
The effects of hypothermia in thrombosis: a systematic review and meta-analysis
Introduction
Thrombotic diseases are life threatening and seriously threaten human health. They include many common diseases such as coronary heart disease, myocardial infarction, ischemic stroke, venous thrombosis, and pulmonary thromboembolism (1-3). The incidence rate, disability rate, and mortality rate of thrombotic diseases are very high. Thrombus is mainly divided into white thrombus, mixed thrombus, red thrombus, and transparent thrombus. It can be prevented by taking part in physical activities, increasing high-density lipoprotein (HDL), and medication (4-6).
A thrombus is a small clot of blood formed on the surface of a vessel or repair of the internal surface of the cardiovascular system. Variable fluid-dependent type clots are composed of insoluble fibrin, deposited platelets, accumulated white blood cells, and trapped red blood cells (7-9). Thrombosis is a multifactorial process in which a group of genetic and environmental factors interact and influence each other. The most common clinical characteristics of patients with thrombosis are hereditary, recurrent, severe symptoms, abnormal thrombosis sites, and younger onset time.
The normal body temperature of a healthy person generally fluctuates between 36.5 and 37.5 °C in a healthy state, which is a relatively constant value. It is regulated by the body temperature center in the hypothalamus (10,11). The heat generated by the human body usually maintains a balance with the heat emitted; however, during surgery, this balance is destroyed for various reasons, resulting in hypothermia (34–36 °C). Studies have shown that intraoperative hypothermia is very harmful to patients. It is linked with an increased infection rate of surgical incision, affects the body’s coagulation, cardiovascular, and central nervous system function, and metabolism (12,13).
The correlation between hypothermia and thrombosis (14,15). To address these concerns, we conducted this meta-analysis to evaluate the relationship between hypothermia and thrombosis. This research analyzed more indicators than previous similar meta-analysis and update this topic since we include several recent articles. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1925).
Methods
Search strategy
We performed an electronic search for original articles, clinical trials, reviews, and meta-analyses published between 2000 and 2020. We searched the databases of PubMed, Embase, the Cochrane database, and China National Knowledge Infrastructure (CNKI), using the keywords: (I) low temperature; (II) thrombosis. Boolean operators OR and AND Boolean operators are used to search for combining words with different meanings. To achieve the maximum sensitivity of the search strategy and identify all studies, we manually screened the reference lists of all retrieved articles to identify potentially relevant studies further.
Eligibility criteria
The inclusion criteria were as follows: (I) considered to be randomized trials or controlled studies; (II) the hypothermia group was compared with the normothermia group; (III) complications that occurred during the treatment were clearly recorded; (IV) no overlapping data. The exclusion criteria were as follows: (I) other health problems were the research subject; (II) patients received other diagnostic technology; (III) there was a lack of available data on the research. The title and abstract of the articles were independently evaluated by two researchers to determine whether they met the inclusion and exclusion criteria. When there was a difference in opinion on a document, the two authors resolved the problem through mutual discussion and requested help from a third author if necessary.
Data collection and quality assessment
We carefully read the full text of the article and extract features from each study. The data extracted from these studies include the first author's name, country, year of publication, gender, language, sample age, sample size, and the research period of each article. Then, we used the revised Cochrane bias risk assessment tool to assess the overall quality of the included studies tool (https://methods.cochrane.org/risk-bias-2).
Statistical analysis
All the meta-analyses were performed with the software Review Manager 5.2 (RevMan, The Cochrane Collaboration, 2013) and bias analysis of the studies were conducted to examine the quality of articles. A funnel plot was used to estimate publication bias. Review Manager was used to evaluate the overall results between the hypothermia group and the normothermia group. The odds ratio (OR) of 95% confidence interval (CI) was calculated to estimate the relationship between intraoperative hypothermia group and normothermia group on complications. When I2>50%, we considered that there was heterogeneity and selected the random effects model; otherwise, the fixed effects model was selected for analysis. For all statistical comparisons, a P value of less than 0.05 was considered statistically significant.
Results
Study selection
The preliminary result of our electronic search is 892 articles. After careful reading, 90 papers meet the primary standards. In further screening, 82 articles were excluded due to inconsistent research design, insufficient data and inconsistent article types. Finally, eight papers are selected for analysis. Figure 1 shows a flowchart of identification, inclusion, and exclusion.
Study characteristics
Table 1 summarizes the types of studies reported and the total number of patients associated with each group, including author, year of publication, language, country, gender, age, sample size and collection time (16-23). A total of 2,053 samples were collected from 2000 to 2019, and 8 articles were published, with sample sizes of 43–615. The participants included 1,417 women and 636 men.
Table 1
| Study | Year | Language | Country | No. of patients (male/female) | Age range (mean) | No. of hypothermia group | No. of normothermia group | Years of onset |
|---|---|---|---|---|---|---|---|---|
| Achim | 2014 | English | Switzerland | 32/11 | 57.1±12.2 | 22 | 21 | January 2011 to March 2013 |
| Andremon | 2017 | English | France | 400/201 | 60.6±15.1 | 89 | 512 | August 2012 to November 2014 |
| Dae | 2017 | English | America | 250/67 | 65±13.2 | 157 | 160 | January 2003 to August 2010 |
| Garcýa | 2018 | English | Spain | 124/21 | 59.8±11.7 | 105 | 40 | May 2005 to July 2016 |
| Joffre | 2014 | English | France | 166/42 | 60.3±12.3 | 55 | 153 | August 2000 to January 2012 |
| Moellhoff | 2020 | English | Germany | 343/272 | 51.9±27.8 | 271 | 244 | June 2012 to March 2019 |
| Nichol | 2015 | English | America | 46/8 | 57.3±8.7 | 28 | 26 | January 2013 to January 2014 |
| Zhang | 2019 | English | China | 56/14 | 62.7±6.8 | 35 | 35 | March 2013 to June 2017 |
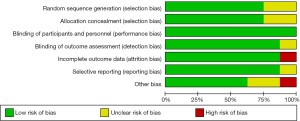
Risk of bias in studies
The quality of the studies was assessed though the risk of bias table in the Review Manager 5.2 Tutorial (24), and the evaluation is shown in Figures 2,3. The assessment revealed limited bias among the included articles. Only 1 study showed the problem of selection bias. From the summary of deviations, there were no problems in selection deviation, performance deviation, loss deviation, and reporting deviation. Generally speaking, there were 2 trials with risk of bias and 6 trials without risk.
Results of individual studies
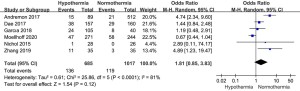
Figure 4 shows the forest map of intraoperative thrombosis in the hypothermia group and normothermia group participants. A total of 8 studies were involved in the analysis. The analysis showed that there were differences between the two groups. The probability of intraoperative thrombosis in the hypothermia group was higher than that in the normothermia group (OR =1.89, 95% CI: 0.87 to 4.13, P=0.0003, I2=74%).
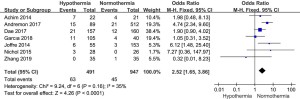
Figure 5 shows a forest plot of intraoperative mortality in patients in the hypothermia and normothermia groups. A total of 5 studies were involved in the analysis. The analysis showed that there were differences between the two groups. The probability of intraoperative death in the hypothermia group was higher than that in the normothermia group (OR =2.84, 95% CI: 0.61 to 13.27, P<0.00001, I2=89%).
Figure 6 shows a forest plot of the probability of massive intraoperative bleeding in participants in the hypothermia and normothermia groups. A total of 6 studies were involved in the analysis, and it was revealed that there were differences between the two groups. The probability of massive intraoperative bleeding in the hypothermia group was higher than that in the normothermia group (OR =1.81, 95% CI: 0.85 to 3.83, P<0.0001, I2=81%).
Results of sensitivity analysis and publication bias
Sensitivity analysis was performed to test the stability of the results. After eliminating the relative outliers, the sensitivity of or value of heterogeneity decreased from 74% to 35%. The results showed that this heterogeneity was mainly due to the study by Moelhoff et al. in 2020. A forest map without the article by Moelhoff et al. is shown in Figure 7.
Funnel plot analysis was used to analyze the probability of thrombosis in the hyperthermia group and normothermia group. All 8 studies were included in the plot. To some extent, the results showed that there was limited publication bias due to the good symmetry of funnel plot (Figure 8).
Discussion
There are three factors of thrombosis include vascular wall injury, slow blood flow rate and hypercoagulable state. Problems in any of these three aspects can lead to thrombosis. Vascular wall damage is more common in patients with a history of venipuncture, deep venous catheterization or surgical injury of blood vessels, which can lead to thrombosis. Patients with coagulation factor disorder, hemophilia, thrombophilia or lack of coagulation factor can lead to early thrombosis after operation. There are also some factors, such as changes in blood flow status, long-term bed rest, malignant tumors, major surgery, severe blood loss after surgery, and more fluid loss after surgery, which can lead to slow blood flow and thrombosis (24-26). Intraoperative hypothermia increases the risk of incision infection and bleeding. We identified 8 studies that met the inclusion criteria to assess the effect of intraoperative hypothermia on promoting thrombosis. These studies showed that the incidence of thrombosis and mortality in the hypothermia group were higher than those in the normothermia group. Active body temperature management can reduce the incidence of thrombosis and mortality, otherwise there is risk. Our results are consistent with the report by Jin et al. (24).
Thrombosis and thromboembolism are two kinds of diseases caused by pathological processes, and are clinically called thrombotic diseases (25-28). According to reports, thrombus can be divided into venous thrombosis, arterial thrombus and microthrombus according to the anatomical position. According to the thrombus composition, it can be divided into platelet thrombus, red blood cell thrombus, mixed thrombus and fibrin thrombus (29-31). Thrombotic diseases seriously threaten human health and life. Their incidence rate is the highest (1.35%) among various diseases and has been increasing gradually in recent years.
Thrombotic disease results from abnormal blood clots in the circulatory system (32,33), for which there are three causes: vascular damage, blood changes, and blood stasis. Thrombosis is a group of complications caused by many different diseases and causes. Due to the difference of various basic diseases and the location of thromboembolism, the clinical manifestations of thrombosis are also different.
The body dynamically balances heat production and heat dissipation through the thermoregulatory center, so as to maintain the core temperature at 36±0.4 °C. Due to the large area and extended duration of exposure of internal organs or limbs during surgery, infusion of a large amount of room temperature liquid, repeated and prolonged washing of the operation area, and the inhibitive effect of anesthetics on the body’s thermoregulatory function, the body temperature of patients falls below the normal range during surgery (34,35). Intraoperative hypothermia is very harmful to patients, especially the elderly and children, as it can increase oxygen consumption, increase heart rate, worsen coagulation function, damage immune function, and even endanger life.
In conclusion, the incidence of thrombosis and mortality in the hypothermia group were higher than those in normothermia group.
There were some limitations to this paper. First, comparisons between the same diseases were not considered, which should be evaluated in further studies (36-38). Second, the details of the complications were not included, which should also be evaluated in the future.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1925
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1925). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Leonov Y, Sterz F, Safar P, et al. Mild cerebral hypothermia during and after cardiac arrest improves neurologic outcome in dogs. J Cereb Blood Flow Metab 1990;10:57-70. [Crossref] [PubMed]
- Vollmer C, Nommensen J, Watolla M, et al. Influence of thoracic epidural anesthesia on gastric oxygenation during hypothermia and hemorrhage. Auton Neurosci 2016;195:1-7. [Crossref] [PubMed]
- Cheng J, Fu Z, Zhu J, et al. The predictive value of plasminogen activator inhibitor-1, fibrinogen, and D-dimer for deep venous thrombosis following surgery for traumatic lower limb fracture. Ann Palliat Med 2020;9:3385-92. [Crossref] [PubMed]
- Su Y, Fan L, Zhang Y, et al. Improved Neurological Outcome With Mild Hypothermia in Surviving Patients With Massive Cerebral Hemispheric Infarction. Stroke 2016;47:457-63. [Crossref] [PubMed]
- Feng G, Feng L, Zhao Y. Association between ratio of γ-glutamyl transpeptidase to high-density lipoprotein cholesterol and prevalence of nonalcoholic fatty liver disease and metabolic syndrome: a cross-sectional study. Ann Transl Med 2020;8:634. [Crossref] [PubMed]
- Thuillier R, Hauet T. Impact of Hypothermia and Oxygen Deprivation on the Cytoskeleton in Organ Preservation Models. Biomed Res Int 2018;2018:8926724 [Crossref] [PubMed]
- Polderman KH, Varon J. How low should we go? Hypothermia or strict normothermia after cardiac arrest? Circulation 2015;131:669-75. [Crossref] [PubMed]
- Perich P, Tuchtan L, Bartoli C, et al. Death from Hypothermia during a Training Course under "Extreme Conditions": Related to Two Cases. J Forensic Sci 2016;61:562-5. [Crossref] [PubMed]
- Pastukhov A, Borisova T. Levetiracetam-mediated improvement of decreased NMDA-induced glutamate release from nerve terminals during hypothermia. Brain Res 2018;1699:69-78. [Crossref] [PubMed]
- Muth CM, Mainzer B, Peters J. The use of countercurrent heat exchangers diminishes accidental hypothermia during abdominal aortic aneurysm surgery. Acta Anaesthesiol Scand 1996;40:1197-202. [Crossref] [PubMed]
- Mota CMD, Borges GS, Amorim MR, et al. Central serotonin prevents hypotension and hypothermia and reduces plasma and spleen cytokine levels during systemic inflammation. Brain Behav Immun 2019;80:255-65. [Crossref] [PubMed]
- Morgan M, Schwartz L, Duflou J. Hypothermia secondary to glioblastoma multiforme? Autopsy findings in two cases. J Forensic Sci 2015;60:511-3. [Crossref] [PubMed]
- Mattingly TK, Denning LM, Siroen KL, et al. Catheter based selective hypothermia reduces stroke volume during focal cerebral ischemia in swine. J Neurointerv Surg 2016;8:418-22. [Crossref] [PubMed]
- Khalilov RA, Dzhafarova AM, Dzhabrailova RN, et al. The kinetic and thermodynamic characteristics of lactate dehydrogenase in the rat brain during hypothermia. Neurochemical Journal 2016;10:156-65. [Crossref]
- Holaday JW, Tseng LF, Loh HH, et al. Thyrotropin releasing hormone antagonizes beta endorphin hypothermia and catalepsy. Life Sci 1978;22:1537-44. [Crossref] [PubMed]
- Zhang Z, Xu M, Wu D, et al. Postoperative Myocardial Injury in Middle-Aged and Elderly Patients Following Curative Resection of Esophageal Cancer With Aggressive or Standard Body Temperature Management: A Randomized Controlled Trial. Anesth Analg 2019;129:352-9. [Crossref] [PubMed]
- Andremont O, du Cheyron D, Terzi N, et al. Endovascular cooling versus standard femoral catheters and intravascular complications: A propensity-matched cohort study. Resuscitation 2018;124:1-6. [Crossref] [PubMed]
- Nichol G, Strickland W, Shavelle D, et al. Prospective, multicenter, randomized, controlled pilot trial of peritoneal hypothermia in patients with ST-segment- elevation myocardial infarction. Circ Cardiovasc Interv 2015;8:e001965 [Crossref] [PubMed]
- Müller A, Lorenz A, Seifert B, et al. Risk of thromboembolic events with endovascular cooling catheters in patients with subarachnoid hemorrhage. Neurocrit Care 2014;21:207-10. [Crossref] [PubMed]
- Moellhoff N, Broer PN, Heidekrueger PI, et al. Impact of Intraoperative Hypothermia on Microsurgical Free Flap Reconstructions. J Reconstr Microsurg 2021;37:174-80. [Crossref] [PubMed]
- Joffre J, Varenne O, Bougouin W, et al. Stent thrombosis: an increased adverse event after angioplasty following resuscitated cardiac arrest. Resuscitation 2014;85:769-73. [Crossref] [PubMed]
- García J, Jiménez-Brítez G, Flores-Umanzor E, et al. Thrombotic and Bleeding Events After Percutaneous Coronary Intervention in Out-of-hospital Cardiac Arrest With and Without Therapeutic Hypothermia. Rev Esp Cardiol (Engl Ed) 2019;72:433-5. [Crossref] [PubMed]
- Dae M, O'Neill W, Grines C, et al. Effects of endovascular cooling on infarct size in ST-segment elevation myocardial infarction: A patient-level pooled analysis from randomized trials. J Interv Cardiol 2018;31:269-76. [Crossref] [PubMed]
- Jin Y, Lin Y, Feng JF, et al. Moderate Hypothermia Significantly Decreases Hippocampal Cell Death Involving Autophagy Pathway after Moderate Traumatic Brain Injury. J Neurotrauma 2015;32:1090-100. [Crossref] [PubMed]
- Horikoshi Y, Kimura T, Nishikawa T, et al. Neuroprotective Effects of Combination of Dexmedetomidine and Hypothermia after Asphyxial Cardiac Arrest in Rats. J Cereb Blood Flow Metab 2015;34:14-21.
- Hifumi T, Kuroda Y, Kawakita K, et al. Fever Control Management Is Preferable to Mild Therapeutic Hypothermia in Traumatic Brain Injury Patients with Abbreviated Injury Scale 3-4: A Multi-Center, Randomized Controlled Trial. J Neurotrauma 2016;33:1047-53. [Crossref] [PubMed]
- Debaty G, Moustapha I, Bouzat P, et al. Outcome after severe accidental hypothermia in the French Alps: A 10-year review. Resuscitation 2015;93:118-23. [Crossref] [PubMed]
- Guidash JC, Berman L, Panagos PG, et al. Engaging Frontline Providers Prevents Hypothermia and Improves Communication in the Postoperative Neonate. Adv Neonatal Care 2021;21:379-86. [Crossref] [PubMed]
- Gong P, Zhao H, Hua R, et al. Mild hypothermia inhibits systemic and cerebral complement activation in a swine model of cardiac arrest. J Cereb Blood Flow Metab 2015;35:1289-95. [Crossref] [PubMed]
- Gao XY, Huang JO, Hu YF, et al. Corrigendum: Combination of mild hypothermia with neuroprotectants has greater neuroprotective effects during oxygen-glucose deprivation and reoxygenation-mediated neuronal injury. Sci Rep 2015;5:12195. [Crossref] [PubMed]
- Welsh FA, Harris VA. Postischemic Hypothermia Fails to Reduce Ischemic Injury in Gerbil Hippocampus. J Cereb Blood Flow Metab 2016;20:245-56. [PubMed]
- Sadaka F, Doerr D, Hindia J, et al. Continuous Electroencephalogram in Comatose Postcardiac Arrest Syndrome Patients Treated With Therapeutic Hypothermia: Outcome Prediction Study. J Intensive Care Med 2015;30:292-6. [Crossref] [PubMed]
- Drewry AM, Fuller BM, Skrupky LP, et al. The presence of hypothermia within 24 hours of sepsis diagnosis predicts persistent lymphopenia. Crit Care Med 2015;43:1165-9. [Crossref] [PubMed]
- Goldfarb DA. Re: Therapeutic Hypothermia in Deceased Organ Donors and Kidney-Graft Function. J Urol 2016;195:1549. [Crossref] [PubMed]
- Boylan GB, Kharoshankaya L, Wusthoff CJ. Seizures and hypothermia: importance of electroencephalographic monitoring and considerations for treatment. Semin Fetal Neonatal Med 2015;20:103-8. [Crossref] [PubMed]
- Allard J, Paci P, Vander Elst L, et al. Regional and time-dependent neuroprotective effect of hypothermia following oxygen-glucose deprivation. Hippocampus 2015;25:197-207. [Crossref] [PubMed]
- Nara A, Nagai H, Yamaguchi R, et al. An unusual autopsy case of lethal hypothermia exacerbated by body lice-induced severe anemia. Int J Legal Med 2016;130:765-9. [Crossref] [PubMed]
- Agatiello M, Toffoli E, Scarabel F, et al. Somatosensory evoked potentials recorded during hypothermia in neonatal hypoxic–ischemic encephalopathy. Clinical Neurophysiology 2015;126:e5 [Crossref]
(English Language Editor: J. Jones)







