
Analysis of risk factors for 90-day mortality after surgery in elderly patients with intertrochanteric fractures and a history of cardiovascular disease
Introduction
Hip fracture is a common type of fracture in the elderly, particularly elderly women. It is estimated that the absolute number of hip fractures in the world will reach 4.5 million by 2050 (1), with intertrochanteric fractures accounting for 44.1% of them (2). Among the different types of fracture, intertrochanteric fractures in elderly patients have the highest probability of internal fixation surgery. With the aging of our country’s population, the incidence of intertrochanteric fracture in elderly patients is increasing every year (3,4), which is seriously affecting the quality of life for the elderly in their later years.
The postoperative complication and mortality rates in elderly patients with intertrochanteric fractures are much higher than other fracture internal fixation operations. It has been reported that the mortality rate after fracture is as high as 16.3% (5), which poses a huge challenge to existing medical treatment. Common death-related risk factors such as age, gender, malnutrition, activities of daily living (ADL) scores, and comorbidities before injury affect the mortality rate after fracture (6-8). In addition, some laboratory test indicators have also been proposed as important risk factors for post-fracture death (9,10). Among them, patients with a history of cardiovascular disease (CVD) are at greater risk of postoperative death (6,8,11). Cardiovascular emergencies such as myocardial infarction, pulmonary embolism, or cerebral infarction in patients with intertrochanteric fractures during the perioperative period are common serious complications and direct causes of death (11,12).
At present, research on risk factors related to death in elderly patients with intertrochanteric fractures in the presence of previous CVD is not sufficient, and the clinical evaluation model of related risk factors has not been confirmed (6,8). Therefore, this study established a 90-day postoperative all-cause mortality risk prediction model for elderly patients with intertrochanteric fractures and previous CVD based on clinical data and explored the clinical application value of related risk factors in predicting the postoperative mortality risk of patients.
We present the following article in accordance with the STARD reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3625/rc).
Methods
Data
This study reviewed a total of 166 elderly patients with intertrochanteric fractures and previous CVD admitted between January 1, 2010 and December 31, 2014. The study included 42 males (25.3%) and 124 females (74.7%), and the average age was 82.9±11.7 years old. All patients had a history of cardiovascular disease and were treated with proximal femoral nail antirotation (PFNA) internal fixation. Of the 166 patients involved in the study, 16 (9.6%) died within 90 days after follow-up. Analysis of the related risk factors for death within 90 days after surgery was conducted. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Ethics Committee of Sichuan Provincial People’s Hospital [ethical approval number: Lun Shen (Research) No. 25 of 2020] and informed consent was taken from all the patients.
Definition of previous history of cardiovascular disease
Patients with intertrochanteric fractures and a history of heart failure (ICD-10: I50), ischemic heart disease (ICD-10: I20-25), or ischemia stroke (ICD-10: I63-64) diagnosed within 5 years before the fracture were included in the study. Preoperative examination revealed calcified plaques in the coronary artery, aorta, or internal carotid artery.
Case inclusion criteria
The inclusion criteria were as follows: elderly patients (aged ≥70 years), intertrochanteric fractures, previous history of cardiovascular disease, clear indications for surgery, no contraindications to PFNA surgery, signed informed consent, and surgical treatment.
Case exclusion criteria
The exclusion criteria included: severe metabolic bone disease, malignant tumor, end-stage disease due to other conditions, voluntary discharge without medical advice, and patients admitted to hospital more than 24 hours after injury.
Statistical methods
Descriptive statistical analyses using standard reporting methods were employed. We used the Shapiro-Wilk normality test for measurement data: for normally distributed data, the mean ± standard deviation and Student’s t-test were used, and the median (interquartile range) and the Wilcoxon rank sum test were used for nonnormally distributed data. In addition, we used the χ2 test for count data, unless the count data had only 2 categories and there was a classification frequency ≤5 or total sample size ≤40, in which case the Fisher’s exact test was used. Kaplan-Meier survival curves were plotted and the logrank test was employed to statistically test the survival curves. Stepwise multivariate Cox risk proportional regression model was used to analyze the risk factors and report the hazard rate (HR) of the risk factors. The significance level was set to α=0.05, and all statistical analyses were completed in R-3.5.1 software.
Results
Baseline analysis
We used the 90-day follow-up baseline data of elderly patients with intertrochanteric fractures and a history of cardiovascular disease to establish a 90-day survival group and a 90-day death group according to whether mortality occurred during the follow-up period. Analysis of the risk factors of the 2 groups showed that patient age was higher in the death group than in the survival group (P=0.023). The American Society of Anesthesiologists (ASA) classification of the 2 groups of patients was different (P=0.003). In addition, the concentration of N-terminal pro brain natriuretic peptide (NT-proBNP) in the patients who had died was significantly higher than that in the surviving patients (P<0.001), while concentration of high-density lipoprotein (HDL) was significantly lower than that of surviving patients (P=0.011, Table 1).
Table 1
| Variable | 90-day survival group (n=150) | 90-day death group (n=16) | Statistic | P value |
|---|---|---|---|---|
| Gender, n (%) | 0.40a | 0.526 | ||
| Male | 39 (26.0) | 3 (18.8) | ||
| Female | 111 (74.0) | 13 (81.3) | ||
| Age, years | 82.5±12.1 | 86.9±6.1 | 2.40b | 0.023 |
| Body mass index (kg/m2) | 23.0 (20.0–26.0) | 21.5 (20.5–25.0) | 1335c | 0.461 |
| ASA class, n (%) | 8.36a | 0.003 | ||
| I–II | 95 (63.3) | 5 (31.2) | ||
| III–IV | 45 (36.7) | 11 (68.8) | ||
| Duration of hospitalization, days | 12.0 (9.0–15.0) | 16.0 (9.0–34.0) | 1006.5c | 0.294 |
| NT-proBNP (pmol/L) | 134.7 (88.5–230.0) | 636.0 (211.7–706.8) | 441.5c | <0.001 |
| Total cholesterol (mmol/L) | 4.26±1.43 | 3.95±0.92 | 1.18b | 0.253 |
| Triglycerides (mmol/L) | 0.94±0.55 | 0.89±0.25 | 0.56b | 0.582 |
| High-density lipoprotein (mmol/L) | 1.61±0.70 | 1.23±0.68 | 2.71b | 0.011 |
| Low-density lipoprotein (mmol/L) | 2.35±1.27 | 2.73±0.85 | 1.62b | 0.118 |
| Hemoglobin (g/dL) | 7.73±1.41 | 7.30±2.34 | 0.73b | 0.479 |
a, the χ2 statistic; b, the Student’s t-test; c, the Wilcoxon W statistic.
Multiple regression analysis
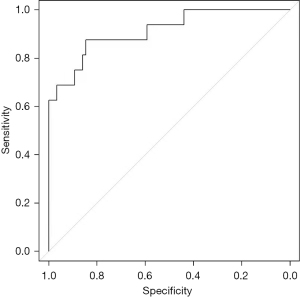
A multivariate Cox proportional regression model was used to establish a 90-day all-cause mortality risk model. The stepwise method was used to adjust the Cox model based on the Akaike information criterion (AIC), and a stable risk model was finally obtained (Table 2). The risk model showed that length of hospital stay and NT-proBNP were significant risk factors, while HDL was a protective factor. The receiver operating characteristic (ROC) curve of the Cox regression model is shown in Figure 1 and the area under the curve (AUC) =0.91.
Table 2
| Variable | HR (95% CI) | Statistics | P value |
|---|---|---|---|
| Hospital stay | 1.07 (1.04–1.11) | 4.26 | <0.001 |
| NT-proBNP | 1.01 (1.01–1.02) | 4.61 | <0.001 |
| High-density lipoprotein | 0.41 (0.18–0.96) | 2.05 | 0.042 |
| Low-density lipoprotein | 1.03 (0.99–1.74) | 2.26 | 0.060 |
HR, hazard ratio; 95% CI, 95% confidence interval.
Kaplan-Meier survival analysis
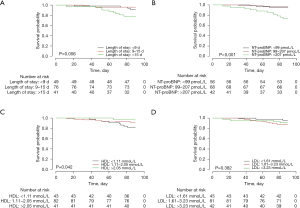
The results of Kaplan-Meier survival curve analysis for each independent risk factor were separated into quartiles and then used to divide the follow-up cohort into 3 groups. Differences among the survival curves and the 3 groups were observed. As shown in Figure 2, a significant difference was shown by the logrank test of the survival curves grouped according to hospital stay length (<9 days, 9–15 days, and >15 days; P=0.006). Significant differences were also found for the NT-proBNP groups (<99 pmol/L, 99–207 pmol/L, and >207 pmol/L; P<0.001) and the HDL groups (<1.11 mmol/L, 1.11–2.05 mmol/L, and >2.05 mmol/L; P=0.042).
Discussion
Intertrochanteric fractures of the femur, also known as femoral intertrochanteric fractures, occur below the femoral neck (from the intertrochanteric line to the beginning of the femoral medullary cavity below the lesser trochanter) (13) and often befall the elderly due to osteoporosis. The mortality for elderly patients with intertrochanteric fractures within 12 months of injury is as high as 12–37% (14).
Surgery is the mainstream treatment for intertrochanteric fracture. There are four common surgical methods, including proximal femoral intramedullary nail internal fixation, proximal femoral bone plate internal fixation, external fixation stent fixation, artificial joint replacement. Proximal femoral intramedullary nail fixation has the advantages of short operation time, small surgical trauma, small intraoperative blood loss, short force arm and well biomechanical conditions, which is beneficial to early postoperative weight-bearing and accelerate functional recovery. It is more suitable for elderly patients with intertrochanteric fracture complicated with cardiovascular disease. Proximal lateral femoral plate internal fixation is the most commonly used surgical method in the past, which has the advantages of lower surgical difficulty and fewer intraoperative radiographic projection times. However, the surgical trauma is large, and the long force arm of lateral internal fixation is only suitable for patients with Evans I and II fracture type. Elderly patients with intertrochanteric fractures are mostly osteoporotic fractures and most of them are comminted unstable fractures, so intramedullary fixation with biomechanical advantages is more suitable. External fixation stent fixation operation has little trauma, simple anesthesia, good tolerance and less blood loss. However, limited by postoperative needle infection and low fracture fixation strength, it increases the risk of postoperative implant failure, fracture non-union and fracture reduction loss, and also increases the difficulty of postoperative nursing. It is usually used for patients who cannot tolerate surgery and anesthesia and cannot accept blood transfusion. Joint replacement is rarely used for intertrochanteric fractures. Its surgical trauma and intraoperative blood loss are mainly used for previous serious hip joint diseases with joint replacement indications, or as a remedy for internal fixation failure. In conclusion, for elderly patients with intertrochanteric fractures with a history of cardiovascular disease, internal fixation with proximal femoral intramedullary nail is adopted. It has the advantages of small surgical trauma, short operation time, supporting early postoperative ambulation with weight bearing, shortening bed time, accelerating functional recovery, and effectively reducing the incidence of postoperative complications, which is conducive to improving the function of elderly patients and reducing mortality.
Previous studies have confirmed that the severity of anemia, intraoperative and postoperative blood loss, operation time, bed time after injury, and nursing status were related to increased mortality (14). This study found that patients with a hospital stay longer than 15 days had a significantly higher mortality rate within 90 days after surgery (P=0.006, Figure 2A), suggesting that the longer the hospital stay, the worse the prognosis. This may be related to complications such as venous thrombus embolism, pulmonary infection, cerebral ischemic stroke, myocardial infarction and pulmonary embolism caused by long-term bed rest during hospitalization. The longer the hospital stay, the higher the probability of these complications, which directly affect the patient’s prognosis. Roche et al. (15) found that pulmonary infection and heart failure were the most common complications leading to increased postoperative mortality. Our study found that the risk of death increased 1.07 times for every additional day of hospitalization, which was consistent with the results of a study by Pareja Sierra et al. (16): the longer the postoperative hospital stay, the greater the risk of infection and heart failure, and the higher the risk of death. It is generally believed that the main factors affecting the length of hospital stay, excluding the direct causes of fracture types, are postoperative complications and their severity (9). Therefore, the length of hospital stay directly correlates with the number and severity of postoperative complications of patients and also indicates that the number and severity of postoperative complications is an important cause of patient death.
At the same time, cardiovascular disease is very common in elderly patients with hip fractures, particularly heart failure (17,18). NT-proBNP is a quantitative marker of heart failure, with high specificity and sensitivity for diagnosis of heart failure (17). Its concentration is clinically significant in predicting the risk of postoperative heart failure in patients with femoral intertrochanteric fractures. One population-based large-data cohort study found that the 30-day postoperative mortality of patients with hip fractures increased with the concentration of NT-proBNP (19). Our multivariate Cox proportional regression model analysis found that NT-proBNP was an independent risk factor for postoperative death in patients with elderly intertrochanteric fractures and a history of cardiovascular disease (HR =1.01, P<0.05), and the risk of death doubled in patients with NT-proBNP concentration increased by 100 pmol/L. Survival analysis found that the 90-day mortality rate of patients with NT-proBNP level >207 pmol/L was significantly higher than in patients with NT-proBNP level <207 pmol/L (Figure 2B). Heart failure is one of the main factors leading to postoperative death in elderly patients with femoral intertrochanteric fractures. We believe that there is a significant correlation between trauma and concentration of NT-proBNP. NT-proBNP exceeding 207 pmol/L indicates that a patient’s reserve of heart function before injury was poor, and the risk of heart failure after surgery is higher. This suggests that for elderly patients with intertrochanteric fractures and a history of cardiovascular disease, preoperative NT-proBNP concentration exceeding 207 pmol/L could be used as an independent risk assessment threshold. When NT-proBNP is higher than this value, the risk of surgery should be carefully evaluated. Studies by Hietala et al. (20) found that preoperative heart failure is an important predictor of myocardial infarction in patients with hip fractures during the perioperative period. Further, Huddleston et al. (21) found that preoperative heart failure history was an independent predictor for postoperative myocardial infarction.
Our study found that HDL was an independent protective factor for postoperative death in elderly patients with intertrochanteric fractures and a history of cardiovascular disease (HR =0.41, P<0.05). Further, for every increase of 1 pmol/L in HDL concentration, the risk of death decreased 41%. In a study of 113,211 hip fracture patients, Norring-Agerskov et al. (18) found that the mortality rate within 30 days of fracture decreased with an increase of HDL concentration. This was because HDL, as a vascular protective lipoprotein, can significantly reduce the risk of cardiovascular and cerebrovascular diseases (22), thereby reducing the risk of thrombotic events and even death in patients after surgery. Our study found that LDL was not an independent risk factor for postoperative death in elderly patients with intertrochanteric fractures and a history of cardiovascular disease (HR =1.03, P>0.05). Survival analysis showed that the higher the HDL concentration, the lower the mortality (P<0.05, Figure 2C), while there was no difference among the LDL groups (P>0.05, Figure 2D). Cardiovascular and cerebrovascular events are an important cause of postoperative death in patients. We believe that the preoperative HDL level is an independent indicator of the degree of cardiovascular damage in patients (23,24). Therefore, assessment of risk and mortality from postoperative cardiovascular and cerebrovascular events could be based on HDL concentration. However, LDL, as the main lipoprotein in cardiovascular damage receiving clinical consideration, was not found to be an independent risk factor in our study (P>0.05). The possible reason for this is that most elderly patients receive lipid-lowering therapy, which may have caused confounding bias.
Moreover, we also analyse the one-year mortality is 13.3% with 22 patients dead. The main cause of death is pulmonary infection (8 patients), heart failure (2 patients), myocardial infarction (5 patients), stroke (5 patients,) and pulmonary embolism (2 patients), which related to lying in bed, blood loss, surgery method and anesthesia mode. The length of hospital stay increases and the NT-proBNP abnormality suggest the occurrence of acute complications.
In summary, we found that the length of hospital stay, plasma NT-proBNP concentration, and HDL concentration could be used as sensitive predictors for prognosis in elderly patients with intertrochanteric fracture surgery and a history of cardiovascular disease. To prevent and care for complications, bed time should be reduced as much as possible, sitting rest is recommended for those who cannot get out of bed, cardiopulmonary function training, control intravenous infusion volume and speed, shorten the operation fasting time, which can significantly reduce complications. However, this study had certain limitations. First, this study was a retrospective study. Second, the type, number, and severity of cardiovascular-related diseases of patients have a greater impact on outcome events, but due to the limited number of samples included in the study, it was impossible to incorporate this factor into the risk model for evaluation. In a later study, we plan to incorporate multi-center data to expand the sample size for statistical modeling analysis.
Acknowledgments
Funding: This work was supported by the Joint Project of Southwest Medical University and the Affiliated Traditional Chinese Medicine Hospital of Southwest Medical University (No. 2020XYLH-013).
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3625/rc
Data Sharing Statement: Available at https://apm.amegroups.com/article/view/10.21037/apm-21-3625/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-21-3625/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Ethics Committee of Sichuan Provincial People’s Hospital [ethical approval number: Lun Shen (Research) No. 25 of 2020] and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury 2018;49:1458-60. [Crossref] [PubMed]
- Kim JW, Kim DH, Jang EC, et al. Mortality and its risk factors in nonagenarians after hip fractures. J Orthop Sci 2019;24:850-4. [Crossref] [PubMed]
- Zhao F, Wang X, Dou Y, et al. Analysis of risk factors for perioperative mortality in elderly patients with intertrochanteric fracture. Eur J Orthop Surg Traumatol 2019;29:59-63. [Crossref] [PubMed]
- Wang X, Zhao BJ, Su Y. Can we predict postoperative complications in elderly Chinese patients with hip fractures using the surgical risk calculator? Clin Interv Aging 2017;12:1515-20. [Crossref] [PubMed]
- Mohd-Tahir NA, Li SC. Economic burden of osteoporosis-related hip fracture in Asia: a systematic review. Osteoporos Int 2017;28:2035-44. [Crossref] [PubMed]
- Wong CX, Gan SW, Lee SW, et al. Atrial fibrillation and risk of hip fracture: A population-based analysis of 113,600 individuals. Int J Cardiol 2017;243:229-32. [Crossref] [PubMed]
- Riemen AH, Hutchison JD. The multidisciplinary management of hip fractures in older patients. Orthop Trauma 2016;30:117-22. [Crossref] [PubMed]
- Bhattacharyya T, Iorio R, Healy WL. Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am 2002;84:562-72. [Crossref] [PubMed]
- Sennerby U, Farahmand B, Ahlbom A, et al. Cardiovascular diseases and future risk of hip fracture in women. Osteoporos Int 2007;18:1355-62. [Crossref] [PubMed]
- Carbone L, Buzková P, Fink HA, et al. Hip fractures and heart failure: findings from the Cardiovascular Health Study. Eur Heart J 2010;31:77-84. [Crossref] [PubMed]
- Yu CM, Chan YS, Zhang Q, et al. Benefits of cardiac resynchronization therapy for heart failure patients with narrow QRS complexes and coexisting systolic asynchrony by echocardiography. J Am Coll Cardiol 2006;48:2251-7. [Crossref] [PubMed]
- Chen DX, Yang L, Ding L, et al. Perioperative outcomes in geriatric patients undergoing hip fracture surgery with different anesthesia techniques: A systematic review and meta-analysis. Medicine (Baltimore) 2019;98:e18220. [Crossref] [PubMed]
- Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med 2017;377:2053-62. [Crossref] [PubMed]
- Chen PH, Wu CC, Chen WJ. Factors affect stability of intertrochanteric fractures when elderly patients fall. Biomed J 2016;39:67-71. [Crossref] [PubMed]
- Roche JJ, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005;331:1374. [Crossref] [PubMed]
- Pareja Sierra T, Bartolomé Martín I, Rodríguez Solís J, et al. Predictive factors of hospital stay, mortality and functional recovery after surgery for hip fracture in elderly patients. Rev Esp Cir Ortop Traumatol 2017;61:427-35. [Crossref] [PubMed]
- van Diepen S, Majumdar SR, Bakal JA, et al. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation 2008;118:1946-52. [Crossref] [PubMed]
- Norring-Agerskov D, Madsen CM, Bathum L, et al. History of cardiovascular disease and cardiovascular biomarkers are associated with 30-day mortality in patients with hip fracture. Osteoporos Int 2019;30:1767-78. [Crossref] [PubMed]
- Santaguida PL, Don-Wauchope AC, Oremus M, et al. BNP and NT-proBNP as prognostic markers in persons with acute decompensated heart failure: a systematic review. Heart Fail Rev 2014;19:453-70. [Crossref] [PubMed]
- Hietala P, Strandberg M, Strandberg N, et al. Perioperative myocardial infarctions are common and often unrecognized in patients undergoing hip fracture surgery. J Trauma Acute Care Surg 2013;74:1087-91. [Crossref] [PubMed]
- Huddleston JM, Gullerud RE, Smither F, et al. Myocardial infarction after hip fracture repair: a population-based study. J Am Geriatr Soc 2012;60:2020-6. [Crossref] [PubMed]
- Albers JJ, Slee A, Fleg JL, et al. Relationship of baseline HDL subclasses, small dense LDL and LDL triglyceride to cardiovascular events in the AIM-HIGH clinical trial. Atherosclerosis 2016;251:454-9. [Crossref] [PubMed]
- Sposito AC, de Lima-Junior JC, Moura FA, et al. Reciprocal Multifaceted Interaction Between HDL (High-Density Lipoprotein) and Myocardial Infarction. Arterioscler Thromb Vasc Biol 2019;39:1550-64. [Crossref] [PubMed]
- Boden WE. High-density lipoprotein cholesterol as an independent risk factor in cardiovascular disease: assessing the data from Framingham to the Veterans Affairs High--Density Lipoprotein Intervention Trial. Am J Cardiol 2000;86:19L-22L. [Crossref] [PubMed]
(English Language Editor: A. Muijlwijk)


