
Risk factors for postoperative delirium in ICU patients with severe illness based on systematic review and meta-analysis
Introduction
The intensive care unit (ICU) provides isolation and equipment for patients with severe illness or coma to undergo simultaneous treatment, nursing, and rehabilitation (1,2). Severe trauma, major surgery, continuous and intensive monitoring of vital indicators, and life support require ICU treatment, with patients transferred back to the general ward when their condition improves (3,4).
Delirium, also known as acute cerebral syndrome, refers to a clinical syndrome with a variety of causes (5). Delirium is characterized by cognitive dysfunction, lack of attention, urgent onset, obvious emotional fluctuations, and mostly occurs in the elderly (6,7). There is an obvious circadian rhythm to disturbance of consciousness, which worsens at night when there is less light. Disorientation includes confusion concerning time and place, and in severe cases, disorientation of people (8,9). Perceptual disorders include hypersensitivity, delusions, and hallucinations (10). Once the delirium has passed and the patient has improved, the presentation of delirium or what occurred is mostly forgotten. Laboratory tests include whole blood routine, blood glucose, liver function, renal function, blood ammonia, blood gas analysis, urine analysis, and drug screening in urine (11). The diagnosis can be made based on typical clinical symptoms, including consciousness disorder, disorientation, and thinking disorder with fluctuating cognitive impairment (12). The etiology of delirium, such as physical disease, electrolyte disorder, alcohol or other substance dependence, can also be determined based on patient history, physical examination, and laboratory examination (13,14). The nursing measure of delirium syndrome is to actively cooperate with doctors for treatment. When patients show symptoms, we should pay attention to protect patients’ personal safety and avoid patients from injury or impulsive behavior. In daily life, patients should be protected from emotional stimulation to avoid self-injury and personal injury (15). In addition, measures such as directional guidance, treatment of cognitive impairment, reduction of psychotropic drug use, increased activity, promotion of sleep, maintenance of the balance of nutrition and water and electricity, and provision of visual and auditory assistance should be taken to control the risk factors of delirium.
The risk factors for delirium generally belong to susceptible factors, such as senile dementia, poor physical condition, cancer and cerebrovascular disease. Depression, audio-visual disorders, malnutrition, water and electrolyte imbalance, drug dependence and alcohol dependence (16). Brain function is impaired in the presence of one or more predisposing factors. At this time, the brain internal environment of the brain is affected, and acute changes resulting in neurotransmitter, neuroendocrine and neuroimmune damage in the brain all become triggering factors, and sometimes environmental changes can promote delirium (17).
At present, delirium has been studied in China and abroad. Most articles agree that age or severe disease is closely related to delirium. However, a small number of articles hold the opposite opinion, including all aspects of risk factors. All of them are controversial. Most of the articles included the research with small sample size and single patient, so most of the articles had certain limitations and the results between the articles were inconsistent, which was a normal phenomenon. At present, there is no study on the fundamental etiology of delirium in China and abroad. In this study, the meta-analysis was used to comprehensively analyze the concentration points of risk factors of delirium in critical patients based on the literature factors related to delirium in critical patients published since the establishment of the database, so as to provide a theoretical basis for further guiding the clinical treatment of postoperative delirium in critical patients in ICU.
We present the following article in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3954/rc).
Methods
Literature search strategy
A computer-based search of the China National Knowledge Network (CNKI) database, China Biomedical Literature Database, Wanfang Database, VIP Database, Baidu Academic, Chinese Medical Citation Index (CMCI), Medline, Embase, PubMed, and other databases was undertaken. Literature analyzing risk factors for postoperative delirium in critically ill ICU patients published between the database establishment date and May 30, 2021 was retrieved using the Boolean logic retrieval method of compound logic. The Chinese databases were searched using a combination of “meta-analysis”, “risk factors for delirium”, and “ICU patients with severe illness”. “Meta analysis” “Risk factors of delirium”, and “ICU severe patients” were used as search terms in the English databases. The quality of the literature was evaluated using RevMan 5.3 software for Cochrane reviews.
Multiple retrievals were carried out to determine the final included references. Search engines were used to trace the identified references, and experts and researchers in the field were contacted to access the latest research progress.
Inclusion and exclusion criteria for articles
The inclusion criteria were: (I) randomized controlled studies; (II) subjects were postoperative ICU patients with severe illness, aged at least 18 years, and hospitalization time was at least 1 day; (III) index comparison was reliable at 95% confidence interval (CI); (IV) outcome indicators were risk factors for delirium; and (V) 1 or more delirium assessment tools were used to determine the diagnosis of postoperative delirium.
The exclusion criteria were: (I) other ICU patients, not postoperative, and younger than 18 years of age; (II) repeated publications and studies with incomplete original data that could not be obtained even after contacting the authors; (III) conference materials, literature reviews, single case study reports, lectures, and critical literature; (IV) studies with research data that could not be extracted and applied; and (V) patients with a history of delirium or patients with incomplete clinical data.
The title, abstract and full text were screened by 2 industry experts, and 3 more preliminary assessments were needed before inclusion. If the opinions of the 2 experts differed, a discussion was held to reach a consistent conclusion.
Observation index
The studies included in the meta-analysis involved three types of risk factors: (I) personal factors, including age, sex, and alcohol consumption; (II) acute Physiology and Chronic Health Evaluation (Apache)-II score; and (III) treatment factors, including mechanical ventilation, the duration of mechanical ventilation, and the use of sedative drugs.
Data extraction
Data extracted were: (I) first author; (II) year of publication; (III) sample size; (IV) research design type; (V) general data of subjects (diagnostic criteria, gender, age, and diagnosis time); and (VI) evaluation indicators (risk factors).
Bias risk and quality assessment
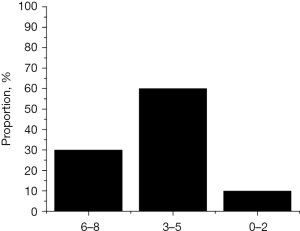
Two professional researchers evaluated the risk of bias at the same time. If their opinions differed, agreement was determined through communication and discussion. We used the recommendations of the National Institute of Clinical Excellence (NICE) for quality evaluation. Quality was evaluated on a scale of 0–8, with scores of 6–8 indicating high-quality research, 3–6 medium-quality research, and 0–2 low-quality research. Two researchers were assigned to separately evaluate the quality of the literature as “high risk bias”, “low risk bias” or “unclear”. In case of disagreement, a unified evaluation was obtained through discussion or a third party was consulted to obtain a consistent evaluation.
Statistical analysis
Statistical analysis was carried out using Stata SE14.0 software, and the effect quantities were combined. Odds ratio (OR) was used as the effect quantity index, and standardized mean difference (MD) was used as the effect index of continuous variables. Heterogeneity was tested, and results of P≥0.1 and I2≤50% indicated that there was some homogeneity among multiple studies, and thus a fixed effect model was used for meta-analysis. When the heterogeneity test results were P<0.1 and I2>50%, it indicated that heterogeneity of the studies was significant and a random effects model was used for meta-analysis, allowing the comprehensive influence of the research results causing heterogeneity to be excluded from the calculation so that the reliability of the results was more guaranteed. We used the bias risk assessment chart in RevMan 5.3 software to evaluate the risk bias of the studies. Every index effect needed to be expressed by a 95% CI.
Results
Literature search results
A total of 234 literatures were retrieved from Chinese database and 312 literatures were retrieved from English database, totaling 546 literatures. A total of 290 literatures were excluded as duplicates, leaving 256 literatures. After browsing of titles and abstracts, 189 literatures were excluded, leaving 67 literatures. After reading of the whole article, 57 literatures were removed, and 10 literatures were finally included into the meta-analysis. The flow chart of literature retrieval is shown in Figure 1. The main reasons for the exclusion of literatures were as follows: the types of literatures were duplicated [290], the types of literatures were not randomized controlled analysis [189], the subjects were not post-ICU patients [30], and the patients with lack or partial lack of relevant research information could not be obtained [27]. Figure 2 shows the quality evaluation results of the recommendations of the National Institute of Clinical Excellence. As for the quality evaluation of references, there were 3 references with scores of 6–8, accounting for 30%, 6 references with scores of 3–5, accounting for 60%, and 1 reference with scores of 0–2, accounting for 10%.
Ten literatures met the final inclusion criteria, and a total of 6,720 patients were counted in the literatures, including 1,047 delirium patients and 5,673 non-delirium patients. After reading of the 10 articles, most of these were small sample studies, the sample size of all articles ranged from 25 to 4,450, and all subjects were over 18 years old. Sample size, assessment time, and risk factor outcome indicators were described in detail in 10 articles. Table 1 shows the basic characteristics of the included literature. The experimental group was patients with delirium and the control group was patients without delirium.
Table 1
| First author | Year | Group | Sample size | Diagnosis of time | Diagnostic criteria | Outcome indicators |
|---|---|---|---|---|---|---|
| Wolters (7) | 2014 | Experimental | 412 | 12 h | CAM-ICU | 12 |
| Control | 689 | |||||
| Kamdar (8) | 2015 | Experimental | 123 | 12 h | CAM-ICU | 125 |
| Control | 100 | |||||
| Liu (9) | 2017 | Experimental | 35 | – | – | 12,467 |
| Control | 35 | |||||
| Li (10) | 2017 | Experimental | 102 | 12 h | CAM-ICU | 123 |
| Control | 234 | |||||
| Zaal (11) | 2015 | Experimental | 13 | – | CAM-ICU | 1,257 |
| Control | 12 | |||||
| Yang (12) | 2017 | Experimental | 52 | 4 h | CAM-ICU | 236 |
| Control | 89 | |||||
| Limpawattana (13) | 2016 | Experimental | 44 | 24 h | CAM-ICU | 1,234 |
| Control | 55 | |||||
| Mori (14) | 2016 | Experimental | 69 | 12 h | CAM-ICU | 5 |
| Control | 80 | |||||
| Yanaguchi (15) | 2014 | Experimental | 35 | 8 h | ICDSC | 124 |
| Control | 91 | |||||
| Pipanmekaporn (16) | 2015 | Experimental | 162 | – | ICDSC | 256 |
| Control | 4,288 |
The outcome indicators were risk factors, and there were three kinds of them. The first kind of risk factor was self-caused, which were age [1], gender [2], and alcohol consumption [3]. The second kind of risk factor was the influence of disease, that was, the score of APACHE-II [4]. The third kind of risk factor was therapeutic effect [5] mechanical ventilation, duration of mechanical ventilation [6], and sedative drug effect [7]. CAM-ICU, Pediatric Confusion Assessment Method for the ICU; ICDSC, Intensive Care Delirium Screening Checklist.
Bias risk assessment of included articles
Figures 3,4 show the evaluation results generated by RevMan 5.3 software of the multiple risk biases of the 10 included studies.
Meta-analysis of age factors
Among the 10 studies, 7 articles were related to age factors. In Figure 5, there were 764 cases in the experimental group and 1,216 cases in the control group, a total of 1,980 cases. Heterogeneity was significant, histological analysis (P<0.0001, I2=81%), and the random-effects model was therefore used, with statistically significant differences between the two groups. Meta-analysis showed that the MD value was 5.65, 95% CI: 2.29–9.01, indicating that the age of postoperative delirium in ICU patients was generally higher than that in non-delirium patients. Figure 6 shows publication bias. After analysis of the risk factor of age in 7 studies, MD value was set as horizontal plane and standard error was set as vertical plane to draw funnel plot of age risk factors. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of gender factors
Nine of the 10 studies were related to gender factors. In Figure 7, there were 978 cases in the experimental group and 5,593 cases in the control group, a total of 6,571 cases. Heterogeneity was significant with histological analysis (P=0.01, I2=59%), so the difference between the two groups was not statistically significant using a random-effect model. Meta-analysis showed that the OR value was 1.01 (95% CI: 0.73, 1.40), indicating that the incidence of postoperative delirium in ICU patients was higher in males than in females. Figure 8 shows publication bias. After the risk factor of gender in 9 studies was analyzed, the OR value was set as the horizontal plane and the standard error was set as the vertical plane to draw the funnel plot of gender risk factors. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of alcohol consumption factors
Three of the ten studies were related to alcohol consumption. In Figure 9, there were 198 cases in the experimental group and 378 cases in the control group, totaling 576 cases. Histological analysis suggested that (P=0.83, I2=0%). Therefore, using the fixed effect model, the difference between the two groups was not statistically significant. Meta-analysis showed that the OR value was 0.02 (95% CI: −0.04 to 0.08), indicating that the incidence of postoperative delirium in ICU patients who drank alcohol was higher than those who did not, but the difference was not significant. Figure 10 shows publication bias. In the three studies, after the risk factor of alcohol consumption was analyzed, the OR value was set as the horizontal plane and the standard error was set as the vertical plane to draw the funnel plot of risk factors of alcohol consumption. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of Apache-II score
Among the 10 studies, 3 articles were related to APACHE-II scoring factor. In Figure 11, there were 241 cases in the experimental group and 4,378 cases in the control group, a total of 4,619 cases. There was some homogeneity between the data, histological analysis (P=0.16, I2=46%), so the fixed effect model was used, and the difference between the two groups was statistically significant. Meta-analysis showed that the MD value was 4.84, 95% CI: 4.54–5.15, indicating that the incidence of postoperative delirium in ICU patients was positively correlated with APACHE-II score. Figure 12 shows publication bias. After analysis of APACHE-II scoring risk factors in the three studies, MD value was set as the horizontal plane and standard error was set as the vertical plane, and funnel plot of APACHE-II scoring risk factors was drawn. The lateral distribution was asymmetrical. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of mechanical ventilation
Among the 10 studies, 4 articles were related to mechanical ventilation factors. In Figure 13, there were 366 cases in the experimental group and 4,480 cases in the control group, totaling 4,846 cases. The heterogeneity was significant and histological analysis was performed (P=0.04, I2=65%), so the random-effect model was used, and the difference between the two groups was statistically significant. Meta-analysis showed that the OR value was 6.02 (95% CI: 3.24, 11.16), indicating that the incidence of postoperative delirium in ICU patients was significantly higher than that in patients without mechanical ventilation. Figure 14 shows publication bias. In the four studies, after the risk factor of mechanical ventilation was analyzed, the OR value was set as the horizontal plane and the standard error was set as the vertical plane to draw the funnel plot of mechanical ventilation risk factors. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of mechanical ventilation duration
Among the 10 studies, there were 3 literatures related to mechanical ventilation time factor. In Figure 15, there were 249 cases in the experimental group and 4,412 cases in the control group, a total of 4,661 cases. The difference in heterogeneity was significant, and histological analysis was performed (P<0.00001, I2=95%), and the difference between the two groups was not statistically significant using a random-effect model. Meta-analysis showed that the MD value was 57.52, 95% CI: −39.92 to 154.97, indicating that postoperative delirium incidence in ICU patients was positively correlated with the duration of mechanical ventilation. Figure 16 shows publication bias. In the three studies, after the risk factor of mechanical ventilation time was analyzed, MD value was set in the horizontal plane and standard error was set in the vertical plane to draw funnel plots of mechanical ventilation time risk factors. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature.
Meta-analysis of sedative use
Three of the ten studies were related to this factor in the use of sedatives. In Figure 17, there were 209 cases in the experimental group and 4,335 cases in the control group, 4,544 cases in total. The difference in heterogeneity was significant, and histological analysis was performed (P<0.00001, I2=93%). Therefore, the random-effect model was used, and the difference between the two groups was statistically significant. Meta-analysis showed that the OR value was 1.88 (95% CI: 0.23–15.50), indicating that postoperative delirium incidence in ICU patients was significantly higher than that in patients without sedatives. Figure 18 shows publication bias. In the three studies, after the risk factor analysis of sedative drug use, the OR value was set as the horizontal plane and the standard error was set as the vertical plane to plot the funnel plot of risk factors of sedative drug use. It’s asymmetrical on both sides. The experimental results indicate that there may be publication bias in the included literature
Discussion
ICU in China began in the early 1980s, and intensive care units are now mandatory in secondary and above hospitals in China (18). Postoperative delirium of ICU patients is also an increasingly frequent problem in recent years, and the treatment of delirium mainly includes (I) etiological treatment: direct treatment of etiology (19), which is difficult to define or solve; (II) support treatment: maintain electrolyte balance and supplement nutrition, with light in daytime and dark light at night; (III) symptomatic treatment: psychotropic drug treatment, which aims to avoid deepening consciousness disorders, with small dose of short-term treatment. In terms of prognosis, it should be noted that many patients will recover in a short term, can’t fully recall the disease, and complications cause functional impairment, with a mortality rate of 22–76% (20). Prevention before the onset is equally important as treatment after the onset. Therefore, 10 literatures were screened and included to conduct a meta-analysis on the risk factors causing the onset. As for the quality evaluation results of the literatures, there are 3 literatures with 6–8 scores, accounting for 30%, 6 literatures with 3–5 scores, accounting for 60%, and 1 literature with 0–2 scores, accounting for 10%, indicating that the included literatures were credible.
Among the 10 studies, there were 7 literatures related to age. The MD value of meta-analysis was 5.65 (95% CI: 2.29–9.01), indicating that the age of postoperative delirium in ICU patients was generally higher than that in non-delirium patients. Meta-analysis showed that the OR value was 1.01 (95% CI: 0.73–1.40), indicating that the incidence of postoperative delirium in ICU patients was higher in males than in females. Meta-analysis showed that the OR value was 0.02 (95% CI: −0.04 to 0.08), indicating that the incidence of postoperative delirium in ICU patients who drank alcohol was higher than those who did not, but the difference was not significant. Meta-analysis showed that the MD value was 4.84 (95% CI: 4.54–5.15), indicating that the incidence of postoperative delirium in ICU patients was positively correlated with APACHE-II score. Meta-analysis showed that the OR value was 6.02 (95% CI: 3.24–11.16), indicating that the incidence of postoperative delirium in ICU patients was significantly higher than that in patients without mechanical ventilation. Meta-analysis showed that the MD value was 57.52 (95% CI: −39.92 to 154.97), indicating that postoperative delirium incidence in ICU patients was positively correlated with the duration of mechanical ventilation. There were 3 literatures related to the use of mechanical sedatives. Meta-analysis showed an OR value of 1.88 (95% CI: 0.23–15.50), indicating that postoperative delirium incidence in ICU patients with severe symptoms was significantly higher than that in patients without sedatives. Ten studies were included, studies on different risk factors were analyzed, and funnel plots were made for each risk factor. The results showed that there was asymmetry and possibly publication bias. The experimental results were generally stable, and the conclusions obtained were relatively credible. The quality level of the included experiments in the meta-analysis of this study was medium to high.
Conclusions
In this study, 10 literatures were included adopting the composite logic Boolean search method, and the risk factors for postoperative delirium in ICU patients were evaluated by meta-analysis. Because the factors causing delirium are various, the main points, including the gender and age of their own factors and whether they drink alcohol, were analyzed. APACHE-II score was found to affect the disease. The effects of treatment include mechanical ventilation, the duration of mechanical ventilation, and sedative drugs. Therefore, this study may have certain limitations, and the results may be contingent and different. In conclusion, different risk factors can influence the incidence of delirium in clinical practice, and corresponding treatment plans can be implemented for ICU patients with severe conditions to reduce the incidence of delirium.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3954/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3954/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wan L, Xue FS, Hou HJ. Assessing risk factors of delirium and its effects on adverse outcomes in patients admitted to the ICU after craniotomy. Eur J Anaesthesiol 2021;38:191-2. [Crossref] [PubMed]
- Tsujii T, Uchida T, Hirano J, et al. Risk factors of delirium following electroconvulsive therapy: a systematic review. European Neuropsychopharmacology 2017;27:S857. [Crossref]
- Kamiya M, Aoyama T, Kano K, et al. Risk factors for postoperative delirium after gastrointestinal surgery - using randomized Phase II trial data. Annals of Cancer Research and Therapy 2018;26:95-100. [Crossref]
- Thompson C, Brienza VJM, Sandre A, et al. Risk factors associated with acute in-hospital delirium for patients diagnosed with a hip fracture in the emergency department. CJEM 2018;20:911-9. [Crossref] [PubMed]
- Hernandez BA, Lindroth H, Rowley P, et al. Post-anaesthesia care unit delirium: incidence, risk factors and associated adverse outcomes. Br J Anaesth 2017;119:288-90. [Crossref] [PubMed]
- van Montfort SJT, Slooter AJC, Kant IMJ, et al. fMRI network correlates of predisposing risk factors for delirium: A cross-sectional study. Neuroimage Clin 2020;27:102347. [Crossref] [PubMed]
- Wolters AE, van Dijk D, Pasma W, et al. Long-term outcome of delirium during intensive care unit stay in survivors of critical illness: a prospective cohort study. Crit Care 2014;18:R125. [Crossref] [PubMed]
- Kamdar BB, Niessen T, Colantuoni E, et al. Delirium transitions in the medical ICU: exploring the role of sleep quality and other factors. Crit Care Med 2015;43:135-41. [Crossref] [PubMed]
- Liu D, Lyu J, Zhao H, et al. The influence of analgesic-based sedation protocols on delirium and outcomes in critically ill patients: A randomized controlled trial. PLoS One 2017;12:e0184310. [Crossref] [PubMed]
- Li G, Lei X, Ai C, et al. Low plasma leptin level at admission predicts delirium in critically ill patients: A prospective cohort study. Peptides 2017;93:27-32. [Crossref] [PubMed]
- Zaal IJ, van der Kooi AW, van Schelven LJ, et al. Heart rate variability in intensive care unit patients with delirium. J Neuropsychiatry Clin Neurosci 2015;27:e112-e116. [Crossref] [PubMed]
- Yang J, Zhou Y, Kang Y, et al. Risk Factors of Delirium in Sequential Sedation Patients in Intensive Care Units. Biomed Res Int 2017;2017:3539872. [Crossref] [PubMed]
- Limpawattana P, Panitchote A, Tangvoraphonkchai K, et al. Delirium in critical care: a study of incidence, prevalence, and associated factors in the tertiary care hospital of older Thai adults. Aging Ment Health 2016;20:74-80. [Crossref] [PubMed]
- Mori S, Takeda JR, Carrara FS, et al. Incidence and factors related to delirium in an intensive care unit. Rev Esc Enferm USP 2016;50:587-93. [Crossref] [PubMed]
- Yamaguchi T, Trukioka E, Kishi Y. Outcomes after deliriu in a Japanese intesive care unit. General Hospital Psychiatry 2014;36:634-6. [Crossref] [PubMed]
- Pipanmekaporn T, Chittawatanarat K, Chaiwat O, et al. Incidence and risk factors of delirium in multi-center Thai surgical intensive care units: a prospective cohort study. J Intensive Care 2015;3:53. [Crossref] [PubMed]
- Xue FS, Wan L, Zhang L. Assessing risk factors of post-liver transplant delirium and its effect on postoperative outcome. Eur J Gastroenterol Hepatol 2021;33:448. [Crossref] [PubMed]
- Simons KS, Workum JD, Slooter AJ, et al. Effect of preadmission sunlight exposure on intensive care unit-acquired delirium: a multicenter study. J Crit Care 2014;29:283-6. [Crossref] [PubMed]
- Krewulak KD, Stelfox HT, Ely EW, et al. Risk factors and outcomes among delirium subtypes in adult ICUs: A systematic review. J Crit Care 2020;56:257-64. [Crossref] [PubMed]
- Yamamoto T, Mizobata Y, Kawazoe Y, et al. Incidence, risk factors, and outcomes for sepsis-associated delirium in patients with mechanical ventilation: A sub-analysis of a multicenter randomized controlled trial. J Crit Care 2020;56:140-4. [Crossref] [PubMed]
(English Language Editor: A. Muijlwijk)



















