Effect of acupuncture treatment on dysphagia caused by pseudobulbar paralysis after stroke: a systematic review and meta-analysis
Introduction
Pseudobulbar paralysis is a common complication after stroke, with an incidence of more than 51% (1). It is caused by upper limb motor injury due to bilateral cortical tract disorders and is characterized by dysphagia, dysphonia, weakness of face and tongue, and emotional instability (2,3). Dysphagia caused by pseudobulbar paralysis affects daily eating and increases the risk of aspiration pneumonia as well as disability and mortality (4,5). Pseudobulbar paralysis lacks specific treatment, which is an urgent problem to be solved at present. Although there are some rehabilitation treatments for dysphagia caused by pseudobulbar paralysis, the efficacy varies greatly. Since dysphagia is multidimensional, a multidisciplinary and comprehensive approach is needed.
The research on acupuncture treatment of dysphagia caused by pseudobulbar paralysis has increased, but the results are not consistent. Moreover, there is a lack of conclusive evidence at present. Given the increasing number of randomized controlled trials (RCTs) of acupuncture for dysphagia caused by pseudobulbar paralysis, we conducted a systematic review and meta-analysis of the existing evidence to examine and explore the effect of acupuncture in dysphagia caused by pseudobulbar paralysis after stroke. We present the following article in accordance with the PRISMA reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3551/rc).
Methods
The protocol has been registered on the PROSPERO platform (CRD42022306827).
Search strategy
We performed the literature search in PubMed, Web of Science, Embase, Cochrane, Chinese BioMedical Literature Database (CBM), China National Knowledge Infrastructure (CNKI), WanFang Data, Chinese Science and Technology Periodicals database (VIP), Open Grey online database, to identify relevant studies from the establishment of the database to October 1, 2020. The following terms individually or in combination were used to identify the potential articles: “pseudobulbar palsy”, “pseudobulbar paralysis”, “stroke”, “stroke sequelae”, “cerebral infarction”, “hemorrhagic stroke”, “cerebrovascular accident”, “ischemic stroke”, “acupuncture”, “scalp acupuncture”, “electroacupuncture”, “tongue needle”, “Jin’s three needles”, “pricking blood”, “body acupuncture”, and “rehabilitation training”. The grey literature was searched using the Open Grey online database. The search was limited to English or Chinese. Besides, a manual search was carried out on included studies or conference abstracts to identify any ongoing studies or trial registries. All the studies have been rigorously evaluated.
Study selection
Studies were included if they met the following criteria: (I) study design: RCTs; (II) intervention: acupuncture with or without rehabilitation; (III) comparison: rehabilitation treatment without acupuncture; (IV) population: diagnosed as dysphagia caused by pseudobulbar paralysis after stroke, regardless of age, sex or race; (V) outcome: the number of patients who substantially recovered, markedly effective, effective and invalid in the intervention and control groups. We excluded non-RCTs, animal studies, prospective studies, case-control studies, cross-sectional studies, letters, reviews, commentaries, and studies that dysphagia not related to pseudobulbar paralysis after stroke or other unknown diseases. If the study was reported more than once, we would use the latest results. In the course of this work, any differences between the two authors need to be discussed with the third author (DHX) to reach a consensus.
Data extraction and quality management
Two groups of four investigators (PW and XMM, JH and JXL) independently reviewed and extracted relevant data from each included report. We extracted the following information: authors, publication year, number of patients, intervention duration, participant characteristics, intervention, acupoints, comparison, efficacy evaluation criteria, and drop-out rate. All results were displayed in the form of figures or tables. Adverse events were also collected from the included studies. The same investigators also assessed the risk of bias from each included study using the Cochrane risk of bias tool. Any differences were resolved by discussion and consensus.
Data synthesis and analysis
Meta-analysis of RCTs with available data was performed by calculating the effect size [risk ratio (RR)] and 95% confidence interval (CI) using the random-effect models and the Mantel-Haenszel (M-H) method.
The detailed calculation method is shown in Table 1.
Table 1
| Group | N | Substantially recovered | Markedly effective | Effective | Invalid |
|---|---|---|---|---|---|
| Intervention | N2 | A2 | B2 | C2 | D2 |
| Control | N1 | A1 | B1 | C1 | D1 |
N2: total number of intervention group; A2: substantially recovered number of intervention group; B2: markedly effective number of intervention group; C2: effective number of intervention group; D2: invalid number of intervention group; N1: total number of control group; A1: substantially recovered number of control group; B1: markedly effective number of control group; C1: effective number of control group; D1: invalid number of control group. RR, risk ratio.
The significant effective size: .
The total effective size: .
Heterogeneity was considered statistically significant at I2>50%. To explore the heterogeneity and stability of the results, we carried out sensitivity analyses. In addition, we conducted subgroup analyses to explore the effects of different interventions.
Publication bias was assessed by visual inspection of funnel plots and formal testing by Egger’s and Begg’s test if more than 10 studies were included.
Statistical analysis
StataSE 12.0 software (StataCorp, USA), and Review Manager 5.3 software (Cochrane collaboration network) were adopted to merge the statistics of the included articles.
Results
Search results
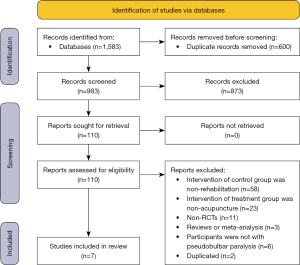
A total of 1,583 studies were identified by the initial database research. Six hundred studies were excluded because of duplication, and 873 studies were excluded based on the titles and or abstracts. The remaining 110 full-text reports were reviewed for more detailed evaluation. available online: https://cdn.amegroups.cn/static/public/apm-21-3551-01.pdf listed the reasons for excluded articles: the intervention of comparison is non-rehabilitation (n=58); the intervention of treatment group is non-acupuncture or non-acupuncture combined with rehabilitation (n=23); non-RCTs (n=11); reviews or meta-analysis (n=3); participants are not with pseudobulbar paralysis (n=6); duplicated (n=2). Finally, seven RCTs that met our eligibility criteria were included in the present meta-analysis (6-12). The selection process for RCTs included in the meta-analysis is shown in Figure 1.
Methodological quality assessment
We conducted a graphical summary of bias risk assessment for the 7 included studies (Figures S1,S2). Of these, patients were randomized using a random number table in 5 studies (8-12). The remaining 2 studies referred to“randomization” but did not describe specific randomization methods (6,7). None of the literature described allocation concealment. Due to the nature of acupuncture, blinding of participants and personnel was not attempted in any articles. Only one study clearly stated that results were assessed blindly by a third-party organization (12). All the included literature had complete data for analysis. Except for Yuan’s study, 6 studies have not provided the protocol of its main and secondary outcomes, which were judged as an unknown risk of reporting bias. Other bias was assessed as low risk in all.
Characterization of included studies
Table 2 showed the characteristics of all included trials (7 studies with 637 participants) assessing the effect of acupuncture treatment in individuals with dysphagia caused by pseudobulbar paralysis after stroke. The average duration of symptoms for all trials was 48 days. The average sample size was 79. Most of the participants were older (the average age was 64 years). The average duration of intervention across all trials was 26 days.
Table 2
| Study | Age (years) | Duration of symptoms (days) | No. of patients (T/C) | Intervention (whether combined with R) | Control (rehabilitation) | Duration of intervention (days) | Drop-out rate (%) | Efficacy evaluation criteria |
|---|---|---|---|---|---|---|---|---|
| Liu, 2009 (6) | T: 59.2; C: 57.4 | T: 63; C: 66 | 82 (42/40) | Y | 3, 4 | 30 | 0 | I |
| Liu & Zhao, 2014 (7) | T: 70.22±6.60; C: 69.75±6.85 | T: 19.75±6.12; C: 20.50±5.88 | 64 (32/32) | Y | 4, 6, 7 | 21 | 0 | I, II |
| Wang, 2017 (8) | T: 65.04; C: 65.73 | T: 27.01; C: 26.12 | 135 (90/45) | N | 2, 3, 4, 5, 8 | 24 | 0 | III, IV |
| Chu, 2017 (9) | T: 67±11; C: 67±10 | T: 41.1±38.6; C: 40.5±30.8 | 97 (48/49) | Y | 1, 2, 3, 4, 5 | 40 | 3 | II, III, V |
| Cao-1, 2019 (10) | T: 60.30±8.75; C: 57.25±10.38 | T: 85.5±49.5; C: 110.7±44.7 | 58 (30/28) | Y | 1, 2 | 20 | 0 | I |
| Cao-2, 2019 (10) | T: 62.66±8.54; C: 57.25±10.38 | T: 96.3±46.8; C: 110.7±44.7 | 60 (32/28) | N | 1, 2 | 20 | 0 | I |
| Liu & Chen, 2019 (11) | T: 66.2±11.3; C: 65.9±10.9 | T: 42; C: 32 | 94 (47/47) | Y | 1, 2, 3, 4, 5 | 40 | 0 | II, III, V, VI |
| Yuan, 2020 (12) | T: 63.29±8.91; C: 62.84±7.54 | T: 16.5; C: 15.0 | 75 (38/37) | N | 2, 3, 5 | 14 | 0 | II, VII |
1: cold stimulation; 2: vocalization training; 3: swallowing training; 4: tongue muscle training; 5: ingestion training; 6: soft palate lift training; 7: masticatory muscle training; 8: swallowing reflex training. I: KTST; II: SWAL-QOL; III: SSA; IV: NIHSS; V: RSST; VI: MWST; VII: Fujishima Ichiro Swallowing Efficacy Score. T, Treatment; C, Control; R, Rehabilitation; Y, Yes; N, No; KTST, Kubota Toshio Drinking Water Test; SWAL-QOL, Swallow Quality-of-Life Questionnaire; SSA, Standard Swallowing Function Score; NIHSS, National Institute of Health Stroke Scale; RSST, Repeated Saliva Swallowing Test; MWST, Modified Water Swallowing Test.
The types of intervention used in all included studies were single acupuncture (8,10,12), or acupuncture combined with rehabilitation (6,7,9-11). Acupoints contain GB20, CV23, CV22, EX-HN12, etc., of which GB20 is mandatory (Table S1). The rehabilitation treatment methods included could stimulation, vocalization training, swallowing training, tongue muscle training, ingestion training, soft palate lift training, masticatory muscle training, swallowing reflex training.
There were seven criteria for evaluating the curative effect, including Kubota Toshio Drinking Water Test (KTST), Swallow Quality-of-Lift Questionnaire (SWAL-QOL), Standard Swallowing Function Score (SSA), National Institute of Health Stroke Scale (NIHSS), Repeated Saliva Swallowing Test (RSST), Modified Water Swallowing Test (MWST), Fujishima Ichiro Swallowing Efficacy Score (FISES).
The drop-out rate of all studies was 0, except that Chu et al. (9) was 3% (2 cases in the intervention group and 1 case in the control group were caused by recurrence and aggravation of cerebrovascular accident).
Efficacy of acupuncture
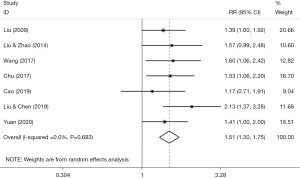
Seven studies reported the effective rate of acupuncture for dysphagia caused by pseudobulbar palsy after stroke. As shown in Figure S3, acupuncture had a significant effect on improving the total effective rate of dysphagia with substantial heterogeneity (RRtotal =1.13; 95% CI: 1.02–1.25; I2=64.4%). Surprisingly, acupuncture markedly increased the significant effective rate of dysphagia without heterogeneity (Figure 2; RRsig =1.51; 95% CI: 1.30–1.75; I2=0%). In the following, we focus on the research of RRsig.
Subgroup analyses
According to whether the intervention group was combined with rehabilitation, we conducted subgroup analyses. In the subgroup of acupuncture + rehabilitation vs. rehabilitation, the RRsig was 1.56 (95% CI: 1.30–1.87; I2=0%) using the random-effects model (Figure S4); in the subgroup of acupuncture vs. rehabilitation, the RRsig was 1.38 (95% CI: 1.08–1.76; I2=0.8%) using the random-effects model (Figure S4). Therefore, acupuncture combined with rehabilitation shows a better effect on dysphagia.
Sensitivity analyses
As shown in Figure S5, we implemented sensitivity analyses by systematically omitting a single study step by step, and the result did not change, indicating that our result was stable.
Publication bias analyses
Publication bias was not assessed for outcome since fewer than 10 articles were included.
Adverse events
All of the included trials provided information on adverse events, and only two of them had adverse events. Wang et al. (8) reported that pneumonia (control group 7/45; intervention group: 7/90), asphyxia (control group 6/45; intervention group: 2/90), dehydration (control group 7/45; intervention group: 11/90), and malnutrition occurred (control group 5/45; intervention group: 8/90). Yuan et al. (12) reported that 10 participants (control group 4/37; intervention group: 6/38) had mild pain during treatment but did not affect follow-up treatment. Other adverse events were not reported.
Discussion
This is a systematic review and meta-analysis of seven RCTs to evaluate the efficacy of acupuncture compared with rehabilitation in patients with dysphagia caused by pseudobulbar paralysis after stroke. The present meta-analysis demonstrates that acupuncture can significantly improve the dysphagia caused by pseudobulbar paralysis after stroke, and acupuncture combined with rehabilitation shows a better effect.
Bulbar paralysis is a kind of low motor neuron paralysis that affects the nuclei of IX, X, XI, and XII of cerebral nerves. In contrast, pseudobulbar paralysis is upper motor neuron paralysis that affects the cortical bulbar bundles of the V, VII, IX, X, XI, and XII. Any injury to the nucleus or cortical tract can lead to medulla oblongata or pseudobulbar paralysis (e.g., stroke, multiple sclerosis, infection, brainstem tumor) (13-15). Bulbar paralysis and pseudobulbar paralysis are mainly seen in men over 75 years old, characterized by dysarthria and dysphagia (16,17). Acupuncture has been the primary medical intervention for stroke and stroke-related complications in China and other parts of East Asia, and the effect is significant (18). There have been numerous meta-analyses on acupuncture in treating dysphagia after stroke, which has proved that acupuncture was an effective method for treating dysphagia after stroke (19-23). However, these meta-analyses did not separate pseudobulbar paralysis from true bulbar paralysis. Our meta-analysis is the first to identify pseudobulbar palsy, demonstrating the superiority of acupuncture in this condition and providing evidence-based evidence for precise clinical treatment.
Expectedly, our subgroup analyses shows that acupuncture combined with rehabilitation is more effective than that acupuncture without rehabilitation. The clinical application of this result can reasonably explain that if the hospital does not have enough rehabilitation measures, acupuncture can improve dysphagia. What is more, if there is adequate rehabilitation treatment, the addition of acupuncture is more effective.
The mechanism of acupuncture stimulation is considered to be closely related to the nervous system and is expected to improve neurological function after stroke (24). Acupuncture treatment of dysphagia caused by pseudobulbar paralysis after stroke may be related to the swallowing cortex’s excitement (25). Also, acupuncture can promote the establishment of collateral circulation and angiogenesis, improve nerve function, regulate inflammatory factors, regulate the production of inflammatory factors, growth factors, and transcription factors, and effectively reduce nerve injury (26,27). In addition, some animal experiments and clinical trials show that acupuncture mainly regulates the release of neurotransmitters, improves cerebral microcirculation, protects neurons, inhibits inflammation, and so on (28-31).
GB20 and CV23 have become the most frequently used acupoints in the included studies. Therefore, acupuncture in these two acupoints may help to improve dysphagia caused by pseudobulbar paralysis after stroke. According to the standard acupoints of the World Health Organization (WHO Western Pacific Regional Office, 2008), GB20 is located at the back of the neck, suboccipital depression, between the origin of the sternocleidomastoid muscle and the trapezius muscle, and the surrounding anatomical tissue includes the sternocleidomastoid muscle, trapezius muscle, head clamp muscle and branches of the lesser occipital nerve. Another important acupoint CV23 was located in the anterior part of the cervical midline, above Adam’s tubercle, and in the depression of the superior margin of the hyoid bone. The surrounding anatomical tissues include the suprahyoid muscle, facial nerve, glossopharyngeal nerve, hypoglossal nerve branch, and vagus nerve branch. Studies have shown that electroacupuncture stimulation of CV23 activated the swallowing-related neurons of (VLM) in the ventrolateral medulla of rats, and promoted swallowing activity in rats, 5-hydroxytryptamine (5-HT1A) in the nucleus of the solitary tract (NTS) may play an essential role in this excitatory effect (32,33).
Overall, this meta-analysis demonstrates the efficacy of acupuncture in treating dysphagia caused by pseudobulbar paralysis after stroke, although more high-quality RCTs are needed. In terms of treatment, we have also found that acupuncture combined with rehabilitation has a better effect, which may have some implications for clinical practice.
Limitations
This study has several limitations. Firstly, we paid attention to the efficacy of acupuncture in the treatment of dysphagia caused by pseudobulbar paralysis, but there was no comparison and research on true bulbar paralysis. Then, due to the small number of studies included, the design of RCTs was not strict, which may have an impact on the accuracy of the results. Besides, all studies were conducted in China, and it was impossible to evaluate the efficacy of acupuncture in different regions and different ethnic groups.
Conclusions
At present, there is no unified standard for the treatment of dysphagia caused by pseudobulbar paralysis after stroke. This meta-analysis fully confirmed that acupuncture could effectively improve dysphagia caused by pseudobulbar paralysis after stroke, and acupuncture combined with rehabilitation has a better effect. However, because the included studies’ quality was not high enough, the findings should be interpreted with caution. Also, further high-quality RCTs are needed.
Acknowledgments
The authors thank anyone who contributed to the article.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3551/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3551/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martino R, Foley N, Bhogal S, et al. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke 2005;36:2756-63. [Crossref] [PubMed]
- Hong C. Thirty-six cases of pseudobulbar palsy treated by needling with prompt and deep insertion. J Tradit Chin Med 2006;26:184-5. [PubMed]
- McCormick WE, Lee JH. Pseudobulbar palsy caused by a large petroclival meningioma: report of two cases. Skull Base 2002;12:67-71. [Crossref] [PubMed]
- Lo WL, Leu HB, Yang MC, et al. Dysphagia and risk of aspiration pneumonia: A nonrandomized, pair-matched cohort study. J Dent Sci 2019;14:241-7. [Crossref] [PubMed]
- Chen D, Guo H. Therapeutic effects of acupuncture combined with rehabilitation training on dysphagia in post-stroke pseudobulbar palsy. Zhongguo Zhen Jiu 2018;38:364-8. [PubMed]
- Liu YM. Observation on the effect of sublingual acupuncture combined with rehabilitation training on 42 cases of dysphagia after stroke. Suzhou University Journal of Medical Science 2009;29:1256-7.
- Liu B, Zhao JD. Clinical Study on Post-stroke Pseudobulbar Palsy Treated by Needling Nine Points on Neck and Under Tongue. Journal of Sichuan of Traditional Chinese Medicine 2014;32:143-5.
- Wang YH, Yang GF, Zhou HX, et al. Therapeutic Study of Dysphagia Caused by Pseudobular Paralysis Post-stoke Treated with Acupuncture at Aqiangzu Points. Liaoning Journal of Traditional Chinese Medicine 2017;44:2398-400.
- Chu J, Liu X, Chen F, et al. Effects of GAO's neck acupuncture on swallowing function and quality of life in patients with post-stroke pseudobulbar palsy: a randomized controlled trial. Zhongguo Zhen Jiu 2017;37:691-5. [PubMed]
- Cao LP, Gao M. Effects of Tongue-pharynx Three-Step Acupuncture Combined with Rehabilitation Training on Plasma Endothelin-1 and Nitric Oxide Levels in Patients with Cerebral Infarction Pseudo-Ball Paralysis. Journal of Traditional Chinese Medicine 2019;60:1129-33.
- Liu X, Chen F, Chu J, et al. Therapeutic observation of Gao’s nape acupuncture plus swallowing training for pharyngeal deglutition disorder after stroke. Journal of Acupuncture and Tuina Science 2019;17:37-43. [Crossref]
- Yuan Y, Qian XL, Yan WM, et al. Fire needling on dysphagia due to pseudobulbar palsy after stroke: a randomized controlled trial. Zhongguo Zhen Jiu 2020;40:347-51. [PubMed]
- Erman AB, Kejner AE, Hogikyan ND, et al. Disorders of cranial nerves IX and X. Semin Neurol 2009;29:85-92. [Crossref] [PubMed]
- Ahmed A, Simmons Z. Pseudobulbar affect: prevalence and management. Ther Clin Risk Manag 2013;9:483-9. [PubMed]
- Alonso A, Logroscino G, Jick SS, et al. Incidence and lifetime risk of motor neuron disease in the United Kingdom: a population-based study. Eur J Neurol 2009;16:745-51. [Crossref] [PubMed]
- Kim JK, Kim BJ, Shin HY, et al. Acute bulbar palsy as a variant of Guillain-Barré syndrome. Neurology 2016;86:742-7. [Crossref] [PubMed]
- Bogousslavsky J, Caplan LR. editors. Stroke Syndromes. Cambridge: Cambridge University Press, 2001.
- Zhang S, Li N, Liu M. Use of acupuncture for stroke in China. Acupunct Med 2009;27:146. [Crossref] [PubMed]
- Ye Q, Xie Y, Shi J, et al. Systematic Review on Acupuncture for Treatment of Dysphagia after Stroke. Evid Based Complement Alternat Med 2017;2017:6421852. [Crossref] [PubMed]
- Feng S, Cao S, Du S, et al. Acuuncture combined with swallowing training for post-stroke dysphagia: a randomized controlled trial. Zhongguo Zhen Jiu 2016;36:347-50. [PubMed]
- Li LX, Deng K, Qu Y. Acupuncture Treatment for Post-Stroke Dysphagia: An Update Meta-Analysis of Randomized Controlled Trials. Chin J Integr Med 2018;24:686-95. [Crossref] [PubMed]
- Zhong L, Wang J, Li F, et al. The Effectiveness of Acupuncture for Dysphagia after Stroke: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med 2021;2021:8837625. [Crossref] [PubMed]
- Huang J, Shi Y, Qin X, et al. Clinical Effects and Safety of Electroacupuncture for the Treatment of Poststroke Dysphagia: A Comprehensive Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med 2020;2020:1560978. [Crossref] [PubMed]
- Rabinstein AA, Shulman LM. Acupuncture in clinical neurology. Neurologist 2003;9:137-48. [Crossref] [PubMed]
- Jin HP, Li XL, Ye QJ, et al. Effect of electrical stimulation with bilateral scalp acupuncture on time parameters in video fluoroscopic swallowing study and cortical excitability in patients with dysphagia after cortical stroke. Zhen Ci Yan Jiu 2020;45:473-9. [PubMed]
- Shi L, Cao HM, Li Y, et al. Electroacupuncture improves neurovascular unit reconstruction by promoting collateral circulation and angiogenesis. Neural Regen Res 2017;12:2000-6. [Crossref] [PubMed]
- Xing Y, Zhang M, Li WB, et al. Mechanisms Involved in the Neuroprotection of Electroacupuncture Therapy for Ischemic Stroke. Front Neurosci 2018;12:929. [Crossref] [PubMed]
- Li X, Wang Q. Acupuncture therapy for stroke patients. Int Rev Neurobiol 2013;111:159-79. [Crossref] [PubMed]
- Liu Y, Zou LP, Du JB, et al. Electro-acupuncture protects against hypoxic-ischemic brain-damaged immature rat via hydrogen sulfide as a possible mediator. Neurosci Lett 2010;485:74-8. [Crossref] [PubMed]
- Du Y, Shi L, Li J, et al. Angiogenesis and improved cerebral blood flow in the ischemic boundary area were detected after electroacupuncture treatment to rats with ischemic stroke. Neurol Res 2011;33:101-7. [Crossref] [PubMed]
- Tao J, Xue XH, Chen LD, et al. Electroacupuncture improves neurological deficits and enhances proliferation and differentiation of endogenous nerve stem cells in rats with focal cerebral ischemia. Neurol Res 2010;32:198-204. [Crossref] [PubMed]
- Ye Q, Liu C, Shi J, et al. Effect of electro-acupuncture on regulating the swallowing by activating the interneuron in ventrolateral medulla (VLM). Brain Res Bull 2019;144:132-9. [Crossref] [PubMed]
- You H, Hu S, Ye QP, et al. Role of 5-HT1A in the nucleus of the solitary tract in the regulation of swallowing activities evoked by electroacupuncture in anesthetized rats. Neurosci Lett 2018;687:308-12. [Crossref] [PubMed]