24/16 | 10.84±1.24 | 40/40 | 94.68±8.12 | PANSS | (a)(b)(c) | |
| Jiang et al. 2020 (9) | RCT | 30/25 | 44.4±4.0 | 29/26 | 43.2±6.2 | 55/55 | 94.02±5.12 | PANSS | (a)(b)(d) | |
| Ye et al. 2021 (14) | RCT | 19/21 | 15.85±1.68 | 18/22 | 15.76±1.70 | 40/40 | 93.25±5.08 | PANSS | (a)(b)(c) | |
| Shao et al. 2021 (15) | RCT | 17/13 | 13.88±1.92 | 16/14 | 13.92±1.80 | 30/30 | 92.14±3.27 | PANSS | (a)(b)(c) | |
| Qin et al. 2021 (16) | RCT | 63/37 | 10.9±1.8 | 60/40 | 9.1±1.1 | 100/100 | 77.25±3.14 | PANSS | (a)(c)(d)(e) | |
| Chen et al. 2021 (17) | RCT | 16/32 | 55.67±5. 47 | 18/30 | 56. 59±5.53 | 48/48 | 66.89±6.24 | CGI-SI | (a)(c)(d)(e)(f)(g) | |
| Shimada et al. 2018 (18) | RCT | 33/35 | 41.39±11.04 | 34/34 | 43.34±9.97 | 68/68 | 108.53±20.33 | PANSS | (a) | |
| Gu et al. 2014 (19) | RCT | 15/18 | 23.39±10.34 | 14/18 | 24.03±8.24 | 32/33 | 82.82±9.54 | PSP | (a) | |
| He et al. 2017 (20) | RCT | 34/28 | 39.62±7.68 | 33/29 | 40.16±7.63 | 62/62 | 58.69±8.66 | HAD | (a)(c)(f) | |
| Xu et al. 2016 (21) | RCT | 50/50 | 32.66±10.58 | 50/50 | 32.85±11.16 | 100/100 | 59.04±7.33 | BPRS | (a) | |
| Chen et al. 2019 (22) | RCT | 25/25 | 34.75±9.82 | 25/25 | 35.82±10.93 | 50/50 | 93.42±3.66 | BPRS | (a) | |
(a) PANSS total score; (b) treatment compliance rate; (c) quality of life; (d) SDSS score; (e) the SSMIS score; (f) the MRSS score; (g) recurrence rate. M/F, male/female; E/C, experimental/control; PANSS, Positive and Negative Syndrome Scale; CGI-SI, Clinical Global Impression-Severity of illness; PSP, Personal and Social Performance Scale; HAD, Hospital Anxiety and Depression Scale; BPRS, brief psychiatric rating scale; SDSS, Social Disability Screening Schedule; SSMIS, schizophrenia self-management instrument scale; MRSS, morning side rehabilitation status scale.
Quality assessment of literature
The overall quality of the 11 studies included in this meta-analysis was good. In relation to the risk of bias, 1 article (16) had a “low” risk of bias, and the other articles had “some concern of risk”; none of the articles had a “high” risk of bias (see Figures 2,3).
Meta-analysis results
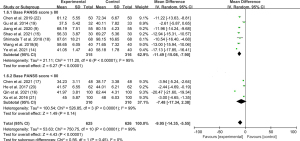
PANSS total score after nursing
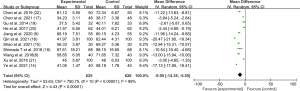
All of the 11 articles compared the average PANSS scores of patients before and after nursing. There was no statistically significant difference in the PANSS scores between the 2 groups before nursing in the reports of all the 11 studies. As the meta-analysis revealed that there was statistical heterogeneity between the articles comparing the PANSS scores after nursing (I2=99%, P<0.00001), the random-effects model was used. The results of the pooled analysis showed that patients who received personalized nursing with a quantitative evaluation strategy had a significantly lower total PANSS score after nursing than patients who received routine nursing (MD =−9.95, 95% CI: −14.35, −5.55; P<0.00001; see Figure 4).
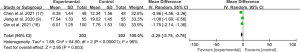
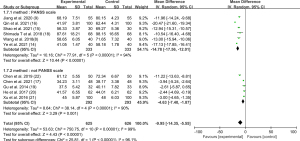
Treatment compliance rate after nursing
Only 4 articles (8,9,14,15) examined the treatment compliance rate of patients. As there was no statistical heterogeneity among the articles (I2=0%, P=0.89), the fixed-effects model was used to pool the data of the studies. Patients who received personalized nursing with a quantitative evaluation strategy had a significantly higher treatment compliance rate than patients who received routine nursing care (OR =4.44, 95% CI: 2.17, 9.09, P<0.0001; see Figure 5).
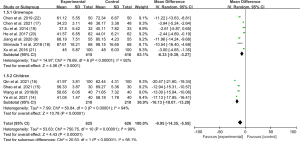
Quality of life after nursing
Only 6 articles (8,14-17,20) examined quality of life indicators after nursing. As there was statistical heterogeneity among the articles (I2=95%, P<0.00001), the random-effects model was used to pool the data. Patients who received personalized nursing with a quantitative evaluation strategy had a significantly higher quality of life after nursing than patients who received routine nursing (SMD =2.40, 95% CI: 1.46, 3.34, P<0.00001; see Figure 6).
SDSS score after nursing
Only 3 articles (9,16,17) reported SDSS scores. As there was statistical heterogeneity between the articles (I2=96%, P<0.00001), the random-effects model was used to pool the data. The patients who received personalized nursing with a quantitative evaluation strategy had significantly lower SDSS scores after nursing than those who received routine nursing (MD =−2.25, 95% CI: −3.75, −0.76; P=0.003; see Figure 7).
Subgroup analysis and regression analysis
Grouping by age
The 11 articles were divided into “children” and “adult” groups according to whether the study subjects were adults or children. For the subgroup analysis of the pooled effect size of PANSS total scores after nursing, there was still heterogeneity among the 2 subgroups, indicating that age was not the source of heterogeneity (see Figure 8).
Grouping by initial PANSS scores
The 11 articles were divided into “≥80” and “<80” groups according to the PANSS baseline score at enrollment. For the subgroup analysis of the PANSS total scores after nursing, there was still heterogeneity in the 2 subgroups, indicating that the initial PANSS of patients was not the source of heterogeneity (see Figure 9).
Grouping by quantification of disease severity
The 11 articles were divided into “PANSS assessment” and “non-PANSS assessment” groups according to the quantitative method used to determine disease severity at enrollment. For the subgroup analysis of the pooled effect size of the PANSS total scores after nursing, there was still heterogeneity in the 2 subgroups, indicating that the use of the PANSS to assess the disease severity of patients was not the source of heterogeneity (see Figure 10).
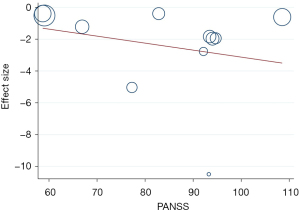
Quantitative regression analysis
A meta-regression was used to replace the quantitative methods of patient age, initial PANSS score, and disease severity into the regression equation. The P values of the 3 factors were all >0.05, indicating that none of these 3 factors was a statistically significant factor affecting the results of the meta-analysis (see Table 2). The bubble plots with age and initial PANSS score in abscissa are shown in Figures 11,12.
Table 2
| Covariate | β | Std. Err. | t | P>|t| | 95% CI |
|---|---|---|---|---|---|
| PANSS | 0.0235068 | 0.0740221 | 0.32 | 0.760 | −0.1515275 to 0.1985412 |
| Age | 0.0599563 | 0. 0662756 | 0.90 | 0.396 | −0.0967606 to 0.2166731 |
| Scale | −2.479465 | 2.572058 | −0.96 | 0.367 | −8.561415 to 03.602485 |
| _Cons | −4.790085 | 5.714544 | −0.84 | 0.430 | −18.30284 to 8.722665 |
PANSS, Positive and Negative Syndrome Scale.
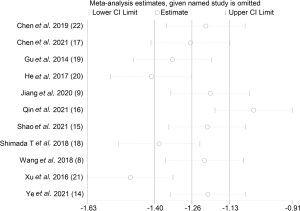
Sensitivity analyses
Our sensitivity analysis of the PANSS total scores after care in both groups (see Figure 13) revealed that the results of studies (16,21) fell outside the upper and lower limits of 95% confidential interval, and that this may have been the source of heterogeneity.
Analysis of publication bias
For the Begg’s test of the PANSS total scores after nursing for the 2 groups, we found that P>|t|=0.042, suggesting that there may be a small degree of publication bias (see Figure 14).
Discussion
Schizophrenia is a mental illness induced by a combination of genetics, changes in the cerebral nervous system, changes in human hormones, and the acquired environment, and its pathogenesis and triggers are still not very clear (23-25). Patients with brain dysfunction, resulting in cognitive, emotional, sensory, volitional, and other mental activities, experience impairments, and the symptoms of schizophrenia are complex and variable (26,27). Patients often do not cooperate with treatment, which creates obstacles in the prognosis and outcomes of the disease (26,27). Thus, effective nursing interventions are needed to ensure smooth treatment.
Traditional nursing applies the same intervention measures to all patients, fails to consider the different disease states and nursing needs of different patients, and is very limited in terms of its clinical treatment efficacy. Conversely, personalized nursing with a quantitative evaluation of the initial severity of the disease with scientific scales, implements differentiated resource allocations and nursing intensity for patients with different symptoms and severity levels, so as to meet the needs of different patients, and improve nursing efficiency (28-31).
In this study, 11 RCT studies were included. All the articles examined the effects of routine nursing and personalized nursing with a quantitative evaluation strategy on the PANSS scores of patients. The pooled effect size showed that the PANSS scores after nursing in the experimental group were lower than those in the control group (MD =−9.95), and the treatment compliance was higher in the experimental group than the control group (OR =4.44). PANSS is an internationally accepted schizophrenia symptom severity assessment table, which is divided into 3 domains (positive symptoms, negative symptoms, and general psychiatric symptoms), and can be used to diagnose schizophrenia. Clinically, a PANSS score <60 points is often used as the cut-off line for disease diagnosis, while a PANSS score >80 points indicates a moderate grade, and a score PANSS >120 points indicates a severe grade (32,33). Thus, the reduction in PANSS scores shows the effectiveness of the personalized nursing model with a quantification-based evaluation strategy.
Quantitative evaluations and personalized care are 2 frontier branches in the field of care. A quantitative evaluation assesses and quantifies a patient’s condition, rehabilitation status with perceivable indicators and presents with digital data (34). Personalized care emphasizes respecting the individual differences of each patient and discovering the different needs of each patient through surveys to develop differentiated care plans and meet diversified care needs. The 2 have been combined and applied in the nursing process of patients with first-episode schizophrenia to assess symptoms, understand the disease status of each patient, and implement different care plans for each patient (35).
In study (8), a stratified nursing approach was carried out for the experimental group whereby mild patients were allocated resources with a nurse-patients ratio of 1:3 and room tours every 15–30 min, moderate patients were allocated resources with a nurse-patients ratio of 1:2 and room tours every 15 min, and severe patients were placed in a special ward with a configuration of nurse-patients ratio 1:1. Based on the characteristics of age and education level, patients can be provided with different levels of health education and rehabilitation nursing to cultivate their social skills, stabilize their psychological cognition, strengthen their self-management, prepare them for the better prognosis outcomes, and help them return to society. In the implementation process of nursing interventions, the subjective initiative of patients is fully mobilized, and passive treatment is transferred to active treatment to cultivate patients’ self-management abilities and minimize their psychiatric symptoms. A major feature of schizophrenia is the poor compliance (36,37). The use of both a quantitative evaluation and personalized nursing focuses the intervention on the characteristics of patients at different disease stages to effectively meet their nursing needs and improve their treatment compliance (29).
In this study, data on the quality of life and social function of the patients were also combined and analyzed. The results showed that the quality of life of the patients in the experimental group was better than that of the control group, while the social function defect score of the experimental group was lower than that of the control group. Our findings indicate that the nursing model combining quantitative evaluation with personalized nursing was helpful in improving the social function defect, quality of life, and symptoms of the patients.
The results of this study affirm the effectiveness of personalized care models with quantitative evaluation strategies; however, we also note that there was a large heterogeneity among the articles in the process of the pooling analyses for the post-care PANSS measures. We conducted subgroup and meta-regression analyses according to different ages, the initial PANSS total score, and the quantitative method of the study subjects, and found that age, the initial PANSS total score, and the quantitative method were not factors affecting the results of the meta-analysis. We performed a case-by-case sensitivity analysis and found that studies (16,21) may causing heterogeneity, presumably because of the participants were all in their remission and from communities. We also note that while all the studies adopted a care model combining quantitative evaluation with personalized care, the details of the interventions varied, which may be a source of heterogeneity. In addition, quantitative evaluations and personalized care lack the support of nursing theory and guidelines, studies vary in the content and definition of personalized care, and there is a lack of uniform standards, all of which limit the application of this care model. Begg’s test quantifying the publication bias in the combined analysis revealed that the study had a small risk of bias; thus, the application of a personalized care model with a quantitative evaluation strategy to care for patients with schizophrenia requires further in-depth research.
Conclusions
The condition of schizophrenia is complex and changeable, and the treatment compliance of patients is low. The use of a personalized nursing model with a quantitative evaluation strategy is helpful in improving patients’ symptoms, disease outcomes, treatment compliance, social function, and quality of life.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-605/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-605/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Häfner H, an der Heiden W. Epidemiology of schizophrenia. Can J Psychiatry 1997;42:139-51. [Crossref] [PubMed]
- Tandon R, Gaebel W, Barch DM, et al. Definition and description of schizophrenia in the DSM-5. Schizophr Res 2013;150:3-10. [Crossref] [PubMed]
- Granero R, Fernández-Aranda F, Pino-Gutierrez AD, et al. The prevalence and features of schizophrenia among individuals with gambling disorder. J Psychiatr Res 2021;136:374-83. [Crossref] [PubMed]
- van de Leemput J, Hess JL, Glatt SJ, et al. Genetics of Schizophrenia: Historical Insights and Prevailing Evidence. Adv Genet 2016;96:99-141. [Crossref] [PubMed]
- Nucifora FC Jr, Woznica E, Lee BJ, et al. Treatment resistant schizophrenia: Clinical, biological, and therapeutic perspectives. Neurobiol Dis 2019;131:104257. [Crossref] [PubMed]
- Yang AC, Tsai SJ. New Targets for Schizophrenia Treatment beyond the Dopamine Hypothesis. Int J Mol Sci 2017;18:1689. [Crossref] [PubMed]
- Smith JD, Hasan M. Quantitative approaches for the evaluation of implementation research studies. Psychiatry Res 2020;283:112521. [Crossref] [PubMed]
- Wang HR, Liu CF. Application of personalized nursing intervention based on quantitative evaluation strategy in adolescent first-episode schizophrenia. Journal of Nursing Education 2018;33:978-81.
- Jiang JM, Chen ZQ, Chen ZY, et al. Analysis of rehabilitation effect of personalized nursing intervention guided by quantitative evaluation on patients with first-episode schizophrenia. Chinese Medical Science 2020;10:146-9.
- Li J, Huang YG, Ran MS, et al. Community-based comprehensive intervention for people with schizophrenia in Guangzhou, China: Effects on clinical symptoms, social functioning, internalized stigma and discrimination. Asian J Psychiatr 2018;34:21-30. [Crossref] [PubMed]
- Methley AM, Campbell S, Chew-Graham C, et al. PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 2014;14:579. [Crossref] [PubMed]
- Su M, Wang CQ, Liang Y, et al. Social function deficiency and family intervention in patients with chronic schizophrenia. Guangzhou Pharmaceutical 2011;42:4.
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Ye XX. Quantitative evaluation of the application effect of guided two-point nursing in adolescent patients with first-episode schizophrenia. Chinese Contemporary Medicine 2021;28:200-2.
- Shao C, Ma MF, Guo LY, et al. Quantitative evaluation of the impact of guided two-point management on adolescent patients with first-episode schizophrenia. Hebei Medicine 2021;43:3316-8.
- Qin ZH, Chen LX. Effect of personalized nursing intervention under quantitative evaluation on self-management ability of adolescent schizophrenic patients. Chinese General Medicine 2021;19:86-8.
- Chen R, Huo BL, Xu XR. Quantitative evaluation of the effect of graded nursing combined with community comprehensive intervention on the rehabilitation of patients with schizophrenia. Chinese Geriatrics 2021;19:156-9.
- Shimada T, Ohori M, Inagaki Y, et al. A multicenter, randomized controlled trial of individualized occupational therapy for patients with schizophrenia in Japan. PLoS One 2018;13:e0193869. [Crossref] [PubMed]
- Gu XH, Zhao HY, Chen K, et al. Effect of graded rehabilitation intervention on patients with schizophrenia. Journal of Clinical Psychosomatic Diseases 2014;20:3.
- He CM, Yang QJ, Ji QM, et al. Effect of personalized intervention on quality of life of schizophrenic patients based on three-dimensional nursing grading model. Nursing Research 2017;31:3801-4.
- Xu CY, Hu XF, Zhang JM, et al. Effect of personalized intervention on social function rehabilitation of schizophrenic patients. Chinese Journal of Modern Nursing 2016;22:3603-6.
- Chen Y. Application of personalized nursing intervention in improving social function rehabilitation of schizophrenic patients. International Journal of Nursing 2019;38:3968-71.
- Stępnicki P, Kondej M, Kaczor AA. Current Concepts and Treatments of Schizophrenia. Molecules 2018;23:2087. [Crossref] [PubMed]
- Morera-Fumero AL, Abreu-Gonzalez P. Role of melatonin in schizophrenia. Int J Mol Sci 2013;14:9037-50. [Crossref] [PubMed]
- Maric NP, Jovicic MJ, Mihaljevic M, et al. Improving Current Treatments for Schizophrenia. Drug Dev Res 2016;77:357-67. [Crossref] [PubMed]
- Van Sant SP, Buckley PF. Pharmacotherapy for treatment-refractory schizophrenia. Expert Opin Pharmacother 2011;12:411-34. [Crossref] [PubMed]
- Severance EG, Dickerson FB, Yolken RH. Autoimmune phenotypes in schizophrenia reveal novel treatment targets. Pharmacol Ther 2018;189:184-98. [Crossref] [PubMed]
- Cheng Q, Ye S, Fu C, et al. Quantitative evaluation of computed and voxelwise computed diffusion-weighted imaging in breast cancer. Br J Radiol 2019;92:20180978. [Crossref] [PubMed]
- An Y, Li Y, Chang W, et al. Quantitative Evaluation of the Function of the Sensory Nerve Fibers of the Palate in Patients With Obstructive Sleep Apnea. J Clin Sleep Med 2019;15:1347-53. [Crossref] [PubMed]
- Asai S, Nakamura S, Toriihara A, et al. Quantitative evaluation of bone single-photon emission computed tomography using Z score analysis in patients with mandibular osteomyelitis. Oral Radiol 2020;36:267-74. [Crossref] [PubMed]
- Wen Z, Zhou H, Zhou J, et al. Quantitative Evaluation of Mechanical Stimulation for Tissue-Engineered Blood Vessels. Tissue Eng Part C Methods 2021;27:337-47. [Crossref] [PubMed]
- Lim K, Peh OH, Yang Z, et al. Large-scale evaluation of the Positive and Negative Syndrome Scale (PANSS) symptom architecture in schizophrenia. Asian J Psychiatr 2021;62:102732. [Crossref] [PubMed]
- Fleischhacker W, Galderisi S, Laszlovszky I, et al. The efficacy of cariprazine in negative symptoms of schizophrenia: Post hoc analyses of PANSS individual items and PANSS-derived factors. Eur Psychiatry 2019;58:1-9. [Crossref] [PubMed]
- Wen J, Wang Y, Jiang W, et al. Quantitative Evaluation of Denervated Muscle Atrophy with Shear Wave Ultrasound Elastography and a Comparison with the Histopathologic Parameters in an Animal Model. Ultrasound Med Biol 2018;44:458-66. [Crossref] [PubMed]
- Shimada T, Ohori M, Inagaki Y, et al. Effect of adding individualized occupational therapy to standard care on rehospitalization of patients with schizophrenia: A 2-year prospective cohort study. Psychiatry Clin Neurosci 2019;73:476-85. [Crossref] [PubMed]
- Kirkpatrick B, Buchanan RW, Ross DE, et al. A separate disease within the syndrome of schizophrenia. Arch Gen Psychiatry 2001;58:165-71. [Crossref] [PubMed]
- Ross DE. The deficit syndrome and eye tracking disorder may reflect a distinct subtype within the syndrome of schizophrenia. Schizophr Bull 2000;26:855-66. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)







