
Multiple synchronous neoplasms in the ipsilateral parotid gland: case series
Introduction
The majority of parotid neoplasms are benign, unilateral, and single lesion (1-4). Synchronous neoplasms refer to the development of one or more neoplasms that occur simultaneously but distinct from each other in the parotid gland (2). Therefore, multiple synchronous parotid neoplasms are very rare with a frequency of about 0.7% (1-10).
Therefore, we intend to analyze the clinical characteristics and treatment results of multiple synchronous neoplasms involving the ipsilateral parotid gland managed for 11 years at this hospital. We present the following article in accordance with the AME Case Series reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-307/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of Chonnam National University Hwasun Hospital (No. CNUHH-2021-150) and informed consent was taken from all the patients. Twenty-one cases of multiple synchronous neoplasm involving the ipsilateral parotid gland from January 2010 to December 2020 were included in this study. Previous parotid surgery or recurrent or metastatic parotid neoplasms were excluded.
The clinical data were reviewed with respect to sex, age, smoking history, location, symptoms, diagnostic method, number and size of neoplasms, fine-needle aspiration cytology (FNAC), surgical procedures, histopathologic results, complications, postoperative treatment, and recurrence. All patients underwent one or more radiological examinations, including computed tomography (CT), magnetic resonance imaging (MRI), and ultrasound (US), prior to surgery to assess the extent of the lesion and assist with treatment planning.
The type and extent of surgery depends on the location of neoplasm and the results of FNAC. All patients underwent a macroscopically complete oncologic resection. Partial parotidectomy, involving enucleation or removal of the inferior half of the superficial lobe, was performed if neoplasms were located in the tail (inferior) portion of the parotid gland. Superficial parotidectomy was performed if the parotid neoplasm was located in the superficial lobe. Total parotidectomy was performed in case the parotid neoplasm was located in the deep lobe. Intraoperative facial nerve monitoring was typically used. Drainage was performed and maintained via aspiration. All resected specimens were confirmed via histopathological examination.
Statistical analysis
Fisher’s exact test was used to compare the differences between benign and malignant parotid gland tumors. SPSS version 27.0 was used for all statistical analyses. Statistical significance was defined at a P value of <0.05.
Results
Among the 994 parotid gland surgeries performed at our hospital from January 2010 to December 2020, 21 cases (2.1%) were identified as multiple synchronous neoplasms involving the ipsilateral parotid gland. Four cases of multiple synchronous neoplasms involved bilateral parotid glands, and 21 lesions were analyzed in a total of 17 patients (Table 1). Of the 17 patients included in this study, 16 were male (94.1%) and only one was female (5.9%). The patients’ age ranged between 49 and 78 years, with a mean age of 51.5±3.5 years. Fourteen patients (82.4%) had a smoking history. Among 21 lesions, there were 9 patients of right parotid gland, 4 patients of left parotid gland, and 4 patients of bilateral parotid gland.
Table 1
| Factors | Value |
|---|---|
| Age (year), mean ± SD [range] | 51.5±3.5 [49–78] |
| Sex (male: female) | 16:1 |
| Smoking (yes: no) | 14:3 |
| Location (right: left: both) | 9:4:4 |
| Duration of symptoms (month), mean ± SD (range) | 48.4±70.9 (0.1–240) |
| Number of neoplasms (two: three) | 16:5 |
| Largest neoplasm (N=21) | |
| Size of neoplasm (cm), mean ± SD (range) | 3.1±0.9 (1.4–4.7) |
| Location of neoplasm (T:S:D) | 16:4:1 |
| Second neoplasm (N=21) | |
| Size of neoplasm (cm), mean ± SD (range) | 1.7±0.8 (0.4–3.8) |
| Location of neoplasm (T:S:D) | 16:3:2 |
| Smallest neoplasm (N=5) | |
| Size of neoplasm (cm), mean ± SD (range) | 1.3±0.6 (0.6–2.0) |
| Location of neoplasm (T:S:D) | 0:5:0 |
| Histopathologic results (N=21) | |
| Warthin tumor + Warthin tumor | 14 |
| Warthin tumor + Warthin tumor + Warthin tumor | 5 |
| Pleomorphic adenoma + pleomorphic adenoma | 1 |
| Salivary gland carcinoma with oncocytic features + pleomorphic adenoma | 1 |
| Period of follow-up (month), mean ± SD [range] | 40.1±46.7 [8–222] |
SD, standard deviation; T, tail portion; S, superficial lobe; D, deep lobe.
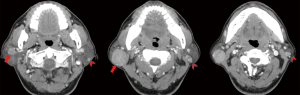
The main symptoms were slowly enlarging mass within the parotid gland (n=20), followed by incidental detection (n=1). The duration of symptoms ranged from 0.1 months to 240 months (48.4±70.9 months). Upon radiological examination, CT was performed in all cases (Figure 1), US in 10 cases and MRI in 1 case. The number of synchronous neoplasms in the ipsilateral parotid gland was 2 in 16 cases (76.2%) and 3 in 5 cases (23.8%).
The largest neoplasms ranged in size from 1.4 to 4.7 cm, with an average size of 3.1±0.9 cm. The largest neoplasm was in the tail portion of the parotid gland in 16 cases (76.2%), in the superficial lobe in 4 cases (19.0%), and in the deep lobe in 1 case (4.8%). The second neoplasms ranged in size from 0.4 to 3.8 cm, with an average size of 1.7±0.8 cm. The second neoplasm was in the tail portion of the parotid gland in 16 cases (76.2%), in the superficial lobe in 3 cases (14.3%), and in the deep lobe in 2 cases (9.5%). The smallest neoplasms ranged in size from 0.6 to 2.0 cm, with an average size of 1.3±0.6 cm. All 5 cases of the smallest parotid neoplasms were in the superficial lobe.
Based on FNAC, 13 cases were suspected with Warthin tumor and 1 case with pleomorphic adenoma. The remaining 7 cases were judged to be non-diagnostic.
Of the 21 cases of multiple synchronous neoplasms involving the ipsilateral parotid gland, 11 lesions were removed via superficial parotidectomy (52.4%), 7 lesions via partial parotidectomy (33.3%), and 3 lesions were resected via total parotidectomy (14.3%). Partial facial dysfunction was detected postoperatively in 2 cases, and facial nerve function recovered within 3 months.
Histopathology revealed the same histopathologic neoplasms [Warthin tumor (n=19), pleomorphic adenoma (n=1)] in the ipsilateral parotid gland in 20 cases, and different histopathologic neoplasms (salivary gland carcinoma with oncocytic features and pleomorphic adenoma) in the ipsilateral parotid gland in 1 case (9). One patient diagnosed with salivary gland carcinoma with oncocytic features and pleomorphic adenoma underwent postoperative radiotherapy, and the remaining 20 cases did not receive any additional treatment.
The follow-up period after surgery was 40.1±46.7 months, ranging from 8 to 222 months. No recurrence was observed in all patients.
Discussion
During 11 years, 21 cases of multiple synchronous neoplasms were identified in the ipsilateral parotid gland, with a frequency of 2.1% among all 994 cases of parotid surgery. Multiple synchronous neoplasms involving the ipsilateral parotid gland occurred in males except for one female. In addition, except for one case, all of them were the same histopathologic neoplasms and Warthin tumor (n=19, 90.5%) was the most common, as previous reports (Table 2).
Table 2
| Article | Number of cases | Average age | Dominant sex | Dominant location | Dominant tumor combinations |
|---|---|---|---|---|---|
| Kaleem et al. [2020] (1) | 1 | 63 | Male | Left | Secretory carcinoma + Warthin tumor |
| Ethunandan et al. [2006] (2) | 16 | 68 | Male | Right | Warthin tumor + Warthin tumor |
| Lu et al. [2019] (3) | 5 | 55 | Female | ND | Acinic cell carcinoma + Warthin tumor |
| Srivastava et al. [2010] (4) | 1 | 52 | Male | Right | Mucoepidermoid carcinoma + Warthin tumor |
| Roh et al. [2007] (5) | 1 | 71 | Male | Left | Adenocarcinoma + Warthin tumor |
| Curry et al. [2002] (6) | 2 | 59 | Female | Left | Mucoepidermoid carcinoma + Warthin tumor |
| Araki et al. [2004] (7) | 1 | 81 | Male | Right | Oncocytoma + Warthin tumor |
| Hall et al. [2010] (8) | 1 | 73 | Female | Left | Warthin tumor + Warthin tumor |
| Takahashi et al. [2008] (10) | 1 | 70 | Female | Left | Warthin tumor + lymphoepithelial cyst |
ND, not described.
Warthin tumor mainly occurs in the parotid gland and constitutes approximately 14–30% of all parotid neoplasms (7,8,10,11). Warthin tumor is the most common histopathologic neoplasm with a multifocal occurrence (2,7,8,10). However, Warthin tumors rarely involve multiple lesions in the ipsilateral parotid gland, and are substantially rarer than bilateral Warthin tumors (8).
Preoperative imaging tests, clinical examination, and careful intraoperative palpation are important for accurate diagnosis and treatment of multiple synchronous neoplasms in the ipsilateral parotid gland (1-3,8,9). In this study, CT was mainly used for economic reasons, but MRI is preferred for diagnosing multiple parotid tumors (3). Intraoperative frozen biopsy and meticulous intraoperative palpation can facilitate the identification of multiple synchronous neoplasms in the ipsilateral parotid gland, especially Warthin tumor (3,9).
Surgery is indicated for multiple synchronous neoplasms involving the ipsilateral parotid gland (1-11). Complete resection with sufficient safe margins is important (3). We determined that the surgical method was based on tumor location and FNAC outcome (11). In this study, superficial parotidectomy was the most frequently preformed because multiple tumors mainly occurred in the tail portion and the superficial lobe of the parotid gland, followed by partial parotidectomy and total parotidectomy. Postoperative transient facial nerve dysfunction occurred in two patients, and one each after superficial parotidectomy and partial parotidectomy. Facial nerve dysfunction resolved uneventfully within 3 months.
Additional treatment after surgery is based on the histopathological results of parotid carcinoma (9). The prognosis of multiple synchronous neoplasms involving the ipsilateral parotid is also similar to that of a single parotid carcinoma (3). In this study, no recurrence was found in all patients including one cancer patient.
Conclusions
Clinicians should be aware of the possibility of multiple synchronous neoplasms in the ipsilateral parotid gland. Accurate diagnosis and treatment require preoperative imaging tests, clinical examinations, and careful palpation during surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-307/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-307/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-307/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-307/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of Chonnam National University Hwasun Hospital (No. CNUHH-2021-150) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kaleem A, Patel N, Alzahrani S, et al. Concurrent presence of secretory carcinoma and Warthin's tumor in ipsilateral parotid gland. Oral Oncol 2020;109:104691. [Crossref] [PubMed]
- Ethunandan M, Pratt CA, Morrison A, et al. Multiple synchronous and metachronous neoplasms of the parotid gland: the Chichester experience. Br J Oral Maxillofac Surg 2006;44:397-401. [Crossref] [PubMed]
- Lu H, Xu W, Zhu Y, et al. Simultaneous occurrence of benign and malignant tumours in the ipsilateral parotid gland-retrospective study. Int J Oral Maxillofac Surg 2019;48:1138-44. [Crossref] [PubMed]
- Srivastava S, Nadelman C. Synchronous ipsilateral Warthin tumor encased by a separate mucoepidermoid carcinoma of the parotid gland: a case report and review of the literature. Diagn Cytopathol 2010;38:533-7. [Crossref] [PubMed]
- Roh JL, Kim JM, Park CI. Synchronous benign and malignant tumors in the ipsilateral parotid gland. Acta Otolaryngol 2007;127:110-2. [Crossref] [PubMed]
- Curry JL, Petruzzelli GJ, McClatchey KD, et al. Synchronous benign and malignant salivary gland tumors in ipsilateral glands: a report of two cases and a review of literature. Head Neck 2002;24:301-6. [Crossref] [PubMed]
- Araki Y, Sakaguchi R. Synchronous oncocytoma and Warthin's tumor in the ipsilateral parotid gland. Auris Nasus Larynx 2004;31:73-8. [Crossref] [PubMed]
- Hall JE, Statham MM, Sheridan RM, et al. Multifocal synchronous ipsilateral Warthin tumors: case report and review of the literature. Ear Nose Throat J 2010;89:E1-3. [Crossref] [PubMed]
- Lee DH, Choi YD, Yoon TM, et al. Synchronous pleomorphic adenoma and oncocytic carcinoma in the ipsilateral parotid gland. Br J Oral Maxillofac Surg 2018;56:629-31. [Crossref] [PubMed]
- Takahashi K, Uzawa N, Kosaka S, et al. Synchronous Warthin tumors and lymphoepithelial cyst in the ipsilateral parotid gland. J Oral Maxillofac Surg 2008;66:1053-6. [Crossref] [PubMed]
- Lee DH, Yoon TM, Lee JK, et al. Surgical treatment strategy in Warthin tumor of the parotid gland. Braz J Otorhinolaryngol 2019;85:546-50. [Crossref] [PubMed]


