
Issues related to the health status, work pressure and occupational environments of medical staff at level A tertiary public hospitals in Shanghai
Introduction
Medical staff are the main force behind the construction of a healthy China. Medical staff need to be cared for to achieve, maintain and develop the fundamental life and health interests of the general public. However, due to increasing social pressure, doctors are at high risk for sudden death, overwork and other diseases. According to the “2017 Survey Report on the Survival of Chinese Doctors” and the “2018 White Paper on the Practice of Chinese Physicians”, only 19.2% of physicians believe their health is “good”, and only 22.3% of physicians believe their health does not affect their work. Chinese physicians face high work intensity, high health risks, high overall pressure, and difficulties in guaranteeing professional power, all of which negatively affect medical personnel’s long-term health (1,2). General Secretary Xi Jinping has emphasized that medical personnel are essential in epidemics, and it is important to pay attention to their protection and care. In the “national examination” of national public hospitals, staff satisfaction evaluations are an important assessment index. As medical personnel treat the health of people, society must care for doctors both in periods of epidemic prevention and control, and ordinary times. Thus, it is necessary to pay attention to the physical and mental health of medical staff, establish long-term mechanisms for medical staff care, and take exquisite and precise care of medical staff. We present the following article in accordance with the SURGE reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1777).
Methods
Subjects
The subjects of this study comprised working staff at 10 level A tertiary public hospitals in Shanghai.
Research method
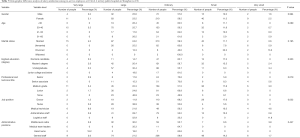
A questionnaire was administered to the study subjects using a random sampling method. 50 employees, including doctors, nurses, medical and technical staff, administrative staff, and logistic staff, were surveyed at each hospital. A total of 500 questionnaires were distributed and 478 questionnaires were collected; thus, there was a recovery rate of 95.6%. The questionnaires were divided into two parts: (I) basic information; and (II) self-evaluation (health status, work stress, practice environment, salary, stress regulation, and motivational factors).
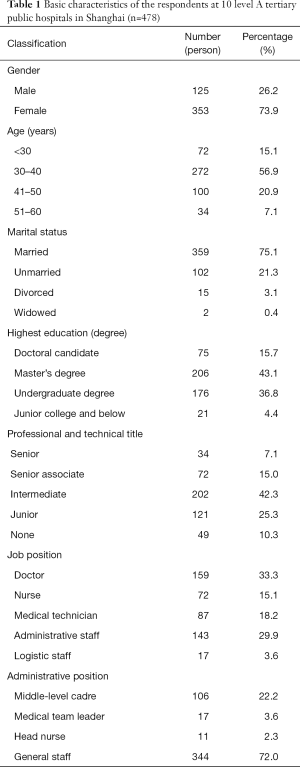
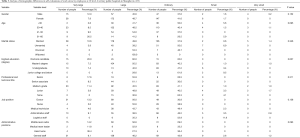
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Shanghai General Hospital (No. 2021KY040) and informed consent was taken from all the patients. The basic characteristics of the respondents are set out in Table 1.
Full table
Statistical analysis
The raw data were organized in an Excel spreadsheet. A database was created, and the further hypothesis testing of the data was conducted using R language. The sample characteristics and survey indicators are described as rates, composition ratios, and other indicators and graphs.
Results
Research results
Self-evaluations of health status
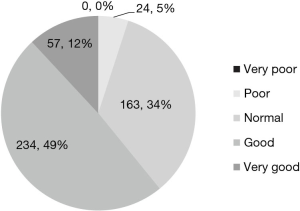
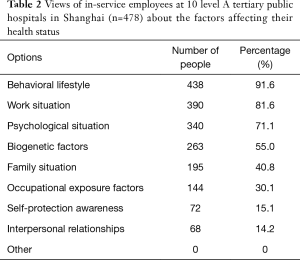
61% of the respondents were of the view that their health status was “good”, 34% that their health status was “average”, and 5% that their health status was “poor” (see Figure 1). According to the frequency of selection, the 4 factors that respondents perceived as most influencing their health status in descending order were behavioral lifestyle (91.6%), work situation (81.6%), psychological situation (71.1%), and biogenetic factors (55.0%) (see Table 2).
Full table
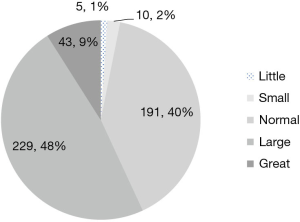
Self-evaluations of work stress
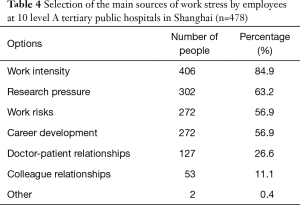
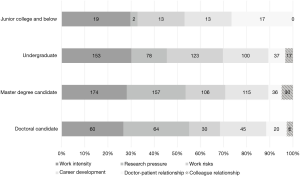
57% of respondents described their work stress as high or very high, 40% as average, and 3% as low or very low (see Figure 2). There were statistically significant differences in the self-evaluations of work stress by medical personnel with different levels of education (degrees). 80% of medical personnel with doctoral degrees described their level of work stress as high or very high, while 57.8%, 49.4%, and 28.6% of respondents with master’s degrees, bachelor’s degrees, and a junior college level of education and below, respectively, described their level of work stress as high or very high (see Table 3). Based on the frequency of selection, respondents viewed the 4 main sources of work stress as work intensity (84.9%), followed by research pressure (63.2%), work risk (56.9%), and career development (56.9%) (see Table 4). According to the results of the cross-tabulation analysis, the primary sources of work stress for doctoral students were scientific research, followed by work intensity. Conversely, the primary sources of work stress for master’s students, undergraduates, and medical staff with a junior college level of education and below were work intensity, followed by scientific research, work risk, and doctor-patient relationships, respectively (see Figure 3).
Full table
Full table
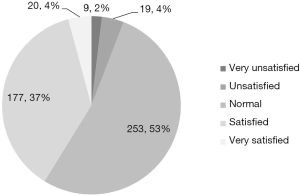
Satisfaction with the practice environment (e.g., doctor-patient relationships)
41% of the respondents thought the practice environment was good, 53% thought that it was average, and 6% were dissatisfied with the practice environment (see Figure 4). There were statistically significant differences in the satisfaction ratings of the practice environment by medical professionals with different job positions. With a level of satisfaction of only 25.2%, physicians were the least satisfied with the practice environment, while medical technicians, nurses, administrative staff, and logisticians had satisfaction levels (from low to high) of 45.9%, 49%, 52.8% and 64.7%, respectively (see Table 5). According to the frequency of selection, the 3 main factors affecting doctor-patient relationships were insufficient communication between doctors and patients (88.7%), followed by a lack of proper recognition on the special nature of medical work by patients (75.1%), and negative media reports (56.7%) (see Table 6).

Full table

Full table
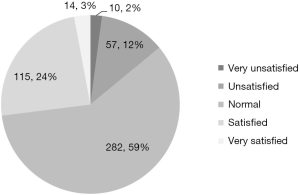
Satisfaction with salary
59% of the respondents expressed moderate satisfaction with their salary, 27% were satisfied or highly satisfied, and 14% were dissatisfied (see Figure 5). There was a statistically significant difference in respondents’ evaluations of satisfaction with salary by medical staff of different job positions. With a satisfaction rate of 52.9%, the logistics staff were the most satisfied with salary, followed by nurses, administrative staff, medical technicians, and physicians, who had satisfaction rates of 41.7%, 31.5%, 28.7%, and 13.2%, respectively (see Table 7). It should be noted that physicians were the least satisfied with salary.
Full table
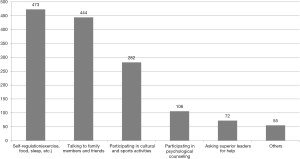
Alleviating stress
The respondents were of the view that the 3 most effective ways to alleviate stress were self-regulation (e.g., exercise, food, and sleep), talking to family members and friends, and participating in cultural and sports activities (see Figure 6).
Motivating factors and demotivating factors
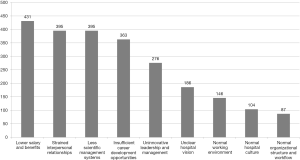
The 5 factors that most motivated the respondents to work hard were better salary and benefits, better career development opportunities, a fairer and more reasonable management system, better leadership and management, and better interpersonal relationships (see Figure 7). The 5 (demotivating) factors that least motivated the respondents to work hard were low salary and benefits, strained interpersonal relationships, poor scientific management systems, insufficient career development opportunities, and un-innovative leadership and management (see Figure 8).
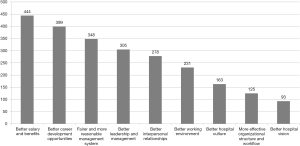
Analysis
The results showed that 61% of the surveyed medical staff were of the view that they were in good health, and 57% were of the view that their work placed them under pressure. Further, more than 50% of the surveyed medical staff were generally satisfied with their practice environments and salaries. In analyzing satisfaction in relation to academic qualifications (degree), job position and other factors, the results showed that the higher the educational background (degree) of an employee, the more work pressure they experienced. Doctoral students cited the pressure of scientific research as their primary work pressure, while medical personnel with other degrees cited work intensity as their primary work pressure. Job risk and career development were also a main source of stress cited by respondents. Doctors were the least satisfied with their practice environments and salaries. Notably, a reasonable salary is the primary factor that motivates medical staff to work hard, and it is also the primary hygiene factor. Thus, any strategy should seek to relieve work pressure, optimize the practice environment and salary, and provide more career development opportunities.
A number of interesting findings were revealed in relation to the major factors affecting the physical and mental health and satisfaction of medical staff. First, as far as the profession is concerned, medical staff are faced with high-tech, high-intensity, and high-risk work pressure, especially at level A tertiary hospitals at which medical staff are responsible for multiple tasks, such as medical treatment, teaching and scientific research. Being in a state of high stress for a long time can cause excessive fatigue (3). Further, superimposed unhealthy behaviors and lifestyles affect physical and mental health. Under the current system, if medical personnel wish to be promoted, they must undertake scientific research, achieve both scientifically and technologically, and publish a certain number of papers. Thus, in addition to the stress related to being busy at work, the stress related to scientific research and career development is also high.
Second, in terms of salary, the training period for medical staff, especially doctors, is quite long, and requires continuous and substantial investment from individuals, families, and the country. The contribution of medical staff to society is also significant. Following the pandemic of the COVID-19, a vast number of medical staff across the country agreed to work in front-line epidemic prevention and control without hesitation, and have made major contributions by protecting the lives and health of people. Given the high investment related to early training, and the high demands and the high output required in later work, the salary of medical staff is not sufficient. Current medical service salaries do not fully reflect the technical and labor value of medical staff, and as a result, medical staff feel that there is a pay-return imbalance. On December 28, 2019, at the 15th meeting of the Standing Committee, the 13th National People’s Congress passed the Basic Medical Hygiene and Health Promotion Law of the People’s Republic, which provides a unique personnel, salary, and reward system that reflects the professional characteristics and technical labor value of medical and health personnel (4,5).
Third, in relation to practice environments, in contrast to the numerous patients being treated at level A tertiary hospitals, there is a relative shortage of medical staff, and patients misunderstand medical work. One-sided reports of public opinion have intensified the conflicts between doctors and patients, and medical disputes have continued to appear, which has placed tremendous mental pressure on medical staff.
Discussion
As is often stated, “cities are built by the people for the people”. Thus, there needs to be a focus on improving the service capacity and management level of hospitals, and the experience of medical personnel in practice. Further, the party organization should be allowed to contact and serve medical personnel. Policies need to be implemented according to position. Additionally, four systems of health protection, welfare benefits, safety assurance, and practice planning need to be introduced that combine commonality and individuality. Expertise and precise care need to be provided to medical staff to effectively protect their legitimate rights and interests. Any plan needs to further improve medical staff’s quality of life, professional identity, and sense of belonging, and vigorously enhance the internal cohesion of hospitals.
Top-level design needs to be led and strengthened by the party committee to establish an overall synergy and consolidate the foundation of employee care
The care of medical staff is a systematic project that involves all aspects of work, study, and life. The needs of medical staff in different positions differ. Thus, it is necessary to strengthen the top-level design and promote it in all aspects. Care for employees should be included in the key tasks of the party committee, and leading and working groups need to be established. The leader of the leading group will be the secretary of the party committee and the dean, and the group members will be leaders from other institutions, who will be responsible for the formulation and guidance of the work plan throughout the process. The working group will include heads of various functional departments, who are responsible for implementing the work plan. The resources of each department should be effectively integrated, the responsibilities of each department consolidated, and a good work pattern for the division of labor, coordination, joint management, and overall advancement established. A caring work evaluation and evaluation mechanism needs to be established to evaluate the effectiveness of the work of the various departments at the end of the year in relation to care. These evaluation results should be incorporated into the annual evaluation results to promote the implementation of the measures and efficiency.
Four major guarantee systems should be established to care for employees with elaboration and precision that combine generality and individuality
Establish a health protection system to maintain the physical and mental health of employees
First, the health management and protection of all employees should be strengthened. To identify common malignant diseases in time, physical examinations should be made available to employees, including additional chest computed technology (CT) examinations, bilateral carotid B-ultrasounds, and cardiovascular and cerebrovascular disease screenings. Employee health files should be kept, and classified health management and continuous tracking should occur if the physical examinations return suspicious results A major illness protection fund should be established to provide timely illness insurance to any employees with major illnesses to alleviate the medical burden of employees.
Second, the psychological counseling and psychological care of some employees who need to relieve the psychological pressure caused by high-intensity work should be strengthened. Balint activities should be held regularly, as the Balint team improves relationships between doctors and patients, allows employees to release their inner emotions, and improves service quality. Psychological outpatient clinics should be established to ease the psychological burden and work pressure placed on medical staff. Timely guidance and interventions should be provided to medical staff who show early signs of mental illnesses.
Third, the rights and interests of employees in relation to communication channels should be safeguarded and a harmonious working environment created. Hospital leaders should lead and regularly attend departments and party branches, strengthen communication with employees through seminars and face-to-face exchanges, keep abreast of the ideological trends of employees, listen to employees’ suggestions and opinions on hospital development and management, employee benefits, and other issues, carefully study and address departmental issues in terms of development in a timely manner, actively assist in coordinating and solving any issues, and relay any solutions to the department or individual who made the suggestion. Thus, a good feedback communication mechanism must be established. Additionally, an online “popular voice channel”, a “mailbox for the leader”, and a “mailbox for the dean” should be set up. Further, a hospital and public opinion platform needs to be established to broaden public opinion feedback channels so that it is easy for employees to voice opinions, offer suggestions, and make requests. This would better serve hospital employees, enhance cohesion, and create a harmonious atmosphere.
Improve the welfare system and create a high-quality living atmosphere
First, a scientific and reasonable performance appraisal and distribution system should be established. To encourage medical reform in public hospitals, this system should focus on key and effective evaluation indicators that reflect the overall strategic goals of hospitals, embody the principles of distribution according to work, and prioritize efficiency and fair evaluation. A scientific and reasonable performance evaluation and distribution system should be established, and a reasonable income growth mechanism for medical staff, especially doctors, should be established to increase the enthusiasm of medical staff.
Second, a high-quality living atmosphere should be created that values life. Hospitals should find and solve practical problems and needs in practical work. The opinions and suggestions of staff should be closely considered to ensure that a care plan suitable to the needs of medical staff is formulated, and practical difficulties are solved in a targeted manner. For example, for newly recruited non-local employees, appropriate housing or rental subsidy policies should be formulated, and talent apartments should be provided to address accommodation issues. For dual-employee families, parent-child winter and summer childcare classes should be offered during vacations to assist employees. In addition, a federation of the labor union, youth league committee, and women should be asked to enrich the cultural and sports life of employees. Investments in and the construction of cultural and sports facilities should be increased so that venues are available for activities, and various cultural and sports activities should be organized to broaden the scope and vision of employees’ communication, strengthen the development of social activities across all walks of life, and relieve the work pressure felt by medical staff.
Strengthen the safety guarantee system and reduce the occupational risks of employees
First, personnel should be rationally deployed, a vacation system for medical staff should be strictly applied, and the work pressures placed on employees should be eased. Clinical front-line work involves heavy tasks, many emergencies and high pressure. Practical and effective measures need to be implemented according to business development and workloads, timely adjustments need to be made to post settings, staff need to be rationally allocated, reasonable working hours need to be set, resting places need to be improved, and a paid vacation system needs to be implemented to avoid continuously overloading medical staff. To relieve the work pressure placed on medical personnel who are responsible for scientific research, the possibility of introducing a leave system for scientific research should be explored, and a period of leave assigned in which medical staff can focus on their scientific research.
Second, medical services should be optimized and harmonious doctor-patient relationships built. The construction of internet hospitals should be promoted, as this would enable patients to enjoy convenient and high-quality medical services anytime from anywhere, and thus improve patient satisfaction. Appointments at different times should be offered to reduce unnecessary waiting time for patients, increase communication between doctors and patients, and build harmonious doctor-patient relationships. A patient experience office should be established to build a communication bridge between doctors and patients, and from the perspective of patients, optimize the service process, improve service efficiency, and improve patient satisfaction. Medical science should be popularized and strengthened to improve patients’ basic knowledge of diseases and understanding of medical work.
Third, the prevention of medical disputes should be strengthened, and the legitimate rights and interests of employees should be protected. Close attention should be paid to potential doctor-patient disputes with a focus on prevention. Further, security, special security and fire safety patrols, and face recognition systems should be introduced at hospitals. Under the operation specifications, emergency alarm buttons should be installed in doctors’ offices and at nurses’ desks. Employee accidental injury insurance should be provided to any medical staff injured in the medical process, and timely medical dispute accidental injury insurance should be provided to ensure staffs’ legal rights are protected.
Implement policies in accordance with individuals, build a career planning system, and open up career development channels
First, staff should be required to formulate personalized career plans, and various types of talents at all levels should be promoted and developed. The career plans of employees should be integrated with the development of hospitals. Formulate development plans with hospital characteristics to classify and guide the development of various types of talents at all levels of hospitals, promote the development of long-term talent, and strengthen hospital talent. In relation to doctors and medical technicians, 3 types of doctor career development channels, including a compound type, a clinical type, and a scientific research type, should be established. In relation to nurses, outstanding young nursing talents and experts should be identified. In relation to nurses and nursing discipline leaders, administrative and logistics staff, a career development channel should be established for the full-time management of talented staff, and corresponding ability standards and training plans introduced. In relation to capable and mediocre employees, talent files should be established and regular talent development assessments conducted. Those who complete the stage goals should continue to be supported; however, those that fail to meet the set goals should be fired. Time should be set aside to foster talent and maintain the development momentum of the hospital.
Second, career promotion channels for all kinds of talents should be established. Based on the different nature of the positions, 7 grades (i.e., physician, medical technology, nursing, research, administration, logistics, and other) should be established so that employees in different positions have sustainable promotion channels.
Acknowledgments
Funding: 2020 Party Building-Ideological and Political Research Project, School of Medicine, Shanghai Jiaotong University (DJ2035).
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1777
Data Sharing Statement: Available at https://dx.doi.org/10.21037/apm-21-1777
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1777). All authors report receiving funding support from 2020 Party Building-Ideological and Political Research Project, School of Medicine, Shanghai Jiaotong University (DJ2035). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Shanghai General Hospital (No. 2021KY040) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lien SSK, Kosik OR, Fan AP, et al. 10-year trends in the production and attrition of Chinese medical graduates: an analysis of nationwide data. Lancet 2016;S11. [Crossref]
- Zhu J, Li W, Chen L. Doctors in China: improving quality through modernisation of residency education. Lancet 2016;388:1922-9. [Crossref] [PubMed]
- Clough BA, March S, Chan RJ, et al. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev 2017;6:144. [Crossref] [PubMed]
- Li Y, Lu C, Liu Y. Medical Insurance Information Systems in China: Mixed Methods Study. JMIR Med Inform 2020;8:e18780 [Crossref] [PubMed]
- Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: progress and gaps in Universal Health Coverage. Lancet 2019;394:1192-204. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


