Editor’s note: “Palliative Radiotherapy Column” features articles emphasizing the critical role of radiotherapy in palliative care. Chairs to the columns are Dr. Edward L.W. Chow from Odette Cancer Centre, Sunnybrook Health Sciences Centre in Toronto and Dr. Stephen Lutz from Blanchard Valley Regional Cancer Center in Findlay, gathering a group of promising researchers in the field to make it an excellent column. The column includes original research manuscripts and timely review articles and perspectives relating to palliative radiotherapy, editorials and commentaries on recently published trials and studies.
Do patients with brain metastases selected for whole brain radiotherapy have worse baseline quality of life as compared to those for radiosurgery or neurosurgery (with or without whole brain radiotherapy)?
Background
Brain metastases patients are selected for treatment based on performance status, age, co-morbidities, whether the metastasis to brain is single or multiple, neurosurgical resectability for single brain metastasis and extracranial disease extent. The goals of brain metastases treatment are to improve brain control (local brain metastases control or whole brain control) and possibly improve survival. Other considerations include neurocognitive outcomes and quality of life (QOL). Guidelines based on these principles have been published (1,2).
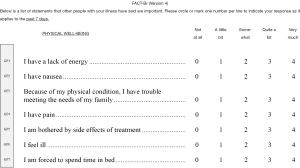
Patients with brain metastases often experience psychological, emotional, social and physical difficulties which can all affect QOL (3-5). QOL is most commonly assessed through self-administered questionnaires (6). The Functional Assessment of Cancer Therapy-Brain (FACT-Br) administered in conjunction with the FACT-G is a common questionnaire used to study QOL in brain metastases patients (4). The FACT-Br totals 50 items that covers physical, social/family, emotional, and functional well-being (FWB), as well as disease specific concerns such as concentration, memory, seizures, eyesight, personality, expression of thoughts, weakness, coordination and headaches (4,6,7) (Appendix 1). While the tool was originally used and validated for primary brain tumors, it has frequently been used in brain metastases patients (8,9). The purpose of this study was to examine the baseline QOL in patients treated with whole brain radiotherapy (WBRT) alone versus stereotactic radiosurgery (SRS) or surgery with or without WBRT, as assessed by the FACT-Br.
Methods
Newly diagnosed brain metastases patients were approached for the study at the time of their consultation. All consecutive series in patients with brain metastases in Rapid Response Radiotherapy Clinic and CNS clinic who agreed to participate were included. Patients with solitary brain metastasis and good performance status with limited extracranial disease were referred for a neurosurgical opinion. Patients with four or less brain metastases would be assessed for SRS while those with multiple metastases for WBRT. Informed consent was obtained. Patient demographic information was collected including age, gender, primary cancer site, years from primary cancer to brain metastases, Karnofsky Performance Status (KPS) score, and Eastern Cooperative Oncology Group Performance Status (ECOG PS) score. Baseline FACT-Br results were obtained prior to brain metastases treatment. Eligible patients were analysed based on their treatment: WBRT alone versus SRS or neurosurgery with or without WBRT. Additionally, the FACT-Br items were grouped according to their different domains (physical, social/family, emotional, functional, well-being and additional concerns) for summary domain scores.
Statistical analysis
To compare demographics between WBRT alone versus SRS or neurosurgery with or without WBRT patients, Wilcoxon rank-sum nonparametric test or Fisher exact test was applied for continuous or categorical variables. When analyzing the 50 FACT-Br item scores between these two groups, Fisher exact test was also conducted. Summary scores were calculated with respect to physical well-being (PWB; using individual items GP1−GP7), social/family well-being (SWB; using individual items GS1−GS7), emotional well-being (EWB; using individual items GE1−GE6), (FWB; using individual items GF1−GF7), brain cancer (BrC; using individual items Br1-An10) subscale, FACT-Br Trial Outcome Index (TOI), FACT-G (General) total score, FACT-Br (Brain) total score. The higher the scores, the better the QOL.
For items with opposite meaning compared to other items in the section, the inversed values were calculated at the first step to make sure all FACT-Br scales had the same direction. To derive the subscale scores (PWB, SWB, EWB, FWB, and BrC), we used the following method for calculation: (sum individual item scores × number of items)/number of items answered. FACT-Br TOI was defined as the sum of PWB, FWB, and BrC subscale score; FACT-G total score was defined as the sum of PWB, SWB, EWB, and FWB; and FACT-Br total score was defined as the sum of FACT-G total score and BrC subscale score (10).
In the current analysis of the FACT-Br questionnaires (version 4), BrC subscale was calculated either using 46 additional concern items (Br1−Br18) or using 50 additional concern items (Br1−An10). Furthermore, FACT-Br TOI and FACT-Br total score had also two sets of scores. All of the aforementioned scores were analyzed separately. Wilcoxon rank-sum nonparametric test was used to compare the summary scores between the two groups. Two-sided P value <0.05 was considered statistically significant. All analyses were performed using Statistical Analysis Software (SAS version 9.4 for Windows).
Results
Patient demographics
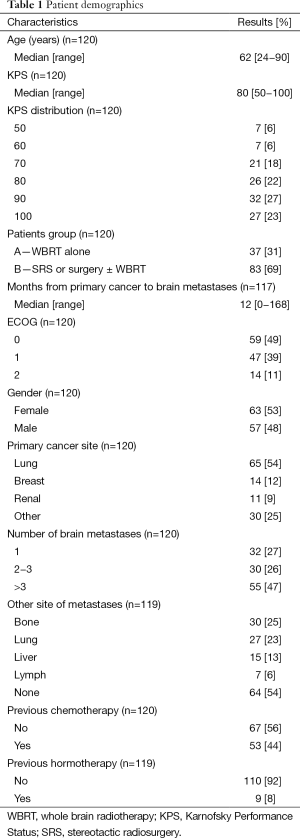
A total of 120 patients were enrolled, with 37 (31%) treated with WBRT alone and 83 (69%) with SRS or surgery with or without WBRT from June 2012 to October 2014. The median age was 62 (range, 24−90) years old and median KPS was 80 (range, 50−100). Fifty-nine (49%), forty-seven (39%) and fourteen (12%) had ECOG PS scores of 0, 1 and 2, respectively. The median time from primary cancer to brain metastases was 1 year (range, 0−14 years). There were 63 females (53%) and 57 males (48%), of which lung (n=65; 54%), breast (n=14; 12%) and renal (n=11; 9%) were the three most common primary cancer sites. With respect to the number of brain metastases, 32 patients (27%) had one, 30 (26%) had 2−3, and 55 (47%) had more than 3. Of 119 patients with available information on extracranial disease, 30 (25%) had bone metastases, 27 (23%) had lung metastases, 15 (13%) had liver metastases, 7 (6%) had lymph metastases, and 64 (54%) had no other metastases (Table 1).
Full table
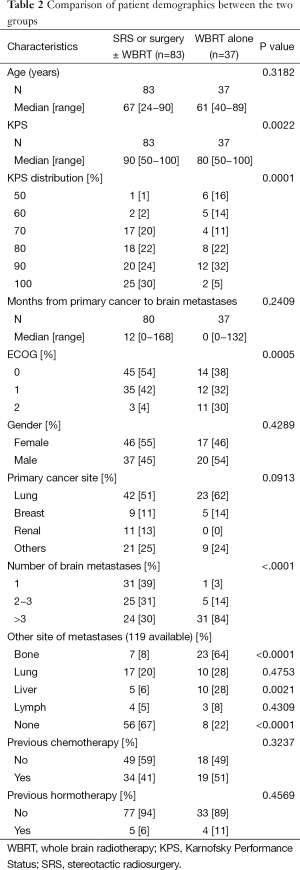
KPS scores between the two groups were significantly different (P=0.002), with WBRT alone patients generally reporting lower KPS scores; median of 80 rather than 90. There were more SRS or surgery with or without WBRT patients with KPS scores of 100 [25 patients (30%) vs. 2 patients (5%) for WBRT alone], while more of WBRT alone patients reported KPS scores of 50 [6 patients (16%) vs. 1 patient (1%)], and 60 [5 patients (14%) vs. 2 patients (2%) (P=0.0001)]. WBRT alone patients also more frequently reported poorer ECOG scores (P=0.0005), with only 11 patients (30%), as opposed to 3 (4%) patients, with a score of 2. WBRT alone patients typically had a higher number of brain metastases [>3 metastases; 31 patients (84%) vs. 24 patients (30%)], and a larger proportion had bone [23 patients (64%) vs. 7 patients (8%)] and liver [10 patients (28%) vs. 5 patients (6%)] metastases as well (Table 2).
Full table
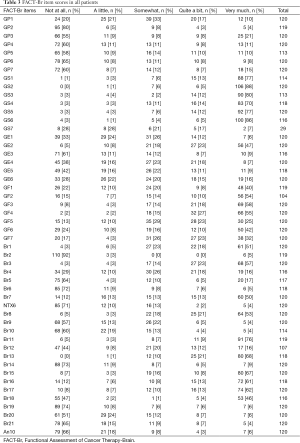
FACT-Br item scores
The frequency of each FACT-Br item score is shown in Table 3. The most common QOL concerns in the entire cohort (based on at least 80% of patients responding quite a bit or very much) were items in the PWB domain (with the exception of “I am forced to spend time in bed”). A total of 82% of patients responded with quite a bit and very much in terms of accepting their illness. A total of 85% of patients responded with quite a bit or very much with respect to making decisions and taking responsibility. Eight-nine percent of patients felt that they were able to put their thoughts together, ranked as quite a bit or very much.
Full table
FACT-Br item scores of the two groups
The item I feel ill (GP6) was notably different between patients receiving WBRT alone compared to SRS or surgery with or without WBRT (P=0.001). The two groups had similar proportions of patients who did not report illness (“not at all”; 65% for both). However, more WBRT alone patients reported “a little” illness (16% compared to 5%) and “very much” illness (16% vs. 4%), while more patients treated with SRS or surgery with or without WBRT reported “somewhat” (15% compared to 3%) and “quite a bit” (12% vs. 0%) of illness (Table 4). All other PWB scores were not significantly different between the two groups.
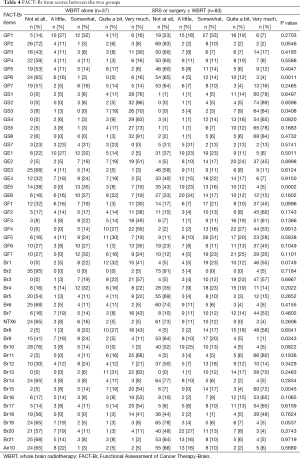
Full table
Patients of the two groups reported different levels of support from their friends (GS3) (P=0.04). SRS or surgery with or without WBRT patients reported greater levels of support (“very much”; 84% vs. 70%), while more WBRT alone patients reported a lack of support (“not at all”; 8% vs. 0%) (Table 4). None of the other SWB questions were statistically significant between the two groups.
The worry of death (GE5) differed between WBRT alone and SRS or surgery with or without WBRT (P=0.0002). Less WBRT alone patients had no worry (38% vs. 43%), or “a little” fear (0% compared to 24%) of death. Less patients of SRS or surgery with or without WBRT reported moderate (“somewhat”; 16% in comparison to 35%) and significant (“very much”; 5% vs. 19%) fear of death (Table 4). All other EWB and FWB scores were not different between the two groups.
SRS or surgery with or without WBRT patients had less difficulty expressing their thoughts (Br9). No difficulty was reported in 64% of SRS or surgery with or without WBRT, while only 41% of WBRT alone patients had no difficulty. A greater proportion of WBRT alone patients reported difficulty expressing thoughts: “somewhat” (24%>21%), “quite a bit” (5.4%>4.8%), and “very much” (11%>1%). There were more SRS or surgery with or without WBRT patients who found it very easy to put their thoughts into action (“very much”; 72% compared to 54%) (P=0.005) (Table 4).
FACT-Br summary scores of the two groups
Using the scales with 46 items, FWB, FACT-G total score, BrC subscale score, FACT-Br total score and FACT-Br TOI (when using 46 items) were found to be statistically significant between the two groups (P=0.04, 0.04, 0.02, 0.02, and 0.02, respectively). SRS or surgery with or without WBRT had higher scores, or better QOL, than WBRT alone patients with respect to FWB (19.6>16.9), FACT-G total score (82.3>76.2), BrC subscale score (60.3>55.4), FACT-Br total score (142.7>131.7), and FACT-Br TOI (100.9>91.7). The higher PWB (21.0>19.3), SWB (25.2>24.4) and EWB (16.6>15.6) scores for SRS and WBRT were numerically higher but not significant (P=0.40, 0.84, and 0.23, respectively) (Table 5).
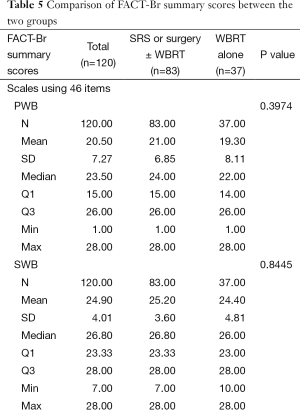
Full table
Similar findings were expressed in the scale with 50 items: WBRT alone had significantly lower QOL across all scores, however, PWB, SWB and EWB did not show the significant difference between two groups (P=0.40, 0.84, and 0.23, respectively). FWB (19.6>16.9), FACT-G total score (82.3>76.2), BrC subscale score (73.5>68.5), FACT-Br total score (155.8>144.8) and FACT-Br TOI (114.1>104.8) were all reported higher for SRS or surgery with or without WBRT patients (P=0.04, 0.04, 0.02, 0.02, and 0.02, respectively) (Table 5).
Discussion
Several studies (11-15) have investigated the choice between WBRT or SRS alone, or a combination of the two treatments. All have included good prognosis patients and up to four small brain metastases for the use of radiosurgery alone, with documented benefit in terms of neurocognitive sparing and QOL as compared to WBRT (16,17). Patients with good prognosis and resectable single brain metastasis who underwent neurosurgery had better survival as compared to patients who did not have neurosurgery but rather only WBRT (18,19).
This study evaluated baseline QOL between WBRT alone versus SRS or surgery with or without WBRT. A higher proportion of WBRT alone patients had lower KPS and ECOG PS scores. Additionally, a higher percentage of WBRT alone patients had greater than three brain metastases. Both of these findings illustrate common practices as documented in the literature. Physicians are less likely to treat patients with poor performance status and multiple brain metastases using SRS or neurosurgery (20-24). The lower QOL as observed in WBRT alone patients may be related to more brain metastases, and active extracranial disease. Li et al. documented that a correlation exists between lower neurocognitive function and an associated lower QOL (25). We also found that WBRT alone patients had worse FWB in particular.
Limitations
Our study was limited by English speaking patients. Patients who declined study or with very poor performance status as they were too ill would not be captured in this study. We only compared the baseline differences.
Conclusions
WBRT alone patients reported statistically different baseline QOL as compared to patients who went on to have SRS or neurosurgery (with or without WBRT); five of fifty individual items and five of eight summary items had lower QOL.
Acknowledgements
We thank the generous support of Bratty Family Fund, Michael and Karyn Goldstein Cancer Research Fund, Joey and Mary Furfari Cancer Research Fund, Pulenzas Cancer Research Fund, Joseph and Silvana Melara Cancer Research Fund, and Ofelia Cancer Research Fund.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Supplementary
Appendix 1 The Functional Assessment of Cancer Therapy-Brain (FACT-Br) Questionnaire
References
- Expert Panel on Radiation Oncology-Brain Metastases, Lo SS, Gore EM, et al. ACR Appropriateness Criteria® pre-irradiation evaluation and management of brain metastases. J Palliat Med 2014;17:880-6. [PubMed]
- Tsao MN, Rades D, Wirth A, et al. Radiotherapeutic and surgical management for newly diagnosed brain metastasis(es): An American Society for Radiation Oncology evidence-based guideline. Pract Radiat Oncol 2012;2:210-25. [PubMed]
- Popovic M, Nguyen J, Chen E, et al. Comparison of the EORTC QLQ-BM22 and the FACT-BP for assessment of quality of life in cancer patients with bone metastases. Expert Rev Pharmacoecon Outcomes Res 2012;12:213-9. [PubMed]
- Chow R, Lao N, Popovic M, et al. Comparison of the EORTC QLQ-BN20 and the FACT-Br quality of life questionnaires for patients with primary brain cancers: a literature review. Support Care Cancer 2014;22:2593-8. [PubMed]
- Chen E, Nguyen J, Zhang L, et al. Quality of life in patients with brain metastases using the EORTC QLQ-BN20 and QLQ-C30. J Radiat Oncol 2012;1:179-86.
- Chiu N, Chiu L, Zeng L, et al. Quality of life in patients with primary and metastatic brain tumors in the literature as assessed by the FACT-Br. World J Oncol 2012;3:280-5.
- Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol 1993;11:570-9. [PubMed]
- Thavarajah N, Bedard G, Zhang L, et al. The Functional Assessment of Cancer Therapy – Brain (FACT-Br) for assessing quality of life in patients with brain metastases: a comparison of recall periods. J Pain Manage 2013;6:223-34.
- Chen E, Cella D, Zeng L, et al. Content validation of the FACT-Br with patients and health-care professionals to assess quality of life in patients with brain metastases. J Radiat Oncol 2014;3:105-13.
- Thavarajah N, Bedard G, Zhang L, et al. Psychometric validation of the functional assessment of cancer therapy—brain (FACT-Br) for assessing quality of life in patients with brain metastases. Support Care Cancer 2014;22:1017-28. [PubMed]
- Sahgal A, Larson D, Knisely J. Stereotactic radiosurgery alone for brain metastases. Lancet Oncol 2015;16:249-50. [PubMed]
- Sahgal A, Aoyama H, Kocher M, et al. Phase 3 trials of stereotactic radiosurgery with or without whole-brain radiation therapy for 1 to 4 brain metastases: individual patient data meta-analysis. Int J Radiat Oncol Biol Phys 2015;91:710-7. [PubMed]
- Andrews DW, Scott CB, Sperduto PW, et al. Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 2004;363:1665-72. [PubMed]
- Tsao MN, Lloyd N, Wong RK, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev 2012;4:CD003869. [PubMed]
- Stafinski T, Jhangri GS, Yan E, et al. Effectiveness of stereotactic radiosurgery alone or in combination with whole brain radiotherapy compared to conventional surgery and/or whole brain radiotherapy for the treatment of one or more brain metastases: a systematic review and meta-analysis. Cancer Treat Rev 2006;32:203-13. [PubMed]
- Chang EL, Wefel JS, Hess KR, et al. Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 2009;10:1037-44. [PubMed]
- Soffietti R, Kocher M, Abacioglu UM, et al. A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life results. J Clin Oncol 2013;31:65-72. [PubMed]
- Patchell RA, Tibbs PA, Walsh JW, et al. A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 1990;322:494-500. [PubMed]
- Vecht CJ, Haaxma-Reiche H, Noordijk EM, et al. Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 1993;33:583-90. [PubMed]
- Kondziolka D, Patel A, Lunsford LD, et al. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 1999;45:427-34. [PubMed]
- Smalley SR, Laws ER Jr, O'Fallon JR, et al. Resection for solitary brain metastasis. Role of adjuvant radiation and prognostic variables in 229 patients. J Neurosurg 1992;77:531-40. [PubMed]
- Black P. Brain metastasis: current status and recommended guidelines for management. Neurosurgery 1979;5:617-31. [PubMed]
- Sundaresan N, Galicich JH, Beattie EJ Jr. Surgical treatment of brain metastases from lung cancer. J Neurosurg 1983;58:666-71. [PubMed]
- Young RF, Jacques DB, Duma C, et al. Gamma knife radiosurgery for treatment of multiple brain metastases. Radiosurgery 1996;1:92-101.
- Li J, Bentzen SM, Li J, et al. Relationship between neurocognitive function and quality of life after whole-brain radiotherapy in patients with brain metastasis. Int J Radiat Oncol Biol Phys 2008;71:64-70. [PubMed]