
Systematic review and meta-analysis: value of venous blood gas in the diagnosis of acute exacerbation of chronic obstructive pulmonary disease in Emergency Department
Introduction
Chronic obstructive pulmonary disease (COPD) is a pulmonary disease for which airflow limitation is the main manifestation. The airflow limitation is completely irreversible and shows progressive development. The causes of its pathogenesis are complex and diverse, and include changes in the internal and external structures and functions of the lungs, and inflammation. Due to the large number of patients with COPD and its high mortality rate, it has now become a public-health concern, and its morbidity and mortality rates continue to increase year by year (1). COPD is a common chronic respiratory disease in our country. Currently, it occupies the first place in the burden of disease. COPD not only seriously affects the life and health of patients, but also places a huge economic burden on patients. The global annual medical expenditure for COPD is about 24 billion U.S. dollars, and 70% of the expenditure is related to acute exacerbation that requires hospitalization.
The acute exacerbation of COPD (AECOPD) is a developmental process of COPD. For a long time, it has been neglected because it is believed to have little effect on the course of the disease. Studies have estimated that on average COPD exacerbations occur 2.5–3 times per year per patient (2,3). Further, the frequency of the exacerbations increases with the severity of the disease, and about half of the exacerbations do not attract the attention of patients. Repeated acute exacerbation is an important clinical feature of COPD, and is not only related to significant physiological decline, but also to increased airway inflammation caused by viruses, bacteria, and air pollution (4). Repeated exacerbation not only affects the health of individuals, but also leads to increased medical expenses and mortality. The effect of the acute exacerbation of chronic obstructive swelling in the prognosis of the disease is still relatively serious; thus, the acute exacerbation of chronic obstructive swelling diagnosis and treatment require attention (5,6).
A blood gas analysis is an important examination that is used to assess the severity of AECOPD and guide the treatment of mechanical assisted ventilation. It plays a vital role in the rescue and monitoring of critical illnesses. COPD blood gas abnormalities first manifest as mild or moderate hypoxemia, and as the disease progresses, the hypoxemia gradually worsens, and hypercapnia appears (7). At present, there are two main types of clinical blood gas examinations; that is, arterial blood gas (ABG) analysis and venous blood gas (VBG) analysis (8).
Arterial blood gas analysis, as the gold standard for evaluating oxygenation and acid-base analysis, can indirectly assess lung function levels through arterial blood gas analysis (9), ABG analysis occupies an important position in the diagnosis and treatment of the acute exacerbation of chronic obstructive swelling disease, as it accurately provides important information, including information about the cause and severity of the disease. In recent years, as the technology continues to mature, the information it provides has become more abundant and diverse (10). However, ABG analysis may take a long time in emergency application, and may lead to the risk of arterial injury and thrombosis (11). VBG analysis method based on real-time analyzer in emergency department can provide patients’ coagulation function, pH, and electrolyte status quickly, which can greatly reduce the risk borne by patients in the process of arterial blood collection, reduce iatrogenic injury, and reduce medical costs. Timely determination of the severity of the disease and implementation of intervention measures can provide effective help for the treatment of patients (12). It plays an important role in the diagnosis and treatment of emergency diseases. However, it is still controversial whether VBG analysis can completely replace ABG analysis in AECOPD diagnosis. Some researchers believed that venous and arterial blood flow disease status may lead to differences between VBG and ABG measurement variables, and that factors such as heart failure and obesity may affect the results of VBG analysis (13). Therefore, the clinical application value of VBG in the diagnosis of AECOPD needs further discussion and research. To systematically evaluate the clinical application value of VBG in the diagnosis of AECOPD, meta-analysis was implemented to evaluate the difference between ABG and VBG in the diagnosis of AECOPD, providing a reference basis for the diagnosis and treatment of patients with AECOPD in clinical emergency. We present the following article in accordance with the MOOSE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-336/rc).
Methods
Articles retrieval strategies
Databases, including Medline, Excerpta Medica Database (EMBASE), Elton B. Stephens. Company (EBSCO), OVID, China Biomedical Database, and Wanfang, were searched using combinations of the related keywords and medical heading terms related to the blood gas analysis of patients with AECOPD. The search period ran from the establishment of the databases to September 2021. The following keywords were used: chronic obstructive pulmonary disease, COPD, blood gas analysis, emergency, acute exacerbation, case-control study, cohort study, and risk factors. The full texts of the target articles were obtained in accordance with the pre-established inclusion and exclusion criteria. The references in the searched articles were also manually searched to avoid any important documents being missed.
Inclusion and exclusion criteria of the included articles
To be eligible for inclusion in the meta-analysis, the articles had to meet the following inclusion criteria: (I) Concern a case-control or cohort study; (II) comprise patients with AECOPD; (III) examine the measurement outcomes of potential of hydrogen (pH), partial pressure of carbon dioxide (PaCO2), and hydro-carbonate (HCO3); (IV) use the inspection methods of ABG and VBG analyses; and (V) have data available for analysis, such as relative risk or odds ratio (OR) and 95% confidence interval (CI) data.
Articles were excluded from the meta-analysis if they met any of the following exclusion criteria: (I) had no effect size available for analysis (i.e., lacked cases or control numbers); (II) did not provide original data (i.e., was a comment, series report, letter, case report, or concerned zoology studies or in-vivo studies); and/or (III) only reported deaths.
Articles screening
The articles were independently screened by two researchers, who also extracted and cross-checked the data. If differences in opinions arose, experts were consulted to decide the data selection issue.
Data extraction
The two researchers independently read the articles and determined whether each article was a case-control or cohort study, and whether the data was complete. The articles were excluded or excluded in the meta-analysis based on the above-mentioned criteria. The quality of each article was evaluated, and duplicate reports, articles of poor quality, and those in which the researchers had little confidence were excluded. The data were extracted according to the established tables, and a database was established to check the data. If a research report was incomplete, the author was contacted and the full text was requested, and if the author confirmed that the article was unavailable, it was excluded from this study. If a disagreement arose between the two researchers, the issue was discussed with a third party.
After the full text was obtained, the data were extracted. If there were repeated reports, the most recent research article was selected. The data extracted for this study included basic information about the articles (i.e., the article title, first author, publication year, author information, and source), the basic characteristics of subjects (i.e., gender, age), the research methods, the research plan design, the intervention measures for the experimental group and the control group, the outcome evaluation indicators, and the outcome data.
Quality evaluation
The Newcastle-Ottawa Scale (NOS) was used to evaluate the literature quality. The NOS mainly includes three parts and eight aspects. NOS includes 4 points for study population selection, 2 points for comparability between groups, 3 points for proper measurement of exposure factors, or 3 points for proper measurement of results. There is a full score of 9, and 6 points or more suggests high quality literature.
Statistical analysis
Meta-analysis of the included literatures was performed using RevMan5.3, and the quality of the literatures was evaluated using NOS. The calculation method used the odds ratio (OR) as the effect size, and the 95% confidential interval (CI) was adopted to express the results. For the analysis of heterogeneity, the chi-square test was used to conduct a preliminary test of the heterogeneity of the literature, and the significance level of the test was set as α=0.05, and P<0.05. Quantitative assessment of heterogeneity results was then performed using I2 in RevMan5.3. When I2<25%, the literature had low heterogeneity; when 25%<I2<50%, the literature had moderate heterogeneity; when I2>50%, the literature had substantial heterogeneity. Hence, when I2<50%, a fixed-effect model was used for meta-analysis; when I2>50%, a random-effects model was used for meta-analysis. A funnel chart was used to analyze the publication bias of each risk factor. RevMan5.3 was used to output the forest plot, and the Z value and P value in the results were extracted to judge the results of meta-analysis. Each effect size was expressed by 95% confidence interval (CI), and P<0.05 indicated that the difference was statistically significant.
Results
Basic information and quality assessment of literature
A total of 3,337 related articles were retrieved in this study, of which 2,299 were retrieved from the databases and 1,038 were retrieved manually. Through a series of screening, a total of 3,330 irrelevant and unsatisfactory articles were finally excluded. Ultimately, 7 articles (14-20) that met the inclusion criteria were included in the meta-analysis. The NOS was used to evaluate the quality of the literature, 3 articles were scored 7 points, and 4 articles were scored 8 points, suggesting that the quality of the included literature was high. The details and NOS scores are shown in Figure 1 and Table 1.
Table 1
| First author | Experimental | Controls | Year of publication | Country | NOS score |
|---|---|---|---|---|---|
| Rang LC (14) | 218 | 62 | 2002 | China | 7 |
| Kelly AM (15) | 107 | 107 | 2005 | Australia | 8 |
| Ak A (16) | 132 | 132 | 2006 | China | 8 |
| Ibrahim I (17) | 122 | 122 | 2011 | America | 7 |
| O’Connor TM (18) | 30 | 30 | 2011 | UK | 8 |
| McCanny P (19) | 59 | 30 | 2012 | America | 7 |
| Kelly AM (20) | 53 | 53 | 2013 | Australia | 8 |
NOS, Newcastle-Ottawa scale.
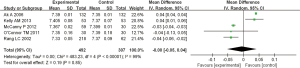
pH detection
Of the 7 articles, 5 (14,16,18-20) compared and studied the pH values of the ABG and VBG analyses of the AECOPD patients. A meta-analysis was performed on the content of the blood gas analyses and pH of these 5 articles, and it was found that I2=99% and P<0.00001. As the I2 was >50%, there was heterogeneity among the articles, and thus the random-effects model (REM) was selected. The meta-analysis results were as follows: mean difference (MD) =–0.00, 95% CI =–0.05 to 0.04, Z=0.19, and P=0.85. Thus, there was no significant difference between the upper ABG and VBG analyses in the pH test results of the AECOPD patients. A forest diagram of the analysis of the pH detection results is shown in Figure 2.
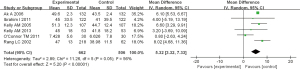
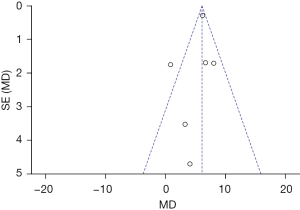
PaCO2 detection
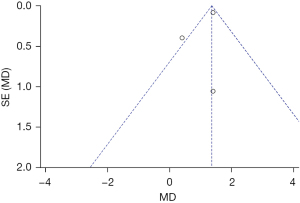
Of the 7 articles, 6 (14-18,20) compared and studied the PaCO2 values of the ABG and VBG analyses of the AECOPD patients. A meta-analysis was performed on the content of the blood gas analyses and the PaCO2 values of these 6 articles, and it was found that I2=56% and P=0.05. As the I2>50%, there was heterogeneity among the articles, and thus the REM was selected. The meta-analysis results were as follows: MD =5.32, 95% CI =3.32–7.33, Z=5.20, and P<0.00001. Thus, there was no significant difference between the upper ABG and VBG analyses in the PaCO2 values of the AECOPD patients. A forest diagram of the analysis of the PaCO2 detection results is shown in Figure 3. Figure 4 shows a funnel chart of the analysis of pCO2 detection results. As Figure 4 shows, the funnel chart was basically symmetrical, and most of the data corresponded to points within the 95% CI, which indicated that publication bias was effective.
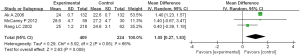
HCO3 detection
Of the 7 articles, 3 articles (14,16,20) compared and studied the HCO3 values of the ABG and VBG analyses of the AECOPD patients. A meta-analysis was performed on the content of blood gas analysis and HCO3 values of these 3 articles, and it was found that I2=66% and P=0.05. As the I2 was >50%, there was heterogeneity among the articles, and thus the REM was selected. The meta-analysis results were as follows: MD =1.05, 95% CI =0.27–1.83, Z=2.63, and P=0.009. Thus, there was an obvious difference between the ABG and VBG analyses of the HCO3 values of the AECOPD patients. A forest diagram of the analysis of the HCO3 detection results is shown in Figure 5. Figure 6 shows a funnel chart of the analysis of the pCO2 detection results. As Figure 6 shows, the funnel chart was basically symmetrical, and most of the data corresponded to points within the 95% CI, which indicated that the publication bias was effective.
Discussion
COPD is a disease characterized by airflow limitations, is incompletely reversible and progressive, and is related to the abnormal inflammatory response of the lungs to harmful gases or harmful particles. Under the action of a variety of pathogenic factors, alveolar macrophages produce a variety of neutrophil chemotactic factors, including interleukin-8 and leukotriene B4, so that neutrophils release elastase and other proteolytic enzymes, causing damage to the entire airway and lung parenchyma (21). When patients are in acute exacerbation, due to increased oxygen consumption and respiratory load, and exceed the self-compensation limit, severe hypoxemia and hypercapnia, respiratory failure, or the exacerbation of original respiratory failure may result (22). Thus, AECOPD poses a great threat to the life and health of patients. Research has shown that as the environment and climate continue to deteriorate, the frequency of the occurrence of AECOPD continues to increase year by year (23). For a long time, people have paid little attention to AECOPD; however, the disease poses a huge threat to people’s health and quality of life. Thus, it is necessary to conduct in-depth examination on the diagnosis of and treatment methods for AECOPD.
Clinically, blood gas analysis is an important method and means by which emergency departments can evaluate the condition and progress of AECOPD patients. Generally, there are two types of blood gas analyses; that is, ABG and VBG (24-26). The ABG analysis is the gold standard test for clinical evaluations of the ventilation status of AECOPD patients. It not only helps doctors determine a patient’s ventilation and acid-base status, but also helps doctors determine whether further medication and non-invasive ventilation are needed (27-29). There are many advantages for ABG, and ABG plays a pivotal role in the diagnosis and treatment of AECOPD patients. However, the ABG analysis also has some limitations. For example, the sampling time for an ABG analysis is accompanied by the risk of bleeding, hematoma, infection, nerve damage, finger ischemia, and other vascular diseases (30,31). Further, blood sampling requirements also increase the risk of staff injury. Conversely, the VBG analysis can be conducted when a patient is intubated, and the pain and risk to patients are relatively low (32). Thus, the VBG analysis is becoming more and more popular in clinical practice, and more and more studies are being conducted on ABG and VBG analyses.
To date, a study has investigated the possibility of VBG sampling instead of ABG sampling in emergency situations (33). One study found a good correlation between the venous and arterial values of pH, but only a small correlation with PaCO2 (34). A previous study has shown that venous PaCO2 can predict arterial hypercapnia (35). There is more and more evidence to support the value of VBG sampling in the evaluation of patients with acute respiratory diseases in the emergency department, but there are also reports of research results that are consistent with the above viewpoints. For example, a study has shown that there is a significant difference between arterial and venous pH in pediatric patients (36). The relevant result indicators of a blood gas analysis can be affected by many factors, which may be the reason for the different results of these studies. Thus, further research needs to be conducted on the clinical application value of the VBG analysis and whether it can completely replace the ABG analysis.
In this study, articles related to the blood gas analysis of AECOPD patients were retrieved to analyze the consistency of the ABG and VBG examination results in relation to three indicators (i.e., PaCO2, pH, and HCO3). We found that the ABG and VBG analyses had significant differences in terms of PaCO2 and pH, but were more consistent in terms of HCO3. Thus, the VBG analysis has certain clinical application value in the diagnosis of AECOPD patients, but the question of whether it can replace the ABG analysis requires further discussion.
Conclusions
In this study, articles related to the blood gas analysis of AECOPD patients were retrieved to analyze the consistency of the ABG and VBG examination results in relation to three indicators (i.e., PaCO2, pH, and HCO3). We found that the ABG analysis and the VBG analysis had significant differences in terms of PaCO2 and pH, but were more consistent in terms of HCO3. Thus, the VBG analysis has certain clinical application value in the diagnosis of AECOPD patients, but the question of whether it can replace the ABG analysis requires further discussion. This study provided a reference and basis for the clinical diagnosis and treatment of AECOPD patients. However, as the articles included in this study were not sufficiently comprehensive and rich, there may be some deviations in the research results of this study. In the future, we intend to further expand the scope of our search to undertake more in-depth and comprehensive research.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-336/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-336/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Halpin DMG, Criner GJ, Papi A, et al. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2021;203:24-36. [Crossref] [PubMed]
- MacLeod M, Papi A, Contoli M, et al. Chronic obstructive pulmonary disease exacerbation fundamentals: Diagnosis, treatment, prevention and disease impact. Respirology 2021;26:532-51. [Crossref] [PubMed]
- Byanova K, Kunisaki KM, Vasquez J, et al. Chronic obstructive pulmonary disease in HIV. Expert Rev Respir Med 2021;15:71-87. [Crossref] [PubMed]
- Hanania NA, O'Donnell DE. Activity-related dyspnea in chronic obstructive pulmonary disease: physical and psychological consequences, unmet needs, and future directions. Int J Chron Obstruct Pulmon Dis 2019;14:1127-38. [Crossref] [PubMed]
- Katzenberg G, Deacon A, Aigbirior J, et al. Management of chronic obstructive pulmonary disease. Br J Hosp Med (Lond) 2021;82:1-10. [Crossref] [PubMed]
- Ferrera MC, Labaki WW, Han MK. Advances in Chronic Obstructive Pulmonary Disease. Annu Rev Med 2021;72:119-34. [Crossref] [PubMed]
- Rhee CK. Chronic obstructive pulmonary disease research by using big data. Clin Respir J 2021;15:257-63. [Crossref] [PubMed]
- Boyer P. Chronic obstructive pulmonary disease, exacerbation and self-management: a literature review. Br J Community Nurs 2021;26:452-7. [Crossref] [PubMed]
- Sørensen KM, Leicht RV, Carlsson CJ, et al. Agreement Between Transcutaneous Monitoring and Arterial Blood Gases During COPD Exacerbation. Respir Care 2021;66:1560-6. [Crossref] [PubMed]
- Scoditti E, Massaro M, Garbarino S, et al. Role of Diet in Chronic Obstructive Pulmonary Disease Prevention and Treatment. Nutrients 2019;11:1357. [Crossref] [PubMed]
- Zysman M, Deslee G, Perez T, et al. Burden and Characteristics of Severe Chronic Hypoxemia in a Real-World Cohort of Subjects with COPD. Int J Chron Obstruct Pulmon Dis 2021;16:1275-84. [Crossref] [PubMed]
- Tousif S, Avendaño-Capriles CA, Shamim K, et al. Agreement and Correlation Between Arterial and Venous Blood pH, PO2, PCO2, Lactate, and HCO3. Cureus 2021;13:e18401. [Crossref] [PubMed]
- Ress KL, Koerbin G, Li L, et al. Reference intervals for venous blood gas measurement in adults. Clin Chem Lab Med 2020;59:947-54. [Crossref] [PubMed]
- Rang LC, Murray HE, Wells GA, et al. Can peripheral venous blood gases replace arterial blood gases in emergency department patients? CJEM 2002;4:7-15. [Crossref] [PubMed]
- Kelly AM, Kerr D, Middleton P. Validation of venous pCO2 to screen for arterial hypercarbia in patients with chronic obstructive airways disease. J Emerg Med 2005;28:377-9. [Crossref] [PubMed]
- Ak A, Ogun CO, Bayir A, et al. Prediction of arterial blood gas values from venous blood gas values in patients with acute exacerbation of chronic obstructive pulmonary disease. Tohoku J Exp Med 2006;210:285-90. [Crossref] [PubMed]
- Ibrahim I, Ooi SB, Yiong Huak C, et al. Point-of-care bedside gas analyzer: limited use of venous pCO2 in emergency patients. J Emerg Med 2011;41:117-23. [Crossref] [PubMed]
- O'Connor TM, Barry PJ, Jahangir A, et al. Comparison of arterial and venous blood gases and the effects of analysis delay and air contamination on arterial samples in patients with chronic obstructive pulmonary disease and healthy controls. Respiration 2011;81:18-25. [Crossref] [PubMed]
- McCanny P, Bennett K, Staunton P, et al. Venous vs arterial blood gases in the assessment of patients presenting with an exacerbation of chronic obstructive pulmonary disease. Am J Emerg Med 2012;30:896-900. [Crossref] [PubMed]
- Kelly AM, Klim S. Agreement between arterial and venous pH and pCO2 in patients undergoing non-invasive ventilation in the emergency department. Emerg Med Australas 2013;25:203-6. [Crossref] [PubMed]
- Sun S, Shen Y, Wang J, et al. Identification and Validation of Autophagy-Related Genes in Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis 2021;16:67-78. [Crossref] [PubMed]
- Huo X, Jin S, Wang Y, et al. DNA methylation in chronic obstructive pulmonary disease. Epigenomics 2021;13:1145-55. [Crossref] [PubMed]
- Baqdunes MW, Leap J, Young M, et al. Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Crit Care Nurs Q 2021;44:74-90. [Crossref] [PubMed]
- Müller T, Blohm JH, Dreher M, et al. Chronisch-obstruktive Lungenerkrankung, schlafbezogene Atemstörungen und Hypoventilation – Einflüsse auf das kardiorenale System Internist (Berl) 2021;62:1166-1173. [Chronic obstructive pulmonary disease, sleep-disordered breathing and hypoventilation-Influence on the cardiorenal system]. [Crossref] [PubMed]
- Lee AHY, Snowden CP, Hopkinson NS, et al. Pre-operative optimisation for chronic obstructive pulmonary disease: a narrative review. Anaesthesia 2021;76:681-94. [Crossref] [PubMed]
- Marlow LL, Lee AHY, Hedley E, et al. Findings of a feasibility study of pre-operative pulmonary rehabilitation to reduce post-operative pulmonary complications in people with chronic obstructive pulmonary disease scheduled for major abdominal surgery. F1000Res 2020;9:172. [Crossref] [PubMed]
- Libu C, Otelea MR, Arghir IA, et al. Challenges in Diagnosing Occupational Chronic Obstructive Pulmonary Disease. Medicina (Kaunas) 2021;57:911. [Crossref] [PubMed]
- Criner G, Duffy S. Reducing and managing chronic obstructive pulmonary disease exacerbations with tiotropium + olodaterol. Curr Med Res Opin 2021;37:275-84. [Crossref] [PubMed]
- Baou K, Katsi V, Makris T, et al. Beta Blockers and Chronic Obstructive Pulmonary Disease (COPD): Sum of Evidence. Curr Hypertens Rev 2021;17:196-206. [Crossref] [PubMed]
- Li A, Chan HP, Gan PXL, et al. Eosinophilic endotype of chronic obstructive pulmonary disease: similarities and differences from asthma. Korean J Intern Med 2021;36:1305-19. [Crossref] [PubMed]
- Chapman KR. Chronic Obstructive Pulmonary Disease: Is Social Injustice the Elephant in the Room? Am J Respir Crit Care Med 2021;203:1331-2. [Crossref] [PubMed]
- Crabtree TD. Bronchoscopic Valve Treatment of End-Stage Chronic Obstructive Pulmonary Disease. Thorac Surg Clin 2021;31:189-201. [Crossref] [PubMed]
- Jenkins C. Differences Between Men and Women with Chronic Obstructive Pulmonary Disease. Clin Chest Med 2021;42:443-56. [Crossref] [PubMed]
- Khemani RG, Celikkaya EB, Shelton CR, et al. Algorithms to estimate PaCO2 and pH using noninvasive parameters for children with hypoxemic respiratory failure. Respir Care 2014;59:1248-57. [Crossref] [PubMed]
- Villgran V, Gordon A, Malik K, et al. Comorbidities Associated With Chronic Obstructive Pulmonary Disease. Crit Care Nurs Q 2021;44:103-12. [Crossref] [PubMed]
- Yawn BP, Mintz ML, Doherty DE. GOLD in Practice: Chronic Obstructive Pulmonary Disease Treatment and Management in the Primary Care Setting. Int J Chron Obstruct Pulmon Dis 2021;16:289-99. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)



