
Efficacy and safety of phacoemulsification cataract surgery with prophylactic vitreous injection of bevacizumab in the treatment of retinopathy: a systematic review and meta-analysis
Introduction
Retinopathy is a relatively complex eye disease, and its specific pathogenesis is not yet clear. It can be caused by a variety of factors, such as hypertension, diabetes, age-related macular degeneration, retinal ischemia, retinitis pigmentosa, and glaucoma, which can lead to different types of retinal diseases (1-3). According to the current clinical research results, retinopathy mainly involves five basic pathological processes: (I) retinal capillary microaneurysm formation; (II) increased vascular permeability; (III) vascular occlusion; (IV) neovascularization and fibrous tissue proliferation; and (V) fibrous vascular membrane contraction (4,5). When patients develop omental lesions, they often experience a sudden drop in vision, gradual blurring of visual objects, deformation of visual objects, ghosting, reduction of visual field, fixed or floating black shadow in front of the eyes, as well as a reduction and discoloration of visual objects (6,7) (Figure 1). Therefore, once patients suffer retinopathy, they should be treated promptly to avoid worsening vision and recovery failure.
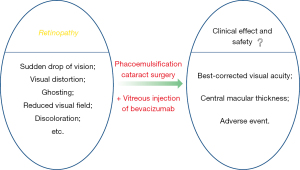
Clinically, the therapeutic methods for retinal diseases mainly include surgical treatment [such as phacoemulsification and laser photocoagulation (8,9)], drug treatment [such as bevacizumab, ranibizumab, triamcinolone acetonide (10,11)], and targeted combination therapy (12,13). Moreover, for retinopathy caused by different factors, clinicians typically choose the corresponding treatment methods according to the actual condition of patients, so as to achieve a more successful treatment effect (14). For example, for patients with cataracts and retinopathy, clinicians usually employ phacoemulsification for cataract treatment. According to some previously reported research results, this treatment method can effectively improve the course and progress of retinopathy patients. However, according to relevant study, about 20% of patients will have an increase in central retinal thickness after phacoemulsification (15). Therefore, an increasing number of clinicians have explored the comprehensive therapy of phacoemulsification cataract surgery combined with drug treatment, and offered some research progress (16-18). Among them, anti-vascular endothelial growth factor (anti-VEGF) treatment for cataracts may be a reasonable intervention to prevent complications related to the progression of retinopathy. As a humanized monoclonal antibody, bevacizumab (Avastin) can effectively inhibit all subtypes of VEGF-A (19). At present, relevant studies have evaluated the efficacy and safety of intravitreal bevacizumab (IVB) prior to phacoemulsification (20-22). However, the scientific evidence of a single study may be limited by small samples, as well as different populations, follow-up periods, and surgical techniques. Therefore, the purpose of this study is to provide more reliable clinical evidence for clinicians through the meta-analysis of the clinical efficacy and safety of phacoemulsification and cataract surgery with prophylactic vitreous injection of bevacizumab in the treatment of retinopathy. We present the following article in accordance with the PRISMA reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-222/rc).
Methods
Data source and search strategy
We searched the PubMed, Web of Science, Embase, and MEDLINE literature databases for English language articles published between 2001 and 2022. The literature retrieval methods involved rapid retrieval of English words and combinatorial retrieval of literature keywords. The search keywords were as follows: “vitreous injection”, “bevacizumab”, “phacoemulsification cataract surgery”, “retinopathy”, “clinical efficacy”, “safety”, and “randomized controlled trial”. The free combination of these keywords was used for database full-text retrieval. At the same time, the relevant citations were tracked by manual retrieval. The literature search and retrieval was conducted on January 30, 2022.
Inclusion criteria
The inclusion criteria were as follows: (I) randomized controlled study on the clinical effect and safety evaluation of prophylactic IVB combined with phacoemulsification for the treatment of retinopathy; (II) studies with complete and relevant data and those in which the intervention group was comparable with the control group; (III) the intervention measures involved experimental group patients being treated with phacoemulsification cataract surgery combined with prophylactic intravitreal injection of bevacizumab, while the control group patients underwent cataract surgery alone in addition to a placebo; (IV) studies in which all patients receiving similar conventional treatment did not undergo bevacizumab intervention treatment postoperatively or during follow-up; and (V) studies that included the main outcome indicators outlined in this paper.
Exclusion criteria
The exclusion criteria were as follows: (I) studies involving non-cataract patients complicated with retinopathy; (II) non-randomized controlled trials; (III) articles with incomplete data or those that could not provide the relevant data outlined in this paper for analysis; and (IV) studies involving patients with a history of ophthalmic surgery who suffered from inflammation and other eye diseases, as well as those with intraoperative complications, such as posterior capsule rupture and severe iris injury.
Literature selection
Two researchers independently performed the literature screening. After reading the titles and abstracts, we excluded studies that obviously did not meet the inclusion criteria. We then obtained and read the full texts of the remaining articles for further screening. Two researchers performed crosschecking, and a third person was introduced to assist in arbitration in questionable cases regarding the inclusion of studies that could not be resolved by discussion.
Data extraction
Two researchers independently extracted and evaluated the relevant data and methodological quality of the articles included in this study, including: the first author, year of literature publication, geographical location of the study, intervention measures, follow-up time, main inclusion and exclusion criteria, number of eyes in each group, average age and gender of patients, follow-up period, withdrawal ratio, and duration of the disease. Two researchers performed crosschecking of the extracted data. In case of divergent opinions, a comprehensive evaluation was conducted by a third party. If the data could not be obtained, the literature was excluded.
Literature quality assessment
The Newcastle-Ottawa Scale (NOS score method) was used for treatment evaluation, with higher scores indicating better quality literature and less bias. Among the included studies, four articles scored 6 points, one article scored 5 points, and one article scored 4 points.
Statistical analysis
RevMan5.3 software provided by Cochrane Collaboration Network was used for meta-analysis. The weighted mean difference (MD) and 95% confidence interval (CI) were used to report the combined effect, and a forest map was used to display the results. The Q test was used to evaluate the heterogeneity between the research results. If there was no statistical heterogeneity (P>0.1; I2≤50%), the fixed effects model is used to analyze the data. If there was statistical heterogeneity (P≤0.1; I2>50%), the included data was preliminarily analyzed and evaluated. We then judged whether there was obvious research or methodological heterogeneity by reading the full texts of the included literature several times. Subsequently, sensitivity analysis of the outcome indicators of each study was carried out one-by-one, and the new data were combined after eliminating the unqualified studies. Finally, we checked whether the overall effect amount had changed. If the result after each elimination was the same as the previous total consolidation result, this indicates that the result was relatively stable. If the above methods could not explain the causes of heterogeneity, the data was combined and analyzed using the random effects model. P<0.05 was considered statistically significant for all of the above effect analyses.
Results
Literature search and screening results
In this study, 489 literatures relevant literatures were initially retrieved. Of these, 358 repetitive and irrelevant articles were removed. After reading the titles and abstracts of the remaining studies, a further 98 literatures that did not meet the inclusion criteria were removed. Subsequently, after intensive reading of the full texts of the remaining articles, 17 studies were excluded because the full text could not be retrieved, and a further 10 articles with incomplete data, those in which the data was unable to be converted, and non-randomized controlled trials were excluded. Finally, six literatures were included, with a total 325 cataract and retinopathy patients (Figure 2). The basic characteristics, common risk factors, and literature quality scores of the included articles are shown in Table 1.
Table 1
Basic characteristics of literatures
According to the retrieval strategy described in 1.1 above, six articles with a total of 325 cataract and retinopathy patients were included in this study. There were 163 cases in the drug intervention group and 162 cases in the control group. There were no significant differences in the average age, sex ratio, and course of disease between the two groups. The basic characteristics and NOS scores of the included articles are shown in Table 2.
Table 2
| Serial number | Author | Study location | Date of publication | Total cases | Main evaluation indicators | Quality score (points) |
|---|---|---|---|---|---|---|
| 1 | Salehi et al. (27) | Shahrekord, Iran | 2012 | 57 | (I), (II), (III), (IV), (V), (VI) | 6 |
| 2 | Khodabandeh et al. (28) | Tehran, Iran | 2018 | 71 | (I), (II), (IV), (V), (VIII), (IX) | 6 |
| 3 | Takamura et al. (29) | Japan | 2009 | 61 | (I), (II), (IV), (V), (VII) | 5 |
| 4 | Cheema et al. (30) | United Kingdom | 2009 | 68 | (I), (II), (III), (IV), (V), (VI) | 6 |
| 5 | Fard et al. (31) | Tehran, Iran | 2011 | 42 | (I), (II), (III), (IV), (V), (VI) | 6 |
| 6 | Lanzagorta-Aresti et al. (32) | Valencia, Spain | 2009 | 26 | (II), (III), (V), (VI) | 4 |
Main evaluation indicators: (I) best-corrected visual acuity at 1 month; (II) best-corrected visual acuity at 3 months; (III) best-corrected visual acuity at 6 months; (IV) central macular thickness at 1 month; (V) central macular thickness at 3 months; (VI) central macular thickness at 6 months; (VII) intraocular pressure; (VIII) postoperative macular edema; (IX) total macular volume.
Meta-analysis results
Best-corrected visual acuity at 1 month
Five studies (27-31) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification cataract surgery in the treatment of retinopathy at 1 month, including a total of 150 cases in the bevacizumab intervention group and 149 cases in the control group. There was heterogeneity among the articles (I2=79%; P=0.0009), and no cause of heterogeneity was found after analysis, so the random effect model was used for data analysis. The results showed that the best-corrected visual acuity of the bevacizumab intervention group was superior to that of the control group at 1 month after treatment, and the difference was statistically significant [MD =−0.06; 95% CI: (−0.09, −0.03); P=0.0002] (Figure 3).
Best-corrected visual acuity at 3 months
Six studies (27-32) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification in the treatment of retinopathy at 3 months, including a total of 163 cases in the bevacizumab intervention group and 162 cases in the control group. There was heterogeneity among the articles (I2=66%; P=0.01), and no cause of heterogeneity was found through analysis, so the random effect model was used for data analysis. The results showed that the best-corrected visual acuity of bevacizumab intervention group was better than that of the control group at 3 months after treatment, and the difference was statistically significant [MD =−0.09; 95% CI: (−0.11, −0.07); P<0.00001] (Figure 4).
Best-corrected visual acuity at 6 months
Four studies (27,30-32) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification cataract surgery for retinopathy at 6 months, including a total of 106 cases in bevacizumab intervention group and 106 cases in control group. There was heterogeneity among the literatures (I2=80%; P=0.002), and no cause of heterogeneity was found through analysis, so the random effect model was used for data analysis. The results showed that the best-corrected visual acuity of bevacizumab intervention group was slightly better than that of the control group at 6 months after treatment, although the difference was not significant and statistically significant [MD =−0.02; 95% CI: (−0.07, 0.03); P=0.39] (Figure 5).
Central macular thickness at 1 month
Five studies (27-31) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification cataract surgery in the treatment of retinopathy at 1 month, including a total of 150 cases in the bevacizumab intervention group and 149 cases in the control group. There was heterogeneity among the literatures (I2=95%; P<0.00001), and no cause of heterogeneity was found after analysis, so the random effect model was used for data analysis. The results showed that the central macular thickness in the bevacizumab intervention group was smaller than that in the control group at 1 month after treatment, and the difference was statistically significant [MD =−37.07; 95% CI: (−45.87, −28.27); P<0.00001] (Figure 6).
Central macular thickness at 3 months
Six studies (27-32) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification in the treatment of retinopathy at 3 months, including a total of 163 cases in the bevacizumab intervention group and 162 cases in the control group. There was heterogeneity among the literatures (I2=97%; P<0.00001), and no cause of heterogeneity was found through analysis, so the random effect model was used for data analysis. The results showed that the central macular thickness in the bevacizumab intervention group was smaller than that in the control group at 3 months after treatment, and the difference was statistically significant [MD =−15.26; 95% CI: (−23.87, −6.66); P=0.0005] (Figure 7).
Central macular thickness at 6 months
Four studies (27,30-32) reported on the clinical effect of vitreous injection of bevacizumab combined with phacoemulsification cataract surgery for retinopathy at 6 months, including a total of 106 cases in bevacizumab intervention group and 106 cases in control group. There was heterogeneity among the literatures (I2=57%; P=0.07), and no cause of heterogeneity was found after analysis, so the random effect model was used for data analysis. The results showed that the central macular thickness in the bevacizumab intervention group was lower than that in the control group at 6 months after treatment, and the difference was statistically significant [MD =−26.77; 95% CI: (−37.51, −16.04); P<0.00001] (Figure 8).
Adverse events
No severe ocular and adverse events related to IVB were reported during the follow-up periods in the six included studies.
Analysis of publication bias
Publication bias analysis was not performed due to the small number of articles included in this study.
Discussion
Retinopathy typically refers to a microvascular disease that manifests as obstruction, exudation, and proliferation as its main clinical characteristics. Its development is highly correlated with the reduction of peripheral cells of capillaries, basement membrane thickening, and endothelial cell proliferation, and is accompanied by typical blood flow characteristics in the development process, which further causes retinal hypoxia and promotes VEGF stimulation of neovascularization. Finally, it causes the rupture of ocular blood vessels, bleeding, and accelerated decline of visual acuity (33). This will not only result in an enormous physical and psychological burden on patients, but also have a significant impact on their quality of life. Therefore, the clinical value and research significance of effective intervention through modern medical techniques and drug treatment is critical to improving the survival of cataract patients complicated with retinopathy.
At present, the treatment of cataracts complicated with retinal diseases mainly includes phacoemulsification, retinal laser photocoagulation, intravitreal injection of drugs, and vitrectomy (34,35). Although these methods can occlude and contract the dilated capillaries to a certain extent, the efficacy of using one method alone is often not ideal, and may even aggravate the prognostic effects, such as macular edema and slow visual recovery. Therefore, the majority of clinicians and ophthalmologists have continued to explore a variety of combined treatment methods. Among these, phacoemulsification or retinal laser photocoagulation combined with intravitreal injection of steroids or anti-VEGF drugs can significantly improve retinal microcirculation, improve postoperative corrected visual acuity, reduce central macular thickness, and achieve a certain prognostic effect. However, because these combined therapies are still in various stages of clinical research, more randomized, prospective, large sample trials are needed to comprehensively evaluate their exact clinical efficacy and safety.
Clinically, the treatment effect of cataract patients with retinopathy usually involves improvement of the best-corrected visual acuity, central macular thickness, intraocular pressure changes, the incidence of postoperative macular edema, and the total volume of the macula, etc. Among these, the improvement of patients’ best-corrected visual acuity and the change in central macular thickness are the key indicators to evaluate the effect of treatment (36). The improvement of best-corrected visual acuity directly reflects the therapeutic effect of patients with cataracts and retinopathy. Generally, the more successful the surgical treatment of patients, the better the improvement of patients’ best-corrected visual acuity, and vice versa. Also, the postoperative thickness of the central macula of the eye is also related to the treatment effect. Therefore, these two aspects were selected as the primary indicators in this systematic review and meta-analysis.
The results of this meta-analysis showed that the best-corrected visual acuity of the preventive vitreous injection bevacizumab intervention group was significantly better than that of the control group at 1 and 3 months after treatment. In addition, the central macular thickness at 1, 3, and 6 months were significantly lower in the preventive vitreous injection of bevacizumab intervention group compared to those in the control group. Therefore, these data comprehensively demonstrate that prophylactic intravitreal injection of bevacizumab combined with phacoemulsification has a good clinical effect in the treatment of cataract patients with retinopathy.
Conclusions
A total of six articles were included in this systematic review and meta-analysis of phacoemulsification with prophylactic vitreous injection of bevacizumab in the treatment of retinopathy. The results showed that patients with cataracts complicated with retinopathy who underwent prophylactic intravitreal injection of bevacizumab combined with phacoemulsification had significantly improved best-corrected visual acuity and central macular thickness, and had a good clinical therapeutic effect. At the same time, the combined treatment had high safety as well as almost no adverse reactions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-222/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-222/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhang W, Chen S, Liu ML. Pathogenic roles of microvesicles in diabetic retinopathy. Acta Pharmacol Sin 2018;39:1-11. [Crossref] [PubMed]
- Kovach JL, Isildak H, Sarraf D. Crystalline retinopathy: Unifying pathogenic pathways of disease. Surv Ophthalmol 2019;64:1-29. [Crossref] [PubMed]
- Gillow JT, Gibson JM, Dodson PM. Hypertension and diabetic retinopathy--what's the story? Br J Ophthalmol 1999;83:1083-7. [Crossref] [PubMed]
- Campochiaro PA. Molecular pathogenesis of retinal and choroidal vascular diseases. Prog Retin Eye Res 2015;49:67-81. [Crossref] [PubMed]
- Yang S, Zhang J, Chen L. The cells involved in the pathological process of diabetic retinopathy. Biomed Pharmacother 2020;132:110818. [Crossref] [PubMed]
- Montiani-Ferreira F, Li T, Kiupel M, et al. Clinical features of the retinopathy, globe enlarged (rge) chick phenotype. Vision Res 2003;43:2009-18. [Crossref] [PubMed]
- Huang CH, Hsieh YT, Yang CM. Vitrectomy for complications of proliferative diabetic retinopathy in young adults: clinical features and surgical outcomes. Graefes Arch Clin Exp Ophthalmol 2017;255:863-71. [Crossref] [PubMed]
- Furino C, Ferrara A, Cardascia N, et al. Combined cataract extraction and intravitreal bevacizumab in eyes with choroidal neovascularization resulting from age-related macular degeneration. J Cataract Refract Surg 2009;35:1518-22. [Crossref] [PubMed]
- Choi AY, Cho H, Kim YC. Effect of two different doses of intravitreal bevacizumab with temporal retina-sparing laser photocoagulation for retinopathy of prematurity. Int J Ophthalmol 2018;11:166-9. [PubMed]
- Campochiaro PA, Akhlaq A. Sustained suppression of VEGF for treatment of retinal/choroidal vascular diseases. Prog Retin Eye Res 2021;83:100921. [Crossref] [PubMed]
- Sarao V, Veritti D, Boscia F, et al. Intravitreal steroids for the treatment of retinal diseases. ScientificWorldJournal. 2014;2014:989501. [Crossref] [PubMed]
- Ran J, Zhou J. Targeting the photoreceptor cilium for the treatment of retinal diseases. Acta Pharmacol Sin 2020;41:1410-5. [Crossref] [PubMed]
- Nicolò M, Ferro Desideri L, Vagge A, et al. Faricimab: an investigational agent targeting the Tie-2/angiopoietin pathway and VEGF-A for the treatment of retinal diseases. Expert Opin Investig Drugs 2021;30:193-200. [Crossref] [PubMed]
- Viswanath K, McGavin DD. Diabetic retinopathy: clinical findings and management. Community Eye Health 2003;16:21-4. [PubMed]
- Kim SJ, Equi R, Bressler NM. Analysis of macular edema after cataract surgery in patients with diabetes using optical coherence tomography. Ophthalmology 2007;114:881-9. [Crossref] [PubMed]
- Gupta PC, Ram J, Kumar MP, et al. Effect of sustained-release long-acting intravitreal dexamethasone implant in patients of non-proliferative diabetic retinopathy undergoing phacoemulsification: A randomized controlled trial. Indian J Ophthalmol 2021;69:3263-72. [Crossref] [PubMed]
- Sze AM, Luk FO, Yip TP, et al. Use of intravitreal dexamethasone implant in patients with cataract and macular edema undergoing phacoemulsification. Eur J Ophthalmol 2015;25:168-72. [Crossref] [PubMed]
- Furino C, Boscia F, Niro A, et al. Diabetic Macular Edema and Cataract Surgery: Phacoemulsification Combined With Dexamethasone Intravitreal Implant Compared With Standard Phacoemulsification. Retina 2021;41:1102-9. [Crossref] [PubMed]
- Belin PJ, Lee AC, Greaves G, et al. The use of bevacizumab in pediatric retinal and choroidal disease: A review. Eur J Ophthalmol 2019;29:338-47. [Crossref] [PubMed]
- Zhao LQ, Cheng JW. A Systematic Review and Meta-Analysis of Clinical Outcomes of Intravitreal Anti-VEGF Agent Treatment Immediately after Cataract Surgery for Patients with Diabetic Retinopathy. J Ophthalmol 2019;2019:2648267. [Crossref] [PubMed]
- Hernández-Da Mota SE, Chacón-Lara A, Hernández-Vázquez E. Use of triamcinolone and bevacizumab in 25G phaco-vitrectomy surgery for the treatment of cataract and diabetic macular edema. Arch Soc Esp Oftalmol 2008;83:293-300. [Crossref] [PubMed]
- Palkovits S, Seidel G, Pertl L, et al. Macular choroidal volume changes after intravitreal bevacizumab for exudative age-related macular degeneration. Retina 2017;37:2262-8. [Crossref] [PubMed]
- Akinci A, Batman C, Ozkilic E, et al. Phacoemulsification with intravitreal bevacizumab injection in diabetic patients with macular edema and cataract. Retina 2009;29:1432-5. [Crossref] [PubMed]
- Jonas JB, Spandau UH, Schlichtenbrede F, et al. Intravitreal bevacizumab combined with cataract surgery for treatment of exudative macular degeneration. J Ocul Pharmacol Ther 2007;23:599-600. [Crossref] [PubMed]
- Altintas AGK, Ilhan C. Intravitreal Dexamethasone Implantation in Intravitreal Bevacizumab Treatment-resistant Pseudophakic Cystoid Macular Edema. Korean J Ophthalmol 2019;33:259-66. [Crossref] [PubMed]
- Wahab S, Ahmed J. Management of cataract with macular oedema due to diabetes mellitus type-II and hypertension with grid laser prior to surgery and intra-vitreal bevacizumab (Avastin) peroperatively. J Pak Med Assoc 2010;60:836-9. [PubMed]
- Salehi A, Beni AN, Razmjoo H, et al. Phacoemulcification with intravitreal bevacizumab injection in patients with cataract and coexisting diabetic retinopathy: prospective randomized study. J Ocul Pharmacol Ther 2012;28:212-8. [Crossref] [PubMed]
- Khodabandeh A, Fadaifard S, Abdollahi A, et al. Role of combined phacoemulsification and intravitreal injection of bevacizumab in prevention of postoperative macular edema in non-proliferative diabetic retinopathy. J Curr Ophthalmol 2018;30:245-9. [Crossref] [PubMed]
- Takamura Y, Kubo E, Akagi Y. Analysis of the effect of intravitreal bevacizumab injection on diabetic macular edema after cataract surgery. Ophthalmology 2009;116:1151-7. [Crossref] [PubMed]
- Cheema RA, Al-Mubarak MM, Amin YM, et al. Role of combined cataract surgery and intravitreal bevacizumab injection in preventing progression of diabetic retinopathy: prospective randomized study. J Cataract Refract Surg 2009;35:18-25. [Crossref] [PubMed]
- Fard MA, Yazdanei Abyane A, Malihi M. Prophylactic intravitreal bevacizumab for diabetic macular edema (thickening) after cataract surgery: prospective randomized study. Eur J Ophthalmol 2011;21:276-81. [Crossref] [PubMed]
- Lanzagorta-Aresti A, Palacios-Pozo E, Menezo Rozalen JL, et al. Prevention of vision loss after cataract surgery in diabetic macular edema with intravitreal bevacizumab: a pilot study. Retina 2009;29:530-5. [Crossref] [PubMed]
- Lechner J, O'Leary OE, Stitt AW. The pathology associated with diabetic retinopathy. Vision Res 2017;139:7-14. [Crossref] [PubMed]
- Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification-a review of the literature. Eye (Lond) 2020;34:616-31. [Crossref] [PubMed]
- Dou X, Duerfeldt AS. Small-Molecule Modulation of PPARs for the Treatment of Prevalent Vascular Retinal Diseases. Int J Mol Sci 2020;21:9251. [Crossref] [PubMed]
- Bamahfouz A. Correlation of Central Macular Thickness and the Best-Corrected Visual Acuity in Three Months After Cataract Surgery by Phacoemulsification and With Intraocular Lens Implantation. Cureus 2021;13:e13856. [Crossref] [PubMed]
(English Language Editor: A. Kassem)









