
Effect of self-management interventions for adults with epilepsy: a systematic review and meta-analysis
Introduction
Epilepsy is a common chronic disease of the nervous system, with about 50 million patients worldwide (1-3). Epilepsy is a syndrome of the highly synchronized abnormal discharge of brain neurons caused by a variety of factors, and its clinical manifestations are paroxysmal, transient, repetitive, and stereotyped (4,5). The unpredictability of epileptic seizures, the long-term physical discomfort caused by the disease, the concerns of patients about the side effects of antiepileptic drugs, and the social discrimination against the disease all affect the psychology and behavior of adult patients with epilepsy leading to a decline in their quality of life (6,7).
Although antiepileptic drugs (AEDs) have made progress in the treatment of patients with epilepsy, many patients with epilepsy still have negative health events (nhes), such as accidental and emergency (ER) visits and low quality of life. Therefore, self-management is very necessary (3,4). Self-management sees patients consistently improving and maintaining their health through their behavior and managing and monitoring the symptoms and symptoms of their disease to reduce its impact on their social function, emotion, and interpersonal relationships (8,9). The three tasks of self-management include daily life management, disease medical management, and emotional cognition management (10).
A self-management program specific for patients with epilepsy involves experts teaching the concept and purpose of self-management, and the significance of self-management to improve patients’ quality of life, while members of the research team work with the patient to develop a personal self-management plan appropriate for their individual needs (11-13). At the same time, patients are required to fill in their personal self-management plan on time, which is regularly checked by research team members. Nurses give patient guidance to patients with poor compliance and strengthen telephone supervision. Experts teach relevant knowledge of antiepileptic drugs so that patients realize the importance of taking them on time and in a sufficient quantity for seizure control (14-16). Patients who often miss taking medicine are reminded by setting their mobile phones or alarm bells. Patients make separate medicine boxes and arrange medication for the following day before going to bed, and place the box where it can be easily seen. Patients who have regular meals are asked to take medicine at meals, and to also take antiepileptic drugs with them when leaving the home (17,18).
While our search revealed some published meta-analyses of self-management in children with epilepsy, there remain few concerning adults. Therefore, we conducted this meta-analysis on the effect of self-management in adults with epilepsy. In this article, we compared three critical scale and included researches published between 2018 and 2020, which can further evaluate the effects of self-management for epilepsy. The evaluating scales include QOLIE-31, SWLS, and ESMS. The QOLIE-31 is a survey of health-related quality of life for adults (18 years or older) with epilepsy. The SWLS is a short 5-item instrument designed to measure global cognitive judgments of satisfaction with one's life. The Epilepsy Self-Management Scale (ESMS) is a 38-item scale that assesses frequency of use of epilepsy self-management practices (3-6). We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-2404).
Methods
Literature search strategy
A systematic search of the PubMed, EMBASE, Web of Science and China National Knowledge databases between January 2000 and February 2021 was conducted using the keywords: ‘self-management’, ‘adult’, and ‘epilepsy’.
We conducted a comprehensive search through the Internet in multiple databases, trial registries and meeting minutes, and the included literature has no restrictions on the publication language or publication status. Randomized controlled trials and non-randomized studies of interventions that enrolled adults with epilepsy who self-managed their condition and reported the following outcomes with aggregate data: QOLIE-31, SWLS, and ESMS, were considered.
Study selection
The inclusion criteria were organized according to the population, interventions, comparisons, results and setting/study design (Picos) reporting structure.
(I) Self management interventions included healthy age-matched men and women; (II) clearly gender matched training doses; and (III) QOLIE-31, SWLS and ESMS reported before and after training. The most comprehensive reports are contained in multiple publications involving the same study. The inclusion of articles is not limited by publication status or language.
If the study: (I) only includes the patient group, it is excluded; (II) there is no control group or only an alternative intervention group; (III) it does not meet the minimum requirements for the description of at least one indicator; (IV) the results are not fully reported, or the relevant authors do not respond to the query sent by e-mail. According to the inclusion and exclusion criteria defined a priori, two independent reviewers screened potentially relevant articles by analyzing the title, abstract and full text to clarify their qualifications. If the two commentators do not agree on the inclusion of an article, the third author is contacted.
After contacting the authors for more detailed information, studies published only in the form of abstracts were included. If more than one publication is available in the same queue, we extract data from the largest or most recent dataset.
Data extraction and quality assessment
Study characteristics, including first author, year of publication, study design, and baseline demographic characteristics were extracted. In addition, outcome information, including QOLIE-31, SWLS, and ESMS were abstracted.
We assessed the risk of bias in the included literature according to the Cochrane Collaboration bias risk tool, which was used to assess the risk of bias in randomized trials from five areas (selection, performance, wear, reporting and other bias).
Statistical analysis
The heterogeneity analyses in our study were performed with Review Manager 5.4 (The Cochrane Collaboration, 2020) to estimate the different effects between self-management and control groups in patients with epilepsy. Differences in three included outcomes between self-management with control subjects were expressed as MD with pertinent 95% CIs. The overall effect was tested using Z-scores, and significance was set at P<0.05. I2 was used in this study Statistics test the heterogeneity of measurement research. Specifically, I2 values less than 50% indicate low heterogeneity, and values greater than 50% indicate high heterogeneity. If heterogeneity is observed, a random effect model is used, and if there is no inter study heterogeneity, a fixed effect model is used. Potential publication bias was assessed by Begg funnel plot and egger linear regression test. P<0.05 indicates publication bias. As shown in our results, we found that most p values of Begg’s and egger’s tests were above 0.05, indicating that there was no significant publication bias except for the results listed in other documents. Finally, we performed a sensitivity analysis to assess the robustness of the results. We excluded the included literature in turn and observed the change of I2 value, so as to evaluate the stability of the results.
Results
Search process
From the electronic search, 698 articles were identified, and after careful reading, 42 studies were found to meet the preliminary criteria. We further excluded 34 articles based on study design, improper inclusion criteria, or insufficient data to abstract, leaving eight studies (19-26) meeting the inclusion criteria and included in the meta-analysis (Figure 1).
Characteristics of included studies
The detailed characteristics of the eight eligible studies are summarized in Table 1, and contained six RCTs, one prospective clinical study, and one retrospective observational study. The year of publication was between 2018 and 2020, the sample size was between 60 and 453, and the subjects included 590 males and 876 females.
Table 1
| Study | Year | Language | Country | Groups | Sex (male/female) | Age (years) | n | Years of onset |
|---|---|---|---|---|---|---|---|---|
| Brigg | 2020 | English | USA | SM | 21/39 | 41.8±14.9 | 60 | 2018 to 2019 |
| Control | 23/37 | 40.9±14.6 | 60 | |||||
| Edward | 2019 | English | UK | SM | 9/14 | 39.9±15.1 | 23 | 2015 to 2018 |
| Control | 22/15 | 40.2±12.6 | 37 | |||||
| Johnson | 2020 | English | USA | SM | 18/31 | 42.9±14.3 | 49 | 2018 to 2019 |
| Control | 23/29 | 42.8±13.7 | 52 | |||||
| Leenen | 2018 | English | Netherlands | SM | 28/24 | 39.91±3.4 | 52 | March 2014 to December 2015 |
| Control | 22/28 | 39.6±3.6 | 50 | |||||
| Ridsdale | 2018 | English | UK | SM | 90/115 | 42.5±14.3 | 205 | 2015 to 2016 |
| Control | 95/104 | 40.8±14.0 | 199 | |||||
| Sajatovic | 2018 | English | USA | SM | 21/39 | 41.5±12.3 | 60 | 2017 |
| Control | 17/42 | 41.0±11.4 | 59 | |||||
| Sajatovic | 2019 | English | USA | SM | 85/147 | 44.5±12.5 | 232 | 2019 |
| Control | 80/141 | 42.4±12.6 | 221 | |||||
| Thompson | 2019 | English | USA | SM | 17/35 | 41.9±12.4 | 52 | 2010 to 2013 |
| Control | 19/36 | 42.6±12.1 | 55 |
SM, self-management.
Results of quality assessment
The Cochrane risk of bias assessment tool was used to evaluate the risk of the included studies, and revealed seven categories with a low risk of bias in greater than 60%. Only one category, selective reporting, displayed a high risk of bias (Figure 2). To minimize the impact of several confounding factors on the difference in outcomes between self-management and control subjects, we pooled data from the eight studies in which researchers reported adjusted risk estimates, and the results showed that the included articles had good quality (Figure 3).
Results of heterogeneity test
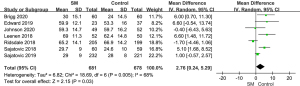
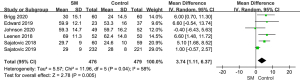
Heterogeneity analysis of QOLIE-31 between SM and control
To analyze the difference in QOLIE-31 between SM and control groups, we performed a meta-analysis to calculate the risk ratio using the random-effect model based on heterogeneity analysis. The overall mean difference was 2.76 with 95% CI (0.24, 5.29). The P value of overall effect was 0.03, I2=68%, which demonstrated that the difference of QOLIE-31 between SM and control groups had significance, and QOLIE-31 in the SM group was higher than in the control group (Figure 4).
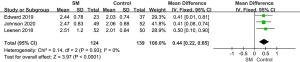
Heterogeneity analysis of SWLS between SM and control
Similarly, a meta-analysis for the difference in SWLS between SM and control groups was conducted. The result showed that there was significant difference of SWLS between the SM and control group [MD =0.44, 95% CI: (0.22, 0.65), P<0.0001, fixed effect model], and the included studies were of low homogeneity (P=0.93, I2=0%) (Figure 5).
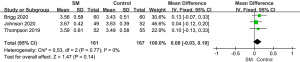
Heterogeneity analysis of ESMS between SM and control
For live birth rate, 3 studies involving 328 patients reported it. Meta-analysis showed that ESMS in SM group was higher than that in control group [MD =0.08, 95% CI: (−0.03, 0.19), P=0.14, fixed effect model], with insignificant heterogeneity (I2=0%) (Figure 6).
Results of sensitivity analysis and publication bias
A total of seven studies reported QOLIE-31. The forest plot showed that the SM group had better QOLIE-31 than the control group [MD =2.76 with 95% CI: (0.24, 5.29), while the P value of the overall effect was 0.03, I2=68%] (Figure 4). We performed a sensitivity analysis by removing Ridsdale 2018’s study, and the change in result was small, in that I2 changed from 68% to 58% (Figure 7), which indicated that the results of the included articles were robust.
We also performed a funnel plot to evaluate the publication bias for QOLIE-31, and the figure showed that the shape was symmetric. The P value of the Egger test was 0.585, which indicated no significant publication bias existed in this meta-analysis (Figure 8).
Discussion
Eight studies met the inclusion criteria to evaluate the effects of self-management for patients with epilepsy. Meta-analysis of these studies showed differences in QOLIE-31 and SWLS, which indicated that self-management could improve quality of life and SWLS in adult epilepsy patients. In addition, results of the ESMS showed that self-management had a higher ESMS scale than a control group.
Studies of self-management intervention in patients with epilepsy are usually conducted using the Quality of Life Scale for Patients with Epilepsy (QOLIE-31), Satisfaction With Life Scale (SWLS), and Epilepsy Self-Management Scale (ESMS). The Quality of Life in Epilepsy-31 (QOLIE-31) in the United States is composed of 31 items and seven aspects, including seizure worry, life satisfaction, mood, energy/fatigue status, and recognition. Knowledge function, the influence of anti-epileptic drugs, and social position. Each aspect includes 2–6 questions, with the score of each question first converted into a percentile score, and the rough score of each element is equal to the sum of the scores of each question included in it divided by the number of questions. The wild scores are then multiplied by their respective weight scores to obtain sub-items. The total scores are obtained by adding the sub-items and the higher the score, the better the patient’s quality of life. The ESMS queries drug-related, safety-related, and general lifestyle management behaviors and the higher the score, the stronger the self-management ability. The ESMS is a fully validated and commonly used self-report scale to assess how often individuals perform tasks that help control seizures. It contains 38 statements, each of which is scored with 5 points, and the answers range from “never” to “always” (27-29).
Although new types of anti-epileptic drugs continue to emerge and surgical methods continue to improve, epileptic seizures still severely impact the physical and mental health and quality of life of patients (30). With changes to ways in which both the medical profession and the community view epilepsy, the condition is now managed with seizure control medication and the hope that patients will maintain a normal work, social, and home life (31). Past studies have shown that through self-management interventions, patients can gain knowledge about epilepsy, change their attitudes towards epilepsy, increase confidence in treating the disease, establish healthy behaviors, reduce the number of seizures, prolong the interval between seizures, and reduce the side effects of anti-epileptic drugs (9,10,32). Self-management improves the self-efficacy of adult patients with epilepsy and guides them to participate in self-management actively, master self-management skills, manage everyday medication by themselves, adhere to treatment, deal with various social problems, and make full use of their social support system to improve social adaptability (33). Through psychological intervention, patients learn to regulate and control their emotions and cope with various pressures, thereby improving their mental health and quality of life (34).
In addition, self management could be improved in the future, including several aspects. We could develop new programs including (I) treatment management, such as taking medicines as prescribed, keeping medical appointments, and communicating effectively with health care providers; (II) seizure management, such as recognizing and avoiding seizure triggers and keeping track of when seizures happen; (III) lifestyle management, such as getting enough sleep and reducing stress (31-34).
Overall, compared with the control group, self-management patients showed better results in several parameters including QOLIE-31, SWLS, and ESMS. As an effective intervention for adult patients with epilepsy, self-management can help them better improve their quality of life and improve their satisfaction.
This study also has some limitations. For example, the efficacy indicators are not comprehensive enough, but other parameters are lacking; different studies have different follow-up times, affecting the final result. In summary, self-management is effective for adult patients with epilepsy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-2404
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-2404). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ 2008;336:491-5. [Crossref] [PubMed]
- Yang L, Zhang R, Zhu H, et al. Factors influencing the long-term prognosis of patients with temporal lobe epilepsy: a single center study. Ann Palliat Med 2020;9:3194-203. [Crossref] [PubMed]
- Nguyen DK, Mbacfou MT, Nguyen DB, et al. Prevalence of nonlesional focal epilepsy in an adult epilepsy clinic. Can J Neurol Sci 2013;40:198-202. [Crossref] [PubMed]
- Leppik I, Birn Ba Um AK, Harms SL, et al. 15. Epilepsy co-morbidities in nursing homes: Focus on Alzheimer's. Epilepsy Behavior 2010;17:583-4. [Crossref]
- Camfield P, Camfield C, Pohlmann-Eden B. Transition from pediatric to adult epilepsy care: a difficult process marked by medical and social crisis. Epilepsy Curr 2012;12:13-21. [Crossref] [PubMed]
- Zeng J, Pediatrics DO. The Application of Integrated Nursing Intervention in the Nursing of Pediatric Epilepsy Patients. China Continuing Medical Education, 2018.
- de Tisi J, Bell GS, Peacock JL, et al. The long-term outcome of adult epilepsy surgery, patterns of seizure remission, and relapse: a cohort study. Lancet 2011;378:1388-95. [Crossref] [PubMed]
- Kinnunen UM, Kivekäs E, Paananen P, et al. Testing of Triggers by Data Mining of Epilepsy Patients' Structured Nursing Records. Stud Health Technol Inform 2015;225:461-5. [PubMed]
- Buelow J, Miller W, Fishman J. Development of an Epilepsy Nursing Communication Tool: Improving the Quality of Interactions Between Nurses and Patients With Seizures. J Neurosci Nurs 2018;50:74-80. [Crossref] [PubMed]
- Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care 2001;24:561-87. [Crossref] [PubMed]
- Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159-71. [Crossref] [PubMed]
- Bodenheimer T, Lorig K, Holman H, et al. Patient self-management of chronic disease in primary care. JAMA 2002;288:2469-75. [Crossref] [PubMed]
- Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Med Care 2001;39:1217-23. [Crossref] [PubMed]
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet 2004;364:1523-37. [Crossref] [PubMed]
- Warsi A, Wang PS, LaValley MP, et al. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med 2004;164:1641-9. [Crossref] [PubMed]
- Manni R, Terzaghi M, Arbasino C, et al. Obstructive sleep apnea in a clinical series of adult epilepsy patients: frequency and features of the comorbidity. Epilepsia 2003;44:836-40. [Crossref] [PubMed]
- Holman HR, Lorig K. Self-management education for osteoarthritis. Ann Intern Med 2006;144:617-author reply 617-8. [Crossref] [PubMed]
- Devos-Comby L, Cronan T, Roesch SC. Do exercise and self-management interventions benefit patients with osteoarthritis of the knee? A metaanalytic review. J Rheumatol 2006;33:744-56. [PubMed]
- Johnson EK, Fraser RT, Lashley S, et al. Program of Active Consumer Engagement in Self-Management in Epilepsy: Replication and extension of a self-management randomized controlled trial. Epilepsia 2020;61:1129-41. [Crossref] [PubMed]
- Briggs FBS, Wilson BK, Pyatka N, et al. Effects of a remotely delivered group-format epilepsy self-management program on adverse health outcomes in vulnerable people with epilepsy: A causal mediation analysis. Epilepsy Res 2020;162:106303. [Crossref] [PubMed]
- Thompson NJ, McGee RE, Garcia-Williams A, et al. The impact of a depression self-management intervention on seizure activity. Epilepsy Behav 2020;103:106504. [Crossref] [PubMed]
- Edward KL, Cook M, Stephenson J, et al. The impact of brief lifestyle self-management education for the control of seizures. Br J Nurs 2019;28:348-54. [Crossref] [PubMed]
- Sajatovic M, Johnson EK, Fraser RT, et al. Self-management for adults with epilepsy: Aggregate Managing Epilepsy Well Network findings on depressive symptoms. Epilepsia 2019;60:1921-31. [Crossref] [PubMed]
- Ridsdale L, Wojewodka G, Robinson EJ, et al. The effectiveness of a group self-management education course for adults with poorly controlled epilepsy, SMILE (UK): A randomized controlled trial. Epilepsia 2018;59:1048-61. [Crossref] [PubMed]
- Sajatovic M, Colon-Zimmermann K, Kahriman M, et al. A 6-month prospective randomized controlled trial of remotely delivered group format epilepsy self-management versus waitlist control for high-risk people with epilepsy. Epilepsia 2018;59:1684-95. [Crossref] [PubMed]
- Leenen LAM, Wijnen BFM, Kessels AGH, et al. Effectiveness of a multicomponent self-management intervention for adults with epilepsy (ZMILE study): A randomized controlled trial. Epilepsy Behav 2018;80:259-65. [Crossref] [PubMed]
- Mattsson P, Tomson T, Eriksson O, et al. Sociodemographic differences in antiepileptic drug prescriptions to adult epilepsy patients. Neurology 2010;74:295-301. [Crossref] [PubMed]
- Adachi N, Kanemoto K, Muramatsu R, et al. Intellectual prognosis of status epilepticus in adult epilepsy patients: analysis with Wechsler Adult Intelligence Scale-revised. Epilepsia 2005;46:1502-9. [Crossref] [PubMed]
- Lorig K, Seleznick M, Lubeck D, et al. The beneficial outcomes of the arthritis self-management course are not adequately explained by behavior change. Arthritis Rheum 1989;32:91-5. [Crossref] [PubMed]
- Lorig KR, Mazonson PD, Holman HR. Evidence suggesting that health education for self-management in patients with chronic arthritis has sustained health benefits while reducing health care costs. Arthritis Rheum 1993;36:439-46. [Crossref] [PubMed]
- Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self-management education. Diabetes Educ 2007;33:599-600, 602-4, 606 passim. [Crossref] [PubMed]
- Jacoby A, Austin JK. Social stigma for adults and children with epilepsy. Epilepsia 2007;48:6-9. [Crossref] [PubMed]
- McGrother CW, Bhaumik S, Thorp CF, et al. Epilepsy in adults with intellectual disabilities: prevalence, associations and service implications. Seizure 2006;15:376-86. [Crossref] [PubMed]
- Rosen KB. Beyond Self-Management: Antecedents and Consequences of Team Empowerment. Academy of Management Journal 1999;42:58-74.
(English Language Editor: B. Draper)






