
The efficacy and safety of combined traditional Chinese and western medicine in the treatment of chronic obstructive pulmonary disease complicated with respiratory failure: a systematic review and meta-analysis study
Introduction
Chronic obstructive pulmonary disease (COPD) is featured with progressive airflow restriction that is not completely reversible, and it is more frequent in people aged over 40. It can have adverse effects on extra-pulmonary tissues and organs. Acute exacerbation caused by COPD (AECOPD) commonly leads to type II respiratory failure (RF), which is associated with a very high mortality rate (1-3). Treatments for COPD include infection control, airway relief, correcting water, electrolyte, and acid-base imbalances. In addition, it is important to actively improve oxygenation and combat RF. The ideal living environment for patients with COPD tends to be high altitude. Long-term oxygen therapy, inhaled corticosteroids, and bronchial pipette can effectively relieve the symptoms of patients with COPD. These treatments reduce hypoxemia and airway obstruction to some extent and significantly benefit the patient’s subsequent treatment (4-6). However, respiratory muscle fatigue, poor nighttime respiratory center response, and carbon dioxide retention may contribute to further disease progression for patients with RF.
However, traditional treatment alone is not sufficient. Ko et al. [2016] (7) pointed out that excessive oxygen delivery may lead to increased carbon dioxide retention, which may worsen the disease, seriously affect lung function and quality of life, and even endanger patients’ lives. Sudden deterioration is a common reason for emergency department visits and hospitalizations in patients with COPD. In the United States, from 1993 to 2005, acute exacerbation of chronic obstructive pulmonary disease (AECOPD) resulted in an average of 600,000 emergency department visits per year (8). Research has shown that current health treatment for AECOPD includes smoking cessation, inhaled bronchodilators, systemic corticosteroids, intravenous aminophylline, antibiotics, controlled oxygen supply, and mechanical ventilation when necessary (9). Treatment for AECOPD is progressive based on the severity of the clinical presentation. Outside of China, traditional Chinese medicine (TCM) is a complementary medicine, which is alternative and unique theoretical in disease treatment. TCM regards COPD as a syndrome of dyspnea and cough (10,11). Traditional Chinese medicine believes that COPD combined with respiratory failure belongs to the deficiency of the essence and the yin-deficiency, mainly due to deficiency of vital energy (12). Therefore, modern medical methods combined with TCM dialectical treatment methods can be used in clinical practice to improve the clinical symptoms of patients. To improve the survival rate of patients with COPD + RF, clinical application of TCM dialectical treatment, combined with conventional western medicine (WM) treatment (such as chemical drugs), can significantly improve the patient’s pulmonary ventilation function and ensure the patient's smooth breathing (13,14). Phlegm-heat blocking the lung is the main etiology and pathogenesis of COPD complicated with RF (15). Therefore, clearing heat and removing blood stasis, dispersing the lung and dredging collaterals are the main points of TCM treatment of the disease. The heat-clearing and phlegm-resolving formula is often used in the treatment of COPD complicated with RF diseases (16). This work aimed to evaluate the efficacy and safety of combined TCM and WM (pure chemical) and conventional WM alone in the treatment of AECOPD by collecting randomized controlled clinical trials (RCTs) of heat-clearing and phlegm-resolving formula or injection.
At present, a large number of studies at home and abroad have confirmed that traditional Chinese medicine combined with western medicine can achieve excellent results in the treatment of COPD complicated with RF disease (17,18). The research scope of the existing meta-analysis is too broad, and there are many TCM treatment methods, and there is no unified method at present. However, whether the traditional Chinese medicine “clearing heat and resolving phlegm” category combined with western medicine can achieve excellent results in the treatment of this disease has not yet been systematically evaluated. In order to increase the systematic analysis of TCM in treating COPD complicated with RF and reduce the economic burden of COPD patients, this study retrieved many clinical RCTs of integrated TCM and WM in treating COPD complicated with RF, and carried out meta-analysis, with the aim of gathering reliable evidence to verify its efficacy and safety. We have provided a reference for the future clinical treatment of COPD combined with RF in the integrative medicine. We present the following article in accordance with the PRISMA reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-272/rc).
Methods
Literature retrieval
Databases including PubMed, Web of Science, Embase, The Cochrane Library and Wanfang data were searched by computer, and the search time range was set from the first month in 2000 to the ninth month in 2020. The key words for search were set as “Chinese medicine”, “Western medicine”, “chronic obstructive pulmonary disease”, and “respiratory failure”. A random combination of keywords was used to search the literature.
How to include and exclude the articles
The articles were included and excluded according to the participants, interventions, comparisons, outcomes (PICOS) principle. Patients in the treatment group were treated with TCM combined with chemotherapy, and those in the control group were treated with chemotherapy alone.
Articles meeting below criteria could be included: (I) Chinese and international articles about the efficacy of combined TCM and WM in treating COPD complicated with RF. (II) Direct or indirect evaluation of the indicators of curative effect of combined TCM and WM in treating COPD complicated with RF. (III) At least 15 samples were included in the study.
Articles had to be excluded if they met any of following items: (I) articles with repeated data. (II) Articles which were review, conference report, empirical lecture, case report, and commentary. (III) Research which was not related to the specific topic. (IV) Control group was not set, or the samples were different greatly so that they were comparable. (V) Studies with unclear or incomplete outcome indicators.
How to assess the literature quality
It was requested of 2 researchers that they read the full texts and extract relevant materials in the literature. Disagreements were addressed through mutual discussion or arbitration by a third party. The Cochrane Reviewer’s Handbook 4.2.5 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark) was used for literature quality assessment.
The evaluation included whether the article contained: (I) generation of random sequences. Describe in sufficient detail the method used to generate assignment sequences and assess whether the generated groupings are comparable. (II) Allocate hidden. Describe in sufficient detail the method to conceal the assignment sequence and decide whether the intervention assignment is visible during the included studies. (III) Double-blind of implementers and participants. For each primary outcome, assessments were made whether relevant information on blinding was provided. (IV) Blinding of outcome assessment. Whether outcome recipients were blinded to avoid all measures of their receiving intervention information. (V) Incomplete outcome data. Mainly describe the completeness of outcome data, including natural deletion and exclusion. Whether the literature reports missing data and reason. (VI) Select Report. Review the possibility of selectively reporting outcomes, and review the results. (VII) Other offsets. Description of other important biases.
Data to be extracted
(I) The first author, publication year, and evaluation results needed to be extracted. (II) The evaluation results included the number of participants, experimental design, specific measures, research time, and outcome indicators. (III) Baseline data of patients. (IV) Indicators of feedback research quality.
Statistical analysis
Data were analyzed statistically using Review Manager 5.3 (RevMan 5.3; The Nordic Cochrane Center, Denmark, 2014). Peto was selected to analyze the literature heterogeneity. When I2<50%, no heterogeneity was indicated, and the meta-analysis was done by using fixed effects model (FEM). When I2>50%, the heterogeneity was obvious, and random effects model (REM) was selected. The measurement data were analyzed by using weighted mean difference (WMD), or otherwise the standard deviation (SD) was adopted. The counting data were indicated by relative risk (RR) and 95% confidence intervals (CI). The funnel plots were made to assess the publication bias. In addition, the reliability and stability of the outcomes were analyzed. When P<0.05, the difference was considered to be statistically significant.
Results
Retrieval results and overview analysis
618 records were obtained initially, and 226 abstracts related to the topic specified in this work were obtained after deletion of duplicates. Two researchers read the abstract and title of the articles, 26 articles meeting the requirements were obtained through preliminary screening. After further reading the full text of the literature, non-random, repeatable, and unavailable literatures were excluded, and 7 articles (Figure 1) meeting the requirements (Table 1) were obtained and included in this study (19-25).
Table 1
| First author | Year | Outcome index | Combined medicine treatment | Control |
|---|---|---|---|---|
| Huang J (19) | 2015 | Treatment efficiency PO2, PCO2 | 50 | 50 |
| Zhang Y (20) | 2004 | Treatment efficiency | 30 | 30 |
| He B (21) | 2014 | Treatment efficiency PO2, PCO2, FEV1% | 50 | 50 |
| Li W (22) | 2008 | Treatment efficiency | 28 | 26 |
| Xie YH (23) | 2005 | Treatment efficiency, PO2, PCO2 | 52 | 30 |
| Jiu HF (24) | 2008 | Treatment efficiency, PO2, PCO2, FEV1% | 30 | 30 |
| Chen H (25) | 2016 | PO2, PCO2, FEV1% | 64 | 64 |
PO2, partial pressure of oxygen; PCO2, partial pressure of carbon dioxide; FEV, forced expiratory volume.
Bias risk
The bias risk was assessed using Cochrane Systematic Review Manual (Figures 2,3). Random sequence generation, incomplete outcome data, and selective reporting did not exist in all the 7 studies. The bias risk was thus relatively low.
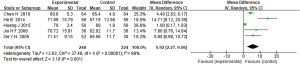
Meta-analysis on efficacy of combined TCM and WM in treating COPD + RF
Among the included articles, 6 articles carried out a detailed evaluation of the therapeutic efficiency of combined TCM and WM in treating COPD complicated with RF, and compared the therapeutic efficiency between combined TCM and WM and the traditional WM in patients with COPD. The results are shown in Figure 4. The heterogeneity was not obvious in the treatment effective rate between the combined Chinese and WM treatment group and the control group (I2=0%, P=0.85). The FEM analysis results showed that the effective rate of the 2 groups was mean difference (MD) (95% CI): 5.40 (3.14 to 9.29), and Z=6.09 (P<0.00001). The results revealed greatly different effective rate of COPD combined with RF between the 2 groups.

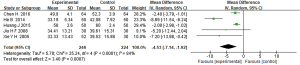
Meta-analysis of PO2 after combined treatment TCM and WM of COPD + RF
Among the included literature, 5 articles carried out a detailed evaluation of the oxygen partial pressure (PO2) after combined treatment TCM and WM of COPD with RF, and compared the post-treatment PO2 between the combined treatment of TCM and WM group and the control group using traditional WM of patients with COPD. The results are shown in Figure 5. PO2 after treatment showed observable heterogeneity between different groups (I2=89%, P<0.00001), so the analysis was realized using. The analysis structure of PO2 after treatment of 2 groups was MD (95% CI): 5.92 (2.27 to 9.56), and the statistical analysis suggested Z=3.18, P=0.001. Great difference could be found in PO2 between the 2 groups after treatment for COPD complicated with RF.
Meta-analysis on post-treatment PCO2 in combined TCM and WM for COPD + RF
Among the included literature, there were 5 documents that performed detailed evaluation of combination therapy of TCM and WM for COPD + RF after partial pressure of carbon dioxide (PCO2), and compared the PCO2 after treatment of the TCM and WM combination therapy and conventional WM alone in patients with COPD, and the results are shown in Figure 5. There was significant heterogeneity in PCO2 after therapy in 2 groups of patients (I2=84%, P<0.0001). The REM analysis revealed that analysis structure of PCO2 in the 2 groups was MD (95% CI): −4.53 (−7.14 to −1.92), and the statistical analysis suggested Z=3.40, P=0.0007. A substantial difference was found in PCO2 between the 2 groups after treatment for COPD complicated with RF (Figure 6).
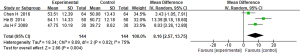
Meta-analysis of lung function after combined treatment of TCM and WM in COPD patients with RF
In included the literature, there were 3 studies which evaluated lung function after TCM and WM combination treatment for COPD with RF in detail, the other studies had a simple description, but did not describe the patient’s lung function index and specific data after treatment in detail. We compared the lung function index after combination treatment of TCM and WM and conventional WM alone for COPD with RF patients, and the results are shown in Figure 7. The lung function index data of patients was heterogeneous (I2=75%, P=0.02), which was analyzed by using REM. The MD (95% CI): 8.16 (2.57 to 13.75) was the analysis structure of lung function index data of patients in 2 groups, and the statistical test structure was Z=2.86 (P=0.004). The results showed that the lung function index data of patients in 2 groups differed greatly.
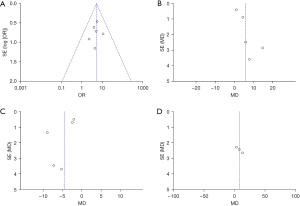
Publication bias analysis
The publication bias of treatment efficiency, PO2, PCO2, and pulmonary function [forced expiratory volume in 1 second (FEV1)%] was analyzed, and the results are shown in Figure 8. The funnel plots of treatment efficiency, recurrence rate, adverse reaction rate, and pneumonia severity index (PSI) score were basically symmetrical, so the data were relatively concentrated. This indicates that the 4 functional indicators included in this study did not have large publication bias.
Discussion
Pathologic features of COPD include inflammation, protease-antiprotease imbalance, and oxidative stress (26,27). No reliable evidence is found to prove that current drug therapies can reverse the slow decline in lung function during development of COPD. Relevant studies have shown that TCM has obvious advantages in treating COPD (28,29).
Phlegm heat injection is a Chinese medicine preparation, widely used in the treatment of fever, acute bronchitis, and acute pneumonia. The main ingredients include baikal skullcap root, honeysuckle, forsythia, bear fruit kernel, and antelope horn, and a pharmacological study showed that phlegm heat injection has antibacterial and antiviral effects. Phenolic acids, flavonoids, and lignans are active components of honeysuckle, baikal skullcap root, and forsythia. Massive amounts of inflammatory cells, cytokines, adhesion molecules, and chemokines are involved in the development and progression of COPD. Serum soluble Intercellular Adhesion Molecule-1 (sICAM-1) and interleukin-18 (IL-18) levels are higher in AECOPD and stable COPD groups than in controls (30), and they are positively correlated in AECOPD patients. They in AECOPD patients with RF were increased to non-RF patients, suggesting that the above two indicators reflect the severity of COPD. Interleukin 10 (IL-10) reduces serum sICAM-1 and IL-18 levels and inhibits COPD associated inflammation (31,32). Systematic analysis in this study found that phlegm heat injection improved lung function, PO2, and PCO2, indicating that phlegm heat injection has anti-inflammatory effects. Phlegm heat injection can effectively relieve the signs and symptoms of COPD and RF patients.
However, baicalin in phlegm-heat injections may cause adverse reactions. As research reports by scholars have confirmed that Tanre Injection treatment can cause nausea, mild headache, and chest tightness in patients, but all symptoms disappear after treatment (33). This study had some limitations. Patients were treated for 7–14 days, no long-term effects were observed, and the results of some of these indicators were highly heterogeneous. Although a REM was used, clinical heterogeneity may still have existed. The sample sizes of the studies included in this study were small, ranging from 30 to 64, which may have led to exaggerated or weakened results. It is necessary to expand the sample size in the future.
Conclusions
Seven suitable articles were selected, involving 490 patients. The RevMan 5.3 was used for data analysis. According to the meta-analysis results, the analysis structure of effective rate was MD (95% CI): 5.40 (3.14 to 9.29) and statistical analysis was Z=6.09 (P<0.00001). The analysis structure of PO2 after treatment was MD (95% CI): 5.92 (2.27 to 9.56), and the statistical analysis was Z=3.18, P=0.001. The analysis structure of PCO2 after treatment was MD (95% CI): −4.53 (−7.14 to −1.92), and the statistical analysis suggested Z=3.40, P=0.0007. The analysis structure of lung function index data was MD (95% CI): 8.16 (2.57 to 13.75), and the statistical analysis indicated Z=2.86 (P=0.004).
In conclusion, the results of this work indicated that TCM combined with WM in treating COPD + RF is more effective than WM alone, and there are no obvious serious adverse reactions. However, due to the effective conditions, there were still few evaluation indexes analyzed, and more indexes should be further analyzed on this basis. This report provides a further theoretical basis for the follow-up study on the curative effect of combined TCM and WM in treating COPD + RF.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-272/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-272/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet 2017;389:1931-40. [Crossref] [PubMed]
- Labaki WW, Rosenberg SR. Chronic Obstructive Pulmonary Disease. Ann Intern Med 2020;173:ITC17-32. [Crossref] [PubMed]
- Hattab Y, Alhassan S, Balaan M, et al. Chronic Obstructive Pulmonary Disease. Crit Care Nurs Q 2016;39:124-30. [Crossref] [PubMed]
- Gentry S, Gentry B. Chronic Obstructive Pulmonary Disease: Diagnosis and Management. Am Fam Physician 2017;95:433-41. [PubMed]
- Long R, Stracy C, Oliver MC. Nutritional care in Chronic Obstructive Pulmonary Disease. Br J Community Nurs 2018;23:S18-26. [Crossref] [PubMed]
- Yeh GY, Horwitz R. Integrative Medicine for Respiratory Conditions: Asthma and Chronic Obstructive Pulmonary Disease. Med Clin North Am 2017;101:925-41. [Crossref] [PubMed]
- Ko FW, Chan KP, Hui DS, et al. Acute exacerbation of COPD. Respirology 2016;21:1152-65. [Crossref] [PubMed]
- Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet 2015;385:899-909. [Crossref] [PubMed]
- Vogelmeier CF, Román-Rodríguez M, Singh D, et al. Goals of COPD treatment: Focus on symptoms and exacerbations. Respir Med 2020;166:105938. [Crossref] [PubMed]
- Wu CW, Lan CC, Hsieh PC, et al. Role of peripheral eosinophilia in acute exacerbation of chronic obstructive pulmonary disease. World J Clin Cases 2020;8:2727-37. [Crossref] [PubMed]
- Zheng W, Gao T, Huang H, et al. Thirteen kinds of Chinese medicine injections for acute exacerbation of chronic obstructive pulmonary disease: Protocol for a systematic review and network meta-analysis. Medicine (Baltimore) 2019;98:e16200. [Crossref] [PubMed]
- Zhang F, Sun L, Zhai J, et al. The Effect of Tanreqing Injection on the Pharmacokinetics of Sirolimus in Rats. Biomed Res Int 2019;2019:1854323. [Crossref] [PubMed]
- Wang L, Fan Y, Xu J, et al. The efficacy and safety of Tanreqing injection combined with western medicine for severe pneumonia: A protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e22010. [Crossref] [PubMed]
- Liu H, Ding XF, Guo R, et al. Effects and safety of tanreqing injection on viral pneumonia: A protocol for systematic review and meta-analysis. Medicine (Baltimore) 2020;99:e21808. [Crossref] [PubMed]
- Li W, Mao B, Wang G, et al. Effect of Tanreqing Injection on treatment of acute exacerbation of chronic obstructive pulmonary disease with Chinese medicine syndrome of retention of phlegm and heat in Fei. Chin J Integr Med 2010;16:131-7. [Crossref] [PubMed]
- Yang J, Yang J. Clearing heat and resolving phlegm for acute exacerbation of chronic obstructive pulmonary disease with the syndrome of phlegm-heat obstruction of the lung. J Int Med Res 2020;48:300060520945502. [Crossref] [PubMed]
- Xi C, Li F, Cheng W, et al. Application of traditional Chinese and Western medicine combined with chronic disease management in pulmonary rehabilitation and evaluation of efficacy. Am J Transl Res 2021;13:6372-81. [PubMed]
- Xiong C, Li Y, Zeng Y, et al. Chinese Herbal Medicine Versus Placebo for the Treatment of Chronic Obstructive Pulmonary Disease: A Protocol of Systematic Review and Meta-analysis. Medicine (Baltimore) 2019;98:e17002. [Crossref] [PubMed]
- Huang J, De Prtment P, Hospital H C, et al. The study on the application effect and safety of Tanreqing injection in treating Ptients with chronic obstructive pulmonary disease and respiratory failure. Journal of Qiqihar University of Medicine 2015;36:2830-2.
- Zhang Y, Qian LT, Wang G, et al. Randomized Controlled Trial of TanReqing Injection in Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease (Syndrome of Retention of Phlegm-Heat in the Lung). Chinese Journal of Evidence-Based Medicine 2004;5:300-7.
- He B. Clinical Study of Tanreqing Injection on Acute Exacerbation of Chronic Obstructive Pulmonary Disease. China Journal of Chinese Medicine 2014;2:189-92.
- Li W, Mao B, Wang G, et al. A study of the mechanism of Qingre Huatan therapy in treatment of acute exacerbation of chronic obstructive pulmonary disease by improving airway inflammation and mucus hypersecretion. Zhong Xi Yi Jie He Xue Bao 2008;6:799-805. [Crossref] [PubMed]
- Xie YH, Jin FG, Liu TG, et al. Curative effect of Tanreqing injection on acute exacerbation of chronic obstructive pulmonary disease. J Emerg TCM 2005;4:291-2.
- Jiu HF, Yang X. Study on effect of Tanreqing injection for Ptients with chronic obstructive pulmonary disease and acute respiratory failure. J Emerg TCM 2008;4:445-7.
- Chen H, Deng Z X, Wen Y M, et al. Therapeutic effect of tanreqing in the treatment of acute exacerbations of chronic obstructive pulmonary disease: a clinical observation. J Emerg TCM 2016;25:300-2.
- McNicholas WT, Hansson D, Schiza S, et al. Sleep in chronic respiratory disease: COPD and hypoventilation disorders. Eur Respir Rev 2019;28:190064. [Crossref] [PubMed]
- Rao W, Wang S, Duleba M, et al. Regenerative Metaplastic Clones in COPD Lung Drive Inflammation and Fibrosis. Cell 2020;181:848-864.e18. [Crossref] [PubMed]
- Zhen G, Jing J, Fengsen L. Traditional Chinese medicine classic herbal formula Xiaoqinglong decoction for acute exacerbation of chronic obstructive pulmonary disease: A systematic review protocol. Medicine (Baltimore) 2018;97:e13761. [Crossref] [PubMed]
- Yang Y, Jin X, Jiao X, et al. Advances in Pharmacological Actions and Mechanisms of Flavonoids from Traditional Chinese Medicine in Treating Chronic Obstructive Pulmonary Disease. Evid Based Complement Alternat Med 2020;2020:8871105. [Crossref] [PubMed]
- Li M, Hua Q, Shao Y, et al. Circular RNA circBbs9 promotes PM2.5-induced lung inflammation in mice via NLRP3 inflammasome activation. Environ Int 2020;143:105976. [Crossref] [PubMed]
- Ghosh N, Choudhury P, Kaushik SR, et al. Metabolomic fingerprinting and systemic inflammatory profiling of asthma COPD overlap (ACO). Respir Res 2020;21:126. [Crossref] [PubMed]
- Attia EF, Bhatraju PK, Triplette M, et al. Endothelial Activation, Innate Immune Activation, and Inflammation Are Associated With Postbronchodilator Airflow Limitation and Obstruction Among Adolescents Living With HIV. J Acquir Immune Defic Syndr 2020;83:267-77. [Crossref] [PubMed]
- Li XX, Zhuo L, Yang YH, et al. Post-marketing surveillance of Tanreqing injection in children: a real world study. Zhonghua Liu Xing Bing Xue Za Zhi 2017;38:248-52. [PubMed]





