
Effect of outpatient physician involvement on the physician orders for life-sustaining treatment completed by hospitalists: a cross-sectional study
Introduction
Hospitalists are specialists in inpatient care. In the United States, they play a positive role in improving the quality of inpatient care, reducing medical costs, and shortening hospital length of stay (1). Moreover, the number of hospitalists has been increasing exponentially every year (2). The hospitalist system in Korea was first introduced in 2015 to reduce the working hours of medical residents and improve the quality of care. Since then, it has been gradually expanded to many hospitals. Recent studies conducted in Korea reported that introduction of the hospitalist program reduced the time spent in the emergency room, hospital length of stay, and transfer rate to the intensive care unit (ICU) (3,4).
In Korea, the “Act on Hospice, Palliative Care, and Life-sustaining Medical Decisions for Patients in the End-of-Life Process (Life-Sustaining Medical Decision Act)” was enacted and applied to the clinical settings from February 4, 2018. The Life-Sustaining Medical Decision Act is a law that protects patients who consider resuscitative efforts to be at odds with their goals of care from undesired life-sustaining treatments (LSTs), through their own decision or the consent of their surrogates. Suspension of LST is intended for patients whose symptoms worsen rapidly and are in the end-of-life (EOL) process. The physician orders for life-sustaining treatment (POLST) was actively introduced during the legislation of the Life-Sustaining Medical Decision Act.
The POLST, which was initially implemented in 1993 at the Oregon Health Sciences University, is a standardized medical order that is supposed to record a discussion between a physician and a patient with severe disease. POLST is a process to improve EOL care, creating specific medical orders to be honored by physicians, nurses, and other healthcare assistants (5). Contrary to the “do not resuscitate (DNR)” form, POLST includes more information on the types of EOL intervention that the patient with terminal disease chooses to receive (6). Although POLST offers more information than a standard DNR form, there are patient safety concerns that relate to the discordant understanding between the patient and the provider completing POLST (7). In Korea, the Life-Sustaining Treatment Decision Act was applied in the clinical setting under the government’s initiative, and the government decided to use the POLST form as part of the EOL care.
Hospitalists are becoming increasingly involved in EOL care decision making for their patients (8). An inpatient stay may be an opportunity for patients to consider whether they want additional hospitalization or where they are in the course of their disease. While patients are in the hospital, they can have in-depth consultations with hospitalists and have a lot of time to plan such things. Hence, it is important to determine whether the LST should be implemented in patients during the EOL process; for patients who have not yet decided on this, hospitalists are involved in the completion of POLST. Because hospitalists are not physicians who have continuously treated patients in an outpatient setting, the continuity of care may be poor. Moreover, it may be difficult for hospitalists to establish a rapport with patients and caregivers, creating a major obstacle for POLST completion. In such situations, the physician who treated the patient in an outpatient setting can be involved in the decision making.
In this study, we aimed to analyze the results of POLST implementation in patients who discussed the treatment with hospitalists who completed POLST. In addition, we aimed to investigate the effect of outpatient physician involvement on POLSTs completed by hospitalists. We present the following article in accordance with STROBE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3158/rc).
Methods
Study design and participants
A retrospective cohort study was conducted in patients aged 18 years or older who were admitted to the hospitalist wards of Seoul National University Bundang Hospital (SNUBH), a quaternary-care academic medical center, and completed POLST between February 2018 and March 2020. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The SNUBH institutional review board reviewed and approved this study design (B-2012-655-107) and waived the need for obtaining an informed consent from participants.
Procedures and data collection
POLST completion was conducted in patients nearing EOL and patients with terminal disease. EOL and terminal disease are defined as statutory provisions in the Life-Sustaining Medical Decision Act. The EOL process refers to a condition in which there is no possibility of recovery despite treatment, the symptoms worsen rapidly, and death is imminent. Terminal diseases are defined as diseases with life expectancy of less than several months due to irreversible organ dysfunction. The above two situations are determined based on the medical judgment of the doctor in charge and one medical specialist in the relevant field.
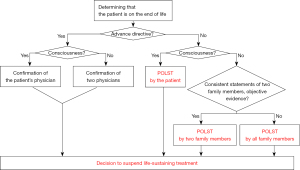
The hospitalists completed POLST with patients or their legal representatives in the following manner: If the patient had previously completed an advanced directive (AD), the doctor confirmed it and proceeded according to the preliminary AD. If no AD was made, the method differed depending on whether the patient was conscious. If the patient was conscious and able to make decisions, he or she was asked to sign the POLST form. In the absence of consciousness, if there was objective evidence such as a living will or video to prove that the patient would not receive LST, a statement from two family members was required. Consent from all family members was required in the absence of such objective evidence. This process is summarized in the flowchart in Figure 1. This flowchart was created in accordance with the laws presented in the Life-Sustaining Medical Decision Act of Korea. According to this act, although a certain patient was in the EOL process due to terminal disease, if the patient wanted full treatment including cardiopulmonary resuscitation, the patient was excluded from the indication of POLST.
POLST included the following information: the patient’s disease status and intervention options; the implementation method of LST and decision for suspension of LST; the use of hospice care; details on the proceedings for completion, registration, custody, modification, and withdrawal of POLST; and the use of the Medical Institution Ethics Committee. Patients and their surrogates can determine the LST category. The LSTs include cardiopulmonary resuscitation, mechanical ventilation, hemodialysis, extracorporeal membrane oxygenation, vasopressor drugs, transfusion, and chemotherapy. After the hospitalists explain the procedures and complications of LST, they decide whether to perform these procedures (Figure S1).
The hospitalist physicians underwent training on how to have a conversation and complete the form on January 31, 2018. The hospitalists who could not attend on that day were required to undergo video training.
Demographic data, including age, sex, diagnosis, educational attainment, outpatient physician involvement, and POLST-discordant ICU care, were obtained. Outpatient physician involvement was defined as the participation of the physician who followed up the patient in counseling during the completion of the POLST form.
Statistical analysis
The characteristics of the patients’ baseline data and POLST are expressed as median with ranges for continuous variables and as frequencies and percentages for categorical variables. Comparisons were performed using the Student’s t-test for continuous variables, and chi-square or Fisher’s exact tests for categorical variables. A multivariate logistic regression analysis was performed to assess the differences of POLST characteristics depending on the outpatient physicians’ involvement. All tests were two sided and performed at a significance level of 0.05. Statistical analyses were performed using IBM SPSS v. 21.0 (IBM Corp, Armonk, NY, USA).
Results
Study patients
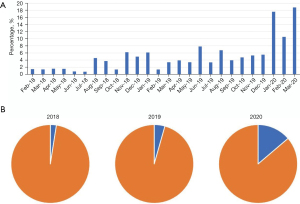
Between February 2018 and March 2020, 3,533 POLST forms were written at SNUBH, of which 175 (5.22%) were completed by hospitalists. Figure 2A shows the percentage of POLSTs completed by hospitalists among all patients. As shown in Figure 2B, the proportion of POLSTs completed by hospitalists were 2.53% in 2018, 4.58% in 2019, and 15.9% in 2020. The oncological co-management in SNUBH was initiated in 2020. A total of 175 patients with POLSTs completed by hospitalists were eligible for this study.
Patient’s baseline characteristics
The clinical characteristics of the patients and POLSTs are summarized in Table 1. The median age of the participants was 75 (range, 34–98) years, and 88 (50.3%) were female. A total of 144 (82.3%) patients had malignancies, while 31 (17.7%) patients had non-cancer illnesses. Among the malignancies, lung cancer was the most common (22.3%), followed by gastrointestinal cancer (17.7%); hepato-pancreatico-biliary cancer (17.1%); breast cancer (12%); genitourinary cancer (6.3%); hematologic malignancy (4.6%); and others (6.9%), including brain tumors, metastasis of unknown origin, soft tissue sarcoma, skin cancer, and thymic cancer. Dementia was the most common non-cancer illness (9.7%), followed by severe lung disease (4.0%), heart failure (1.1%), chronic kidney disease (1.1%), severe liver disease (0.6%), and rheumatoid disease (1.1%). Among the 175 patients, 102 (58.3%) had achieved higher education after completing high school.
Table 1
| Variables | No. of patients (n=175) |
|---|---|
| Age, median (range, year) | 75 (34–98) |
| Sex, n (%) | |
| Male | 87 (49.7) |
| Female | 88 (50.3) |
| Diagnosis (underlying medical condition), n (%) | |
| Malignancy | 144 (82.3) |
| Lung cancer | 39 (22.3) |
| Gastrointestinal cancer | 31 (17.7) |
| Hepato-pancreatico-biliary cancer | 30 (17.1) |
| Breast cancer | 12 (6.9) |
| Genitourinary tract cancer | 11 (6.3) |
| Hematologic malignancy | 8 (4.6) |
| Others | 12 (6.9) |
| Non-cancer illness | 31 (17.7) |
| Dementia | 17 (9.7) |
| Severe lung disease | 7 (4.0) |
| Heart failure | 2 (1.1) |
| Chronic kidney disease | 2 (1.1) |
| Severe liver disease | 1 (0.6) |
| Rheumatoid disease | 2 (1.1) |
| Educational attainment, n (%) | |
| < High school | 73 (41.7) |
| High school | 59 (33.7) |
| College or more | 43 (24.6) |
| Outpatient physician’s involvement, n (%) | 83 (47.4) |
| POLST-discordant ICU care, n (%) | 4 (2.3) |
POLST, physician orders for life-sustaining treatment.
In 47.4% of the cases, the outpatient physicians in charge of the patients were involved in the process of completing the POLST form through consultation. Four patients received POLST-discordant ICU care, which accounted for 2.3% of the total patients.
Characteristics of POLST
The characteristics of POLST are summarized in Table 2. Ninety-seven (55.4%) patients directly signed the POLST form, while 78 (44.6%) were signed by the patients’ legal representatives. Only 23 (13.1%) patients selected “comfort measures only,” which means that the patients did not wish to receive any LST, and 152 (86.9%) patients chose limited intervention as LST.
Table 2
| Variables | No. of POLSTs (n=175) |
|---|---|
| POLST signatory, n (%) | |
| Patients making decisions | 97 (55.4) |
| Surrogates’ decisions | 78 (44.6) |
| Choices selected on POLST forms, n (%) | |
| Comfort measures only | 23 (13.1) |
| Limited additional intervention | 152 (86.9) |
POLST, physician orders for life-sustaining treatment.
Comparison between the groups with and without outpatient physician involvement
Table 3 shows the differences according to the status of outpatient physician participation in the POLST completion process. In the group that received POLST through the participation of outpatient physicians, the proportion of younger patients, patients with malignant diseases, and patients who chose comfort measures alone was relatively higher than the group without outpatient physician involvement. Results of the multivariate analysis showed that in patients with malignancies, outpatient physicians were involved more frequently during the POLST completion process (P=0.02). When the outpatient physicians were involved, more patients signed the POLST form themselves (P=0.02) and chose comfort measures only when asked to determine their preferred LST type (P=0.00). No significant difference was observed in the POLST-discordant ICU care between the two groups (P=0.19).
Table 3
| Variable | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| Odds ratio (95% CI) | P value | Odds ratio (95% CI) | P value | ||
| Male sex | 1.02 (0.57–1.85) | 0.94 | 1.02 (0.51–2.01) | 0.97 | |
| Age >60 years | 0.37 (0.18–0.77) | 0.01 | 0.41 (0.17–1.01) | 0.05 | |
| Malignancy | 6.15 (2.24–16.90) | 0.00 | 3.90 (1.29–11.81) | 0.02 | |
| Education, > high school | 0.97 (0.53–1.76) | 0.91 | 0.74 (0.36–1.56) | 0.43 | |
| Signatory | 0.35 (0.19–0.65) | 0.00 | 0.42 (0.20–0.85) | 0.02 | |
| Selected LST | 5.14 (1.67–15.82) | 0.00 | 6.66 (1.98–22.33) | 0.00 | |
| ICU care | 3.41 (0.35–33.46) | 0.19 | 5.35 (0.44–65.07) | 0.19 | |
POLST, physician orders for life-sustaining treatment; LST, life-sustaining treatment.
Discussion
Since Wachter et al. first named a hospitalist as a doctor who specializes in caring for inpatients in the United States in 1996 (9), many countries, such as Canada and Japan, have introduced the hospitalist system. Since its introduction in 2015, the hospitalist system in Korea has evolved and diversified; it now includes quality improvement and inpatient safety (10). However, the role of the hospitalist has not been standardized and varies according to the needs of each hospital. According to the 2014 survey of the Society of Hospital Medicine, hospitalists play various roles, including primary care physician referral, medical co-management, palliative care, and others. As reported in this survey, 15.6% of the hospital medicine groups for adults were responsible for providing palliative care. As part of palliative care, the EOL care for patients with terminal disease is also conducted by hospitalists. According to one study, POLST sometimes does not reflect the patient wishes well (7), so it is important to train the hospitalists to prevent these medical errors.
The hospitalist system was introduced in 2015 in SNUBH. From 2015 to 2019, the hospitalists in SNUBH were mainly in charge of acute medical units and surgical co-management. After the implementation of oncological co-management in SNUBH in January 2020, it has become usual for hospitalists to provide palliative care for patients with malignant disease. In the oncological co-management at SNUBH, hospitalists are mainly responsible in managing the acute medical problems of cancer patients, treating the complications of chemotherapy (e.g., neutropenic fever), treating various infections, providing pain management, and providing EOL care. They are not in charge of administering chemotherapy, which is administered by oncologists. Therefore, the frequency of POLST completion by hospitalists has increased significantly in 2020 compared to that in 2018 and 2019.
A total of 144 (82.3%) patients had malignancies and 31 (17.7%) patients had non-cancer illnesses. Although the proportion of cancer patients who underwent POLST was more than four times higher than that of patients without cancer, 20% of the patients with non-cancer illnesses were also included. With the rapid aging of the population and the development of medical science, the number of patients with chronic diseases unrelated to cancer continues to increase; hence, the hospitalization rate of these patients will also increase. Therefore, the role of hospitalists in terms of EOL care and POLST completion will become more important.
Continuity of care commonly affects patient satisfaction. It consists of provider continuity, information continuity, and management continuity (11). Since the hospitalists are not in charge of outpatient treatment and are only responsible for providing inpatient care, they have a limited role in continuity of care, such as providing the direction of treatment (12). If a patient does not have AD or has not discussed LST prior to his or her admission to a hospitalist ward and is nearing EOL due to the aggravation of the disease, the hospitalists and patients who have to decide on the level of LST will experience considerable confusion. To overcome this problem, The Realistic Interpretation of Advance Directives (TRIAD) VIII research was conducted, where a video testimonial/message was found to improve communication between patients and medical providers (13).
For patients whose clinical condition is expected to worsen due to a malignant or chronic irreversible disease, the LST should be fully explained by a physician who has established sufficient rapport with the patient (14). The involvement of outpatient physicians in the completion of POLST is a way to overcome the discontinuity in care.
In this study, the patients were divided into two groups according to the status of outpatient physician involvement. The multivariate analysis in Table 3 shows that the participation of outpatient physicians was significantly higher in patients with malignant diseases. The nature of cancer fosters long-term rapport between the patient and physician. In fact, most patients with malignant diseases want their oncologists to know about the course of their disease and life expectancy (15). Hence, oncologists must provide patients and their caregivers with accurate information about the disease prognosis and treatment options in a timely manner to enable rational decision making. Moreover, they also play a crucial role in EOL care and POLST completion in patients with malignant diseases (16).
The involvement of outpatient physicians also affected the POLST characteristics. According to the results of the multivariate analysis in Table 3, when the outpatient physician intervened during the completion of the POLST, the patients directly signed the POLST rather than their surrogates. The fact that the patients were the ones who signed this form indicate that they are paying attention, suggesting that the outpatient physician’s involvement is more likely in such situations. In addition, if an outpatient physician was involved, the patients were more likely to choose comfort measures only when determining the LST type.
This study is the first to investigate the characteristics of POLST completion by hospitalists in patients with cancer and non-cancer illnesses. We also compared the characteristics of POLST completion according to the status of outpatient physician involvement. However, this study had some limitations. First, this was a retrospective cohort study conducted at a single referral center. The hospitalist’s role in completing POLST may vary from hospital to hospital, as the hospitalist system operates differently depending on the needs of each hospital. Thus, further studies on POLST in various hospital settings are required. Second, this study has relatively little information on non-cancer illnesses, as most of the study participants were cancer patients. Hence, additional research is warranted to confirm the POLST status of patients with terminal chronic diseases other than cancer. Lastly, we determined whether the outpatient physician was involved in POLST completion based on the data documented in the charts, such as consultation replies or nursing records. Although it was not recorded on the chart, the possibility that the outpatient physician contributed to the patient’s POLST could not be excluded. However, it seems reasonable to avoid including undocumented outpatient physicians’ interventions, as medical records are an important tool for physicians to communicate with each other.
Conclusions
Outpatient physicians participated in POLST completion by hospitalists in less than half of the cases, and non-goal-concordant LST was reduced when the outpatient physicians were involved in POLST completion. Therefore, it is important to increase the continuity of care through the active participation of outpatient physicians in the EOL care of patients.
Acknowledgments
We would like to thank Editage (www.editage.co.kr) for English language editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3158/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3158/dss
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3158/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3158/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The SNUBH institutional review board reviewed and approved this study design (B-2012-655-107) and waived the need for obtaining an informed consent from participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Auerbach AD, Wachter RM, Katz P, et al. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med 2002;137:859-65. [Crossref] [PubMed]
- Wachter RM, Goldman L. Zero to 50,000 - The 20th Anniversary of the Hospitalist. N Engl J Med 2016;375:1009-11. [Crossref] [PubMed]
- Ohn JH, Kim NH, Kim ES, et al. An Acute Medical Unit in a Korean Tertiary Care Hospital Reduces the Length of Stay and Waiting Time in the Emergency Department. J Korean Med Sci 2017;32:1917-20. [Crossref] [PubMed]
- Lee JH, Kim AJ, Kyong TY, et al. Evaluating the Outcome of Multi-Morbid Patients Cared for by Hospitalists: a Report of Integrated Medical Model in Korea. J Korean Med Sci 2019;34:e179. [Crossref] [PubMed]
- Meier DE, Beresford L. POLST offers next stage in honoring patient preferences. J Palliat Med 2009;12:291-5. [Crossref] [PubMed]
- Jesus JE, Geiderman JM, Venkat A, et al. Physician orders for life-sustaining treatment and emergency medicine: ethical considerations, legal issues, and emerging trends. Ann Emerg Med 2014;64:140-4. [Crossref] [PubMed]
- Mirarchi FL, Juhasz K, Cooney TE, et al. TRIAD XII: Are Patients Aware of and Agree With DNR or POLST Orders in Their Medical Records. J Patient Saf 2019;15:230-7. [Crossref] [PubMed]
- Auerbach AD, Pantilat SZ. End-of-life care in a voluntary hospitalist model: effects on communication, processes of care, and patient symptoms. Am J Med 2004;116:669-75. [Crossref] [PubMed]
- Wachter RM, Goldman L. The emerging role of “hospitalists” in the American health care system. N Engl J Med 1996;335:514-7. [Crossref] [PubMed]
- Chae W, Park EC, Lee KY, et al. Development and Evolution of Hospital Medicine in Korea. J Hosp Med 2021;16:247-50. [Crossref] [PubMed]
- van Walraven C, Oake N, Jennings A, et al. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract 2010;16:947-56. [Crossref] [PubMed]
- Turner J, Hansen L, Hinami K, et al. The impact of hospitalist discontinuity on hospital cost, readmissions, and patient satisfaction. J Gen Intern Med 2014;29:1004-8. [Crossref] [PubMed]
- Mirarchi FL, Cooney TE, Venkat A, et al. TRIAD VIII: Nationwide Multicenter Evaluation to Determine Whether Patient Video Testimonials Can Safely Help Ensure Appropriate Critical Versus End-of-Life Care. J Patient Saf 2017;13:51-61. [Crossref] [PubMed]
- Brinkman-Stoppelenburg A, Rietjens JA, van der Heide A. The effects of advance care planning on end-of-life care: a systematic review. Palliat Med 2014;28:1000-25. [Crossref] [PubMed]
- Hagerty RG, Butow PN, Ellis PA, et al. Cancer patient preferences for communication of prognosis in the metastatic setting. J Clin Oncol 2004;22:1721-30. [Crossref] [PubMed]
- Lammers AJ, Zive DM, Tolle SW, et al. The oncology specialist’s role in POLST form completion. Am J Hosp Palliat Care 2018;35:297-303. [Crossref] [PubMed]


