
Role of direct oral anticoagulants in gastrointestinal cancer associated thrombosis “practical issues in clinical practice”—narrative review
Introduction
Cancer associated thrombosis (CAT) is the second leading cause of death in cancer patients after disease progression (1). Patients with cancer are four to seven times more likely to develop venous thromboembolism (VTE) than patients without cancer. The International Initiative on Thrombosis and Cancer (ITAC) and the American Society of Clinical Oncology (ASCO) have supported the role of direct oral anticoagulants (DOACs) in the management of cancer-associated thrombosis (2,3).
Gastrointestinal (GI) malignancies are associated with an increased risk of bleeding; therefore, several international guidelines and review articles suggest a cautious use of DOACs in this patient group (4). Safety data supporting the use of DOACs in GI malignancies is limited and heterogeneous. According to the Canadian consensus algorithm, patients with active GI malignancies and those taking concomitant medications that would lead to potentially serious drug-drug interactions (DDIs) with DOACs, GI surgery or absorption disorders are considered high risk for DOACs use. These subgroups of patients should be treated with extended duration low molecular weight heparin (LMWH).
Patients with CAT in the setting of GI malignancy represent a unique group with important clinical issues during treatment with DOACs; higher risk of bleeding from primary tumour especially when untreated primary in situ, increased susceptibility to nausea and vomiting due to the tumour itself or chemotherapy protocols used in their management, altered anatomy due to surgery or impact of primary tumour location as well as exposure to different chemotherapy agents with potentially clinically significant interactions with DOACs. There is a paucity of data in regards to GI malignancies in DOACs based on randomised controlled trials (RCTs) and meta-analysis. These factors need careful consideration when managing CAT in this tumour group, and future randomised trials looking at these specific factors in GI malignancies are urgently needed. We present the following article in accordance with the Narrative Review reporting checklist (available at https://dx.doi.org/10.21037/apm-21-658).
Methods
Search strategy
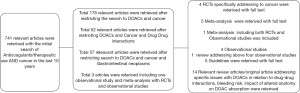
We searched Medline and PubMed Central with MeSH analysis for RCTs, meta-analysis, real-world observational studies (OSs) comparing efficacy and safety of DOACs to LMWH for treatment of CAT. We have also analysed the data from these RCTs specifically for CAT in subsets of GI malignancies. The flow chart in Figure 1 explains the selection of articles included in this review. The details of the search strategy are enclosed in the supplementary file (https://cdn.amegroups.cn/static/public/apm-21-658-1.pdf). We also reviewed the important clinical guidelines published by various expert groups such as the American Society of Clinical Oncology (ASCO), Canadian Consensus Guidelines, International Society of Thrombosis and Haemostasis (ISTH), International Initiative on Thrombosis and Cancer (ITAC), and American Society for Haematology (ASH) for any specific recommendations on DOACs and their use in GI malignancies. We excluded the randomised trials discussing the role of DOACs for prophylaxis in GI malignancies. We comprehensively reviewed the data about bleeding risk [both major and clinically relevant non-major bleeding (CRNMB)]. We specifically reviewed all the data available about GI cancer subtypes in the RCTs. We also reviewed the practical issues of altered bowel anatomy, drug interactions and absorption, the impact of the intact primary on bleeding risk from DOACs in GI malignancies.
Study data were reviewed for the following issues specific to GI cancers:
- Specific tumour types of GI malignancy and the number of specific subtypes of patients included in the RCTs;
- Whether the primary was removed or in situ;
- Metastatic vs. non-metastatic;
- Inclusion and exclusion criteria’s specific to GI malignancies in the RCTs;
- Incidence of major bleed and CRNMB;
- Potential DDIs about specific GI protocols;
- Impact of alteration in GI anatomy on absorption and efficacy of DOACs in various RCTs.
Results
Hokusai VTE Cancer trial (5)
Hokusai VTE Cancer trial was an open-label, non-inferiority, randomised trial comparing anticoagulation with edoxaban (DOAC) vs. dalteparin (LMWH) in patients with cancer who had acute symptomatic or incidental VTE. Of the 1,046 patients, 522 were randomised to the edoxaban group and 524 in the dalteparin group. In the study, 304 (29%) patients had a GI tract malignancy. Table 1 describes the study design, inclusion and exclusion criteria, duration and definition of the primary outcome. Table 2 shows a breakdown of the number of patients with upper and lower GI malignancies in the two arms.
Table 1
| Characteristics of each RCTs | Hokusai-VTE | CARAVAGGIO | Adam VTE | SELECT-D |
|---|---|---|---|---|
| Study design | Randomised, open-label non inferiority trial with blinded central outcome adjudication | Randomised, open-label non inferiority trial with blinded central outcome adjudication | Randomised, open-label superiority trial | Randomised, open-label non inferiority trial with blinded central outcome adjudication |
| Inclusion criteria | Patients with active cancer or cancer diagnosed within 2 years before study inclusion with acute VTE | Patients with active cancer or cancer diagnosed within 2 years before study inclusion with acute VTE | Patients with active cancer or received cancer treatment within the last 6 months with acute VTE | Patients with active cancer; with acute VTE |
| Exclusion criteria | Basal/squamous cell skin cancers | Basal/squamous cell skin cancers | Basal/squamous cell skin cancers | Basal/squamous cell skin cancers |
| ECOG 3-4 | Cerebral metastasis, primary brain tumour | ECOG 3-4 | Weight <40 kg | |
| Aspirin >100 mg or DAPT | ECOG 3-4 | Significant hepatic/renal impairment | Aspirin >75 mg or DAPT | |
| P-glycoprotein inhibitors | Significant hepatic/renal impairment | Active bleeding | Cytochrome P-450 3A4 or P-glycoprotein inhibitors | |
| Significant hepatic/renal impairment | Active bleeding | Cytochrome P-450 3A4 and P-glycoprotein inhibitors | Significant hepatic/renal impairment | |
| Active bleeding | Aspirin >165 mg, DAPT or Thienopyridine treatment | Active bleeding | ||
| Treatment duration | 6 to 12 months | 6 months | 6 months | 6 months |
| Primary outcome | Recurrent VTE; major bleeding | Recurrent VTE | Major bleeding | Recurrent VTE; primary safety outcome was major bleeding events |
RCTs, randomised controlled trials; VTE, venous thromboembolism; ECOG, Eastern Cooperative Oncology Group; DAPT, dual antiplatelet therapy.
Table 2
| RCTs | Hokusai-VTE | Caravaggio | Adam VTE | Select-D | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Edoxaban | Dalteparin | Apixaban | Dalteparin | Apixaban | Dalteparin | Rivaroxaban | Dalteparin | ||||
| Total gastrointestinal malignancy | 165 (31.6%) | 139 (26.5%) | 188 (32.6%) | 187 (32.2%) | 48 (32%) | 57 (38%) | 91 (44.8%) | 86 (42.3%) | |||
| Upper gastrointestinal | 33 (6.3%) | 21 (4%) | 23 (4%) | 31 (5.4%) | 7 (4.8%) | 4 (2.7%) | 15 (7.3%) | 26 (12.8%) | |||
| Pancreatic/hepatobiliary | 49 (9.3%) | 39 (7.4%) | 44 (7.6%) | 43 (7.4%) | 23 (15.6%) | 24 (16.2%) | 21 (10.3%) | 13 (6.4%) | |||
| Colorectal | 83 (15.9%) | 79 (15.1%) | 121 (21%) | 113 (19.5%) | 18 (12.2%) | 29 (19.6%) | 55 (27%) | 47 (23%) | |||
| Intact primary | Unavailable | Unavailable | 145 | 150 | Unavailable | Unavailable | Unavailable | Unavailable | |||
GI, gastrointestinal; RCTs, randomised controlled trials; DOAC, direct oral anticoagulant; CAT, cancer associated thrombosis; VTE, venous thromboembolism.
Recurrent VTE occurred in 41 patients (7.9%) in the edoxaban group and 59 patients (11.3%) in the Dalteparin group (difference in risk, −3.4%; 95% CI, −7.0 to 0.2).
Major bleeding occurred in 36 patients (6.9%) in the edoxaban group and 21 patients (4.0%) in the dalteparin group (difference in risk, 2.9%; 95% CI, 0.1 to 5.6). Of all the major bleeding episodes, 47% of patients taking edoxaban involved the upper GI system, only 14% of patients taking dalteparin experienced an upper GI bleed. Furthermore, in GI cancer patients receiving edoxaban with significant bleeding, the clinical presentation was upper GI bleeding in 71.4% of events (6,7).
This trial had insufficient GI malignancy specific information on bleeding risk in patients with the primary in-situ, specific location, relation to metastatic vs non-metastatic disease. It did not report the impact of altered anatomy (Table 2).
SELECT-D trial (8)
In this multicenter, randomised, open-label pilot trial (8), patients with active cancer who had symptomatic pulmonary embolism (PE), incidental PE, or symptomatic lower extremity proximal vein DVT were recruited. The trial compared rivaroxaban with dalteparin. Four hundred six patients were randomised, and each arm had 203 patients. In the study, 177 (43.5%) patients had GI malignancies. Table 1 describes the study design, inclusion and exclusion criteria, duration and definition of the primary outcome. Table 2 shows the number of patients with upper and lower GI malignancies in the two arms. The 6-month cumulative rate of major bleeding was 4% (95% CI, 2% to 8%) for dalteparin and 6% (95% CI, 3% to 11%) for rivaroxaban (HR, 1.83; 95% CI, 0.68 to 4.96). Corresponding rates of CRNMB were 4% with dalteparin and 13% with rivaroxaban (HR, 3.76; 95% CI, 1.63 to 8.69). The authors concluded that rivaroxaban was associated with relatively low VTE recurrence but higher CRNMB compared with dalteparin. Major bleeding was threefold higher in patients with oesophageal or gastroesophageal cancer treated with rivaroxaban than with dalteparin (36% vs. 11%, respectively). Approximately 73% (8/11) of all major bleeding episodes in the rivaroxaban treated group were related to the GI tract (Table 2). The data and safety monitoring committee (DSMC) reviewed the safety analysis of the first 220 patients. Most CRNMB were GI tract and urinary system related. The DSMC noted a non-significant difference in major bleeding between the arms in the 19 patients with cancer of the oesophagus or gastroesophageal junction. The patients with upper GI cancers were subsequently excluded from enrolment as a precautionary measure.
In this trial, no data was provided on the status of the primary tumour (in-situ or resected/treated with locoregional radiation therapy) and the types of chemotherapy or targeted therapy received in each study drug arm. Treatment duration in the trial was six months, so the results are not generalisable beyond six months (Table 1).
ADAM-VTE trial (9)
The ADAM-VTE trial (9) is a multicentre, open-label superiority trial designed to test the hypothesis that apixaban was associated with a significantly lower rate of major bleeding than dalteparin in the treatment of patients with active malignancy and confirmed VTE. The primary outcome of this trial was major bleeding as described in Table 1. The secondary outcome was the recurrence of VTE. Two hundred eighty-seven patients were recruited in this trial, with 145 patients in the apixaban group and 142 in the dalteparin group. In the study, 105 (36.5%) patients had GI malignancies. Table 2 shows the number of patients in various subsets of upper and lower GI malignancies in the two arms.
There were no major bleeds in the apixaban arm. Two major bleeds (1.4%) occurred in the dalteparin group. The rate of CRNMB was 6.2% in the apixaban arm compared to 4.2% in the dalteparin arm. The trial essentially did not meet predefined primary outcomes as sample size calculations were based on high event rates. We could not extract any specific findings related to the GI malignancies from this small trial.
The limitation of the ADAM-VTE trial as per the authors are:
- The small sample size of 300 patients;
- 5% (16/300) patients were lost to follow up;
- The events rates were low in both the arms for both primary and secondary outcomes.
CARAVAGGIO trial (10)
CARAVAGGIO trial was a multinational, randomised, investigator-initiated, open-label, non-inferiority phase IIIB trial comparing dalteparin with apixaban for the treatment of newly diagnosed proximal DVT and/or PE in patients with cancer (Table 1). The primary outcome of the study was objectively confirmed recurrent VTE during the trial period. The primary safety outcome was major bleeding. Patients with active bleeding or a high risk of bleeding were excluded from this trial. A total of 1,170 patients underwent randomisation, and the arms were well balanced. In the study, 375 (32%) patients had GI malignancy. Table 2 shows the number of patients in various subsets of upper and lower GI malignancies in the two arms. The apixaban arm had a 2.3% low risk of VTE recurrence as compared dalteparin arm with a hazard ratio of 0.63 (95% CI, 0.37–1.07). There were 22 (3.8%) cases of major bleeding in the apixaban arm as compared to 23 (4%) in the dalteparin arm with an HR of 0.82 (95% CI, 0.40–1.69). Eleven (1.9%) major GI bleeds in the apixaban arm compared to 10 (1.7%) in the dalteparin arm. Major non-GI bleeding was 11 (1.9%) in the apixaban arm as compared to 13 (2.2%) in the dalteparin arm. There were two fatal bleeds in the dalteparin arm. CRNMB occurred in 52 (9%) patients in the apixaban arm and 35 patients (6%) in the dalteparin arm in terms of secondary outcome. The authors concluded that oral apixaban was non-inferior to subcutaneous Dalteparin for the treatment of CAT without an increased risk of major bleeding.
Recently the investigators of the CARAVAGGIO trial published the comprehensive results of bleeding with apixaban and dalteparin in the study (11). The major bleeding events had five items:
- Clinically overt bleeding associated with a decrease in haemoglobin of 2 gm/dL or bleeding requiring transfusion of 2 or more units of blood;
- Bleeding occurring at the critical site; or
- Fatal bleeding;
- Bleeding resulting in surgical interventions (note: this was an additional item used in the CARAVAGGIO study).
CRNMB was defined as acute clinically overt bleeding that did not meet the criteria of major bleeding but requiring non-surgical, medical intervention by a health care professional, leading to hospitalisation or increased level of care or prompting evaluation (12). In most of the RCTs, this definition was consistently used to define CRNMB.
In the study, 16 major bleeds occurred in patients with cancer of the GI tract; seven occurred in patients who received apixaban and nine in patients who received dalteparin. There were no major bleeding events in patients with resected upper GI or colorectal cancer. The CRNMB were still higher in patients with GI cancers. There were 22 events of CRNMB in the apixaban group as compared to 9 events in the dalteparin group.
Still, caution is required in patients with upper GI malignancies with in situ primary or untreated primary sites. As shown in Table 2, only 23 patients with upper GI malignancy were included in this study which highlights the need for prospective studies of DOAC in these subgroups of malignancy with CAT.
Meta-analyses of the above four trials
There are five meta-analyses reported in 2020, including all the trials mentioned above (13-17). The most comprehensive meta-analysis was published by Mulder et al. in the blood journal (13). In the primary analysis comprising 2,607 patients restricted to patients with proximal DVT or PE (5,8,9), the risk of recurrent VTE was non significantly lower with DOACs than with LMWH (RR 0.68; 95% CI, 0.39 to 1.17). Conversely, the risk of major bleeding (RR 1.36; 95% CI, 0.55 to 3.35) and CRNMB (RR 1.63, 95% CI, 0.73 to 3.64) was non significantly higher. Mortality was comparable in both groups (RR 0.96; 95% CI, 0.68 to 1.36). The authors concluded that DOACs are an effective treatment option for cancer patients with acute VTE, although caution is needed in patients with a high risk of bleeding (13). This meta-analysis again points to the risk of increased bleeding in GI malignancies with DOACs as compared to LMWH and collected additional unpublished data from the above-mentioned four randomised trials. This included major GI bleeding from Hokusai VTE Cancer trial, bleeding events during the on-treatment period (5,8,9) and bleeding events in all study period (7). The definition of on treatment bleeding was any bleeding up until 3 days after study drug discontinuation (5,7-9).
This meta-analysis also reported that the risk of major bleeding and CRNMB was non-significantly higher with DOACs than with LMWH, with 1.3% additional risk of major bleeding and 4.1% additional risk of CRNMB. GI cancer patients need particular caution as the majority of bleeding events occurred in the GI tract in 36 of 62 events (58%). An increased risk of major GI bleed was observed in the Hokusai-VTE and SELECT-D trial but not in the ADAM-VTE trial. Major bleeding was not increased in the Apixaban group of the CARAVAGGIO trial even though the study included 33% of GI cancers. The authors hypothesise that this may be due to the pharmacodynamic properties of apixaban as compared to other DOACs and the inclusion of a very small number of upper GI malignancy patients.
Issues with drug chemotherapy- related interactions with DOACs in GI malignancy
Drugs that alter CYP3A4 enzyme activity and/or P-glycoprotein pump can alter the plasma concentration of the DOACs leading to clinically significant alterations in their anticoagulation effects. All DOACs are substrates for P-glycoprotein. Apixaban and Rivaroxaban are substrates for Cyp3A4, but Edoxaban is not. The use of strong CYP3A4 medications was an exclusion criterion for the ADAM-VTE, SELECT-D and CARAVAGGIO trials. Hence, in real-world practice, it is best to avoid rivaroxaban in patients on concomitant strong dual Cyp3A4/p-glycoprotein inducer or strong dualCyp3A4/p-glycoprotein inhibitors. Apixaban needs to be avoided with strong dual CYP3A4/p-glycoprotein inducers but can be used at 50% dose with dual Cyp3A4/p-glycoprotein inhibitors (18). In the Hokusai-VTE trial, the dose of Edoxaban was reduced to 30 mg once a day with common p-glycoprotein inhibitors. The trial protocol recommends reducing the edoxaban dose with concurrent use of cancer-specific P-glycoprotein inhibitors (including tyrosine kinase inhibitors) and immunomodulating drugs (including cyclosporin, tacrolimus, and dexamethasone). All these agents required edoxaban dose reduction from 60 to 30 mg. Edoxaban should be avoided in patients on any concomitant P-glycoprotein inducers.
Peixoto de Miranda et al. has recently reported DDIs of 257 antineoplastic and supportive care agents with seven anticoagulants. They reviewed data on seven comprehensive DDI databases and 264 summaries of product characteristics. The only drug class most associated with DDI were tyrosine kinase inhibitors (19).
Cancer patients are commonly treated with combination chemotherapy protocols. Previous comprehensive reviews on this topic suggest an increased risk of interactions when DOACs with various chemotherapy and targeted agents (20). Interestingly no specific recommendations are made in the current ASCO, ITAC, and ASH guidelines on this important clinical issue (2,3,21). The Canadian expert consensus group recommend pharmacist-led drug interaction evaluation, which should be repeated if cancer management changes. The ISTH guidelines also support LMWH in significant DDI of antineoplastic and supportive care drugs with anticoagulants (22).
The Canadian consensus group also recommend the cautious use of DOACs with anticancer regimens associated with significant GI toxicities. The LMWHs might be safer for patients thought to be at higher risk of bleeding. This recommendation has important clinical implications in specific settings such as severe chemotherapy or immunotherapy induced pan-colitis or enteritis.
DOAC’s in patients with GI malignancies who have undergone resections
Patients with GI tract malignancies represent a select group of oncology patients with several unique factors that may significantly impact the absorption and effectiveness of DOACs (23).
Patients with GI malignancy often undergo surgical resection for curative intent or symptom control. Common surgeries which may significantly impact DOAC absorption include total gastrectomy, sleeve gastrectomy, Roux-en-Y gastric bypass (RYGB), pancreaticobiliary diversion with duodenal switch, proximal small bowel resection and colonic resection (23).
Hakeam et al. have reviewed the literature on the effect of major GI tract surgery on the absorption and efficacy of DOACs (24). Table 3 is a modified adaptation from Hakeam et al., which summarises the impact of major surgical interventions on DOACs bioavailability.
Table 3
| Type of DOAC | Total gastrectomy | Partial gastrectomy | RYGB | Distal resection and SBS | Colectomy |
|---|---|---|---|---|---|
| Apixaban | Unlikely affected | Unlikely affected | Unlikely affected | Possibly reduced | Possibly reduced |
| Edoxaban | Possibly reduced | Possibly reduced | Possibly reduced | Unlikely affected | – |
| Rivaroxaban | Reduced up to 56% | Possibly reduced | Possibly reduced | Unlikely affected | Unlikely affected |
DOACs, direct oral anticoagulants; RYGB, Roux-en-Y gastric bypass; SBS, short bowel syndrome.
Prospective data on DOAC use in patients with GI malignancies who have undergone GIT resection is lacking. There are significant theoretical concerns on the influence that GIT resection can have on the absorption and metabolism of DOACs. Until more evidence is available, caution is recommended in using DOACs in patients who have had gastric/proximal small bowel resection/bypass. There is a theoretical possibility that apixaban may be safer due to more distal absorption. However, in the absence of current evidence, LMWH should be the treatment of choice in patients with a history of total gastrectomy. Patients with partial gastrectomy will need close monitoring if treated with Apixaban or other DOACs. Colonic resection is theoretically safer for dabigatran, rivaroxaban and edoxaban. However, we cannot see any safety signals for apixaban in both ADAM-VTE and Caravaggio study, and all DOACs can be safely used in resected lower GI malignancies. Currently, information is missing from all the randomised trials on type of GI surgeries, location of primary and impact on outcomes. Future RCTs should include this valuable information and ideally consider pharmacokinetic or pharmacodynamic studies in the subset of GI cancer patients with major surgeries, which can impact absorption of the DOACs.
Real world data for DOACs use in GI cancers
The real world data from one the registries shows that LMWHs were the most common initial anticoagulation for CAT (25). In this review, the authors reviewed four sizeable real-world data sets for type of anticoagulation therapy for the initial and ongoing management of CAT (25-29). The two most extensive series included in this review included 8,125 and 14,086 patients, respectively. In the first series of 8,125 patients, colon cancer and pancreatic cancer constituted 7.7% and 5.8% of the total cohort. LMWH and unfractionated heparin were prescribed most commonly to the hospitalized patients (35.2% and 27.4%, respectively). The DOACs were only prescribed to 9.6% of patients. The reasons for a lower percentage of DOACs prescriptions were:
- Higher risk of bleeding with specific tumour subtypes;
- DDIs;
- Risk of poor absorption due to nausea, vomiting, mucositis and anatomical changes.
At the time of discharge, DOACs were used more commonly, with 40.3% of patients receiving DOAC compared to 18% of patients receiving LMWH. The compliance was much better with DOACs with only 30% drop out rates compared with 75.9% for LMWH. This dropout rate emphasises that compliance with injectable therapies is poor, and patient preferences are of significant importance in deciding the choice of therapy.
Cohen et al. reported lower events for major bleeding and CRNMB with apixaban as compared to LMWH. This real-world data had 14,086 patients with 51% metastatic disease patients. The rates of recurrent VTE with LMWH as compared to DOACs was 28.8% vs. 15.8%. There were 8.3% more major bleeding events with LMWH as compared to apixaban. Tsoukalas et al. (25) highlight the limitations of these real-world studies which include selection bias, decisions subjected to preferences of treating clinicians, the level of evidence being inferior compared to RCTs. Even with these limitations, these studies add valuable information about the day to day practice and ideas for future research directions.
Recent pooled analysis of direct vs. conventional anticoagulants for treatment of cancer-associated thrombosis reported the pooled and interaction analysis between OSs and RCTs. It included 10 OSs that had 35,142 patients, and 8 RCTs had 2,602 patients. They reported no significant difference in treatment effect estimates between OSs and RCTs. Whereas, increased risk of GI bleeding was found with DOACs versus conventional anticoagulants in CAT patients. The limitation of this study was the inclusion of only two cancer-specific RCTs (Hokusai and Select-D). The authors had no access to the patient-level data about the tumour type, stage, or location (30).
Summary
In conclusion, the recent randomised trials and meta-analyses make DOACs the drug class of choice for the management of VTE in patients with cancer. There is still a need for caution when using DOACs in patients with GI malignancies with VTE given the higher risk of bleeding, especially in patients with intact untreated primary (especially in upper GI cancers). Careful consideration of altered GI anatomy and evaluation of potential DDIs are also required. LMWH may be considered the safer option in this subgroup of patients. However, patient preference and likely compliance with injectable LMWH are also important factors when making the final decision. Overall, we can safely administer DOACs with standard GI malignancy chemotherapy protocols, however specific care should be taken when prescribing DOACs concomitantly with tyrosine kinase inhibitors. Only a small number of patients received bevacizumab or other monoclonal antibodies in the studies, so it will be difficult to draw any conclusions for clinical interactions of monoclonal antibodies with DOACs. There is a need for randomised trials in patients with a specific subset of malignancies such as GI malignancies. Patients with resected lower GI cancers can receive DOACs with the careful assessment of anatomical change as well as evaluating other patient factors and potential drug interactions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-658
Peer Review File: Available at https://dx.doi.org/10.21037/apm-21-658
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-658). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Levitan N, Dowlati A, Remick SC, et al. Rates of initial and recurrent thromboembolic disease among patients with malignancy versus those without malignancy. Risk analysis using Medicare claims data. Medicine (Baltimore) 1999;78:285-91. [Crossref] [PubMed]
- Farge D, Frere C, Connors JM, et al. 2019 international clinical practice guidelines for the treatment and prophylaxis of venous thromboembolism in patients with cancer. Lancet Oncol 2019;20:e566-81. [Crossref] [PubMed]
- Key NS, Khorana AA, Kuderer NM, et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J Clin Oncol 2020;38:496-520. [Crossref] [PubMed]
- Carrier M, Blais N, Crowther M, et al. Treatment algorithm in cancer-associated thrombosis: Canadian expert consensus. Curr Oncol 2018;25:329-37. [Crossref] [PubMed]
- Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism. N Engl J Med 2018;378:615-24. [Crossref] [PubMed]
- Kraaijpoel N, Di Nisio M, Mulder FI, et al. Clinical Impact of Bleeding in Cancer-Associated Venous Thromboembolism: Results from the Hokusai VTE Cancer Study. Thromb Haemost 2018;118:1439-49. [Crossref] [PubMed]
- Ay C, Beyer-Westendorf J, Pabinger I. Treatment of cancer-associated venous thromboembolism in the age of direct oral anticoagulants. Ann Oncol 2019;30:897-907. [Crossref] [PubMed]
- Young AM, Marshall A, Thirlwall J, et al. Comparison of an Oral Factor Xa Inhibitor With Low Molecular Weight Heparin in Patients With Cancer With Venous Thromboembolism: Results of a Randomized Trial (SELECT-D). J Clin Oncol 2018;36:2017-23. [Crossref] [PubMed]
- McBane Ii R, Loprinzi CL, Ashrani A, et al. Apixaban and dalteparin in active malignancy associated venous thromboembolism. The ADAM VTE Trial. Thromb Haemost 2017;117:1952-61. [Crossref] [PubMed]
- Agnelli G, Becattini C, Meyer G, et al. Apixaban for the Treatment of Venous Thromboembolism Associated with Cancer. N Engl J Med 2020;382:1599-607. [Crossref] [PubMed]
- Ageno W, Vedovati MC, Cohen A, et al. Bleeding with Apixaban and Dalteparin in Patients with Cancer-Associated Venous Thromboembolism: Results from the Caravaggio Study. Thromb Haemost 2021;121:616-24. [Crossref] [PubMed]
- Agnelli G, Becattini C, Bauersachs R, et al. Apixaban versus Dalteparin for the Treatment of Acute Venous Thromboembolism in Patients with Cancer: The Caravaggio Study. Thromb Haemost 2018;118:1668-78. [Crossref] [PubMed]
- Mulder FI, Bosch FTM, Young AM, et al. Direct oral anticoagulants for cancer-associated venous thromboembolism: a systematic review and meta-analysis. Blood 2020;136:1433-41. [Crossref] [PubMed]
- Tao DL, Olson SR, DeLoughery TG, et al. The efficacy and safety of DOACs versus LMWH for cancer-associated thrombosis: A systematic review and meta-analysis. Eur J Haematol 2020;105:360-2. [Crossref] [PubMed]
- Giustozzi M, Agnelli G, Del Toro-Cervera J, et al. Direct Oral Anticoagulants for the Treatment of Acute Venous Thromboembolism Associated with Cancer: A Systematic Review and Meta-Analysis. Thromb Haemost 2020;120:1128-36. [Crossref] [PubMed]
- Moik F, Posch F, Zielinski C, et al. Direct oral anticoagulants compared to low-molecular-weight heparin for the treatment of cancer-associated thrombosis: Updated systematic review and meta-analysis of randomized controlled trials. Res Pract Thromb Haemost 2020;4:550-61. [Crossref] [PubMed]
- Ueyama H, Miyashita H, Takagi H, et al. Network meta-analysis of anticoagulation strategies for venous thromboembolism in patients with cancer. J Thromb Thrombolysis 2021;51:102-11. [Crossref] [PubMed]
- O'Connell C, Escalante CP, Goldhaber SZ, et al. Treatment of Cancer-Associated Venous Thromboembolism with Low-Molecular-Weight Heparin or Direct Oral Anticoagulants: Patient Selection, Controversies, and Caveats. Oncologist 2021;26:e8-e16. [Crossref] [PubMed]
- Peixoto de Miranda ÉJF, Takahashi T, Iwamoto F, et al. Drug-Drug Interactions of 257 Antineoplastic and Supportive Care Agents With 7 Anticoagulants: A Comprehensive Review of Interactions and Mechanisms. Clin Appl Thromb Hemost 2020;26:1076029620936325 [Crossref] [PubMed]
- Short NJ, Connors JM. New oral anticoagulants and the cancer patient. Oncologist 2014;19:82-93. [Crossref] [PubMed]
- Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv 2021;5:927-74. [Crossref] [PubMed]
- Khorana AA, Noble S, Lee AYY, et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost 2018;16:1891-4. [Crossref] [PubMed]
- Martin KA, Lee CR, Farrell TM, et al. Oral Anticoagulant Use After Bariatric Surgery: A Literature Review and Clinical Guidance. Am J Med 2017;130:517-24. [Crossref] [PubMed]
- Hakeam HA, Al-Sanea N. Effect of major gastrointestinal tract surgery on the absorption and efficacy of direct acting oral anticoagulants (DOACs). J Thromb Thrombolysis 2017;43:343-51. [Crossref] [PubMed]
- Tsoukalas N, Tsapakidis K, Galanopoulos M, et al. Real world data regarding the management of cancer-associated thrombosis. Curr Opin Oncol 2020;32:289-94. [Crossref] [PubMed]
- Guo JD, Hlavacek P, Poretta T, et al. Inpatient and outpatient treatment patterns of cancer-associated thrombosis in the United States. J Thromb Thrombolysis 2020;50:386-94. [Crossref] [PubMed]
- Papakotoulas P, Tsoukalas N, Christopoulou A, et al. Management of Cancer-associated Thrombosis (CAT): Symptomatic or Incidental. Anticancer Res 2020;40:305-13. [Crossref] [PubMed]
- Sakamoto J, Yamashita Y, Morimoto T, et al. Cancer-Associated Venous Thromboembolism in the Real World- From the COMMAND VTE Registry. Circ J 2019;83:2271-81. [Crossref] [PubMed]
- Cohen AT, Keshishian A, Lee T, et al. Safety and effectiveness of apixaban, LMWH, and warfarin among venous thromboembolism patients with active cancer: a retrospective analysis using four US claims databases. American Society of Hematology, Washington, DC; 2019.
- Gu ZC, Yan YD, Yang SY, et al. Direct versus conventional anticoagulants for treatment of cancer associated thrombosis: a pooled and interaction analysis between observational studies and randomized clinical trials. Ann Transl Med 2020;8:95. [Crossref] [PubMed]


