
A systematic review and meta-analysis compare surgical treatment and conservative treatment in patients with cervical spondylotic myelopathy
Introduction
Cervical spondylotic myelopathy (CSM) is a common chronic progressive disease. It accounts for 10% to 15% of cervical spondylosis, although the etiology of CSM is not clear, it is generally believed to be related to cervical disc degeneration, a high range of motion, or instability of the cervical spine (1-3). Disorders of blood circulation in the spinal cord can also affect the progress of CSM (4). The gradual progression of spinal degeneration affects the diameter of the spinal canal and the range of motion of the cervical spine, and thus, increases the risk of disease (5,6).
CSM is commonly managed by conservative treatment or surgical treatment. MRI is the first choice for the diagnosis of cervical spondylotic myelopathy, with the rapid development of imaging, the diagnosis and surgical management of CSM has also improved (7,8). While surgery has become the treatment of choice for clinicians, there is still some debate regarding the type of surgical method to apply (9,10).
As cervical osteoarthritis degeneration may cause irreversible spinal cord injury, any delay in surgical treatment often leads to poor prognosis (11,12). Therefore, early decompression is usually recommended for patients with moderate or severe CSM (13). However, in patients with mild, non-progressive, or slowly progressive CSM, the condition tends to take a relatively benign natural course and the advantages of surgical treatment over conservative treatment has not been determined (14,15). In such patients, conservative treatment appears to be the preferred choice because it avoids surgical complications and is associated with less financial burden (16,17).
At present, there is no consensus on which method is more favorable for the management of patients with CSM. This meta-analysis compared conservative treatment with surgical treatment in patients with CSM so as to provide evidence-based guidelines for spinal surgeons, which may help patients with CSM. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1365).
Methods
Literature search strategy
A systematic search of the online databases, including PubMed, Embase, Web of Science, and China National Knowledge, was performed from January 2000 to March 2021. The following keywords were used: surgical treatment, conservative treatment, and CSM. The search words were combined using Boolean operators “and”. There were no language restrictions on the literature search. Manual searches of the reference lists of retrieved articles were performed to identify any relevant studies that may had been missed by the search strategy.
Study selection
Articles that met the following inclusion criteria were included in the study: (I) patients were diagnosed with CSM; (II) patients in the experimental group were treated with surgery, and patients in the control group were given conservative treatment; (III) indicators were used to assess the efficacy of surgical treatment and conservative treatment; and (IV) full text articles were available.
Studies were excluded if it did not meet the inclusion criteria, the outcomes of interest were not reported, or the data could not be used. Review articles, abstracts, and duplicate publications were excluded.
Data extraction and quality assessment
After title and abstract screening for potentially eligible studies, two reviewers independently read the full text articles and extracted the following relevant data: name of first author, study design, sample size, patient’s age and gender, year of onset, the study duration, and the primary outcome. The methodological quality of included studies was evaluated with the Cochrane risk of bias assessment tool.
Statistical analysis
Meta-analysis was performed using Review Manager 5.4 software provided by Cochrane. If P<0.05 or I2>50%, it was assumed that there was a certain degree of heterogeneity among the studies, and the random effects model would be used for analysis. If P≥0.05 and I2≤50%, it was assumed that there was no heterogeneity or less heterogeneity between the studies, and the fixed effects model would be used for analysis. The risk ratio (RR) was used to analyze binary variables, mean difference (MD) and 95% confidence interval (CI) was used to analyze continuous variables, and U tests were used to test hypotheses. Sensitivity analysis was conducted by eliminating individual studies sequentially.
Results
Literature selection
A total of 1,145 studies were identified from the database search. Through abstract reading and analysis, 980 articles were excluded as they did not meet the inclusion criteria. A further 70 articles were excluded due to different study design or insufficient data available. Ultimately, 10 papers met the selection criteria and were included in this meta
Characteristics of the included studies
The characteristics of the 10 included studies in this meta-analysis are presented in Table 1. All literature was published between 2000 and 2018. The studies contained a total of 517 patients, of whom 256 were treated with surgery and 261 patients were treated with conservative therapy. The primary outcomes included pre-treatment Japanese Orthopedic Association (JOA) score, post-treatment JOA score, recovery rate, American Spinal Injury Association (ASIA) score and ASIA grade change.
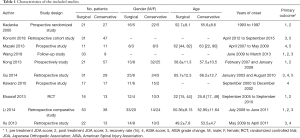
Full table
Assessment of risk of bias
According to the Cochrane risk of bias assessment tool, the methodological quality of the included studies was evaluated for bias risk. Among the 10 articles, high risk of performance bias, attrition bias, and reporting bias was found in 3 different studies (Figure 2). The summary risk of bias assessment for the 10 included studies is illustrated in Figure 3.
Results of heterogeneity tests
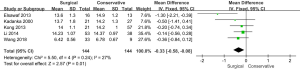
To analyze the difference in pre-treatment JOA scores between the surgical and conservative treatment groups, a meta-analysis was performed to calculate the overall MD using the fixed effects model based on heterogeneity analysis. The MD was −0.33 with 95% CI, −0.58 to −0.08, while the P value of the overall effect was 0.01, I2=27%, which demonstrated that the differences in pre-treatment JOA scores between the surgical and conservative groups were significant (Figure 4). The pre-treatment JOA scores were higher in the conservative treatment group compared to the surgical treatment group.
Similarly, a meta-analysis was conducted to examine the post-treatment JOA scores between the surgical and conservative groups. The results demonstrated that there was no significant difference in post-treatment JOA scores among the two groups (MD: 0.17, 95% CI, −0.70 to 1.05, P=0.70, random effects model), and the included studies were heterogeneous (P=0.0008, I2=79%; Figure 5). The results did not change even after sensitivity analysis by removing the study by Wang et al. (26) (P=0.55, I2=63%).

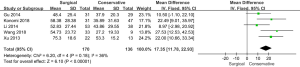
A total of 5 studies involving 306 patients reported the rate of recovery. Meta-analysis showed that compared to the conservative group, the surgical group experienced a higher recovery rate (%) (MD: 17.35, 95% CI, 11.78 to 22.93, P<0.00001, fixed effects model), without significant heterogeneity (P=0.18, I2=36%; Figure 6).
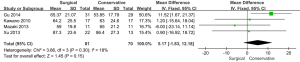
A fixed effects model was used to evaluate the heterogeneity of the ASIA score. Insignificant heterogeneity was detected among the included studies (P=0.30, I2=18%). The results showed that there was no difference between the surgical and conservative groups in terms of ASIA score (MD: 5.17 with 95% CI, −1.83 to 12.18, P=0.15; Figure 7).
A total of three studies reported ASIA grade change. In this meta-analysis, “change” was defined as an increase of at least one grade. The forest plot showed that there was no significant difference between the surgical and conservative groups in terms of ASIA grade change (RR was 2.08 with 95% CI, 0.56 to 7.68, P=0.27, random effects model; Figure 8). While the heterogeneity of the included studies was significant (P=0.003, I2=82%), a sensitivity analysis was conducted by removing the report of Mazaki et al. (18), and the results changed significantly. The P value of the overall effect was 0.0002 and I2 changed from 82% to 0% (P=0.47), which indicated that the homogeneity of the remaining two articles was improved. Furthermore, the results demonstrated that the surgical group promoted a better ASIA grade change compared to the conservative group.

Publication bias
A funnel plot was performed to qualitatively evaluate the publication bias for recovery rate. Figure 9 shows that the shape was fairly symmetric, and the P value of Egger’s test was 0.534, which indicated no significant publication bias existed in this meta-analysis.
Discussion
CSM is a common degenerative disease of the cervical spine, often seen in the elderly (2,3,6,28). The severity of the associated clinical symptoms and signs depends on the pathophysiology of the spinal cord (29). CSM, combined with long-term poor body posture, can result in spinal cord compression or spinal cord ischemia, which can then manifest as a variety of spinal cord dysfunctions.
The decision between surgical treatment versus conservative treatment is affected by many factors, including the disease state, efficacy of treatments, subjective experience of the patient, and a clear understanding of the etiology of the condition.
The traditional view has been that conservative treatment will not prevent the chronic progression of the disease, and surgery is the treatment of choice for most patients. Surgery is usually recommended within 6 months of the onset of disease, with improvements in patient quality of life observed after one year (30,31). Furlan et al. showed that surgical treatment of CSM patients resulted in better prognosis compared to conservative treatment (32). Kaner et al. believed that early surgery could improve neurological function (33). However, a retrospective analysis of patients with mild CSM found that 56% of patients did not need surgical treatment within 10 years after the initial conservative treatment (34). Furthermore, Kadanka et al. did not find any significant difference in patient outcomes between conservative and surgical treatment in the 3-year and 10-year follow-up of the same mild and moderate CSM patients (35,36).
This current meta-analysis examined 10 articles involving 517 patients with CSM. The results showed that the pre-treatment JOA scores in patients in the surgical group were significantly lower than those in the conservative group (P=0.01), but there was no significant difference in post-treatment JOA scores between the surgical and conservative groups, suggesting that the increase in JOA scores after surgery was higher than that after conservative treatment. The recovery rate of patients in the surgical group was significantly higher than that in the conservative group (P<0.00001), and these results were similar to reports by Liu et al. (37). Although this study demonstrated that there was no significant difference in ASIA scores between the two groups (P=0.30), there was a certain difference in ASIA grade change after sensitivity analysis.
Although our study confirmed that surgical treatment was superior to conservative treatment in improving functional recovery of CSM patients, we can not ignore the defects and possible risks of surgical treatment. Firstly, it was important for the choice of surgical methods, not only according to the number of involved segments, but also considering the operator’s operation skills and proficiency, so as to achieve decompression and stability, and avoid surgical complications. Secondly, some studies have confirmed that patients with moderate or severe cervical spondylotic myelopathy were suitable for surgical treatment, however, for patients with mild, non-progressive CSM, surgical treatment had not shown advantage than conservative treatment (14). Therefore, for CSM patients, the choice of surgical methods and treatment timing was very important.
There were some limitations in this study. First, the outcome indicators were not sufficiently comprehensive. The main outcome indicators in the included studies were JOA score, recovery rate, and ASIA score and grade. However, hospitalization time, complications, mortality, and other indicators were less reported, and thus, there was a lack of safety measures. Second, the length of the follow-up period varied in different studies, and this may have affected the final results. Third, this meta-analysis was limited by the quantity and quality of the included studies, and the conclusions should be verified by larger, multicentered, controlled trials with longer follow-up periods.
In summary, surgical treatment is an efficient way for patients with CSM. Compared with conservative treatment, surgery showed a greater increase in JOA score, better recovery rates, and more obvious ASIA grade improvement.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1365
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1365). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lad SP, Patil CG, Berta S, et al. National trends in spinal fusion for cervical spondylotic myelopathy. Surg Neurol 2009;71:66-9; discussion 69. [Crossref] [PubMed]
- Yu Z, He D, Xiong J, et al. Extensor muscle-preserving laminectomy in treating multilevel cervical spondylotic myelopathy compared with laminoplasty. Ann Transl Med 2019;7:472. [Crossref] [PubMed]
- Kalsi-Ryan S, Karadimas SK, Fehlings MG. Cervical spondylotic myelopathy: the clinical phenomenon and the current pathobiology of an increasingly prevalent and devastating disorder. Neuroscientist 2013;19:409-21. [Crossref] [PubMed]
- Cunningham MR, Hershman S, Bendo J. Systematic review of cohort studies comparing surgical treatments for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2010;35:537-43. [Crossref] [PubMed]
- Sah S, Wang L, Dahal M, et al. Surgical management of cervical spondylotic myelopathy. JNMA J Nepal Med Assoc 2012;52:172-7. [Crossref] [PubMed]
- Onifer SM, Zhang YP, Burke DA, et al. Adult rat forelimb dysfunction after dorsal cervical spinal cord injury. Exp Neurol 2005;192:25-38. [Crossref] [PubMed]
- Hori M, Okubo T, Aoki S, et al. Line scan diffusion tensor MRI at low magnetic field strength: feasibility study of cervical spondylotic myelopathy in an early clinical stage. J Magn Reson Imaging 2006;23:183-8. [Crossref] [PubMed]
- Klineberg E. Cervical spondylotic myelopathy: a review of the evidence. Orthop Clin North Am 2010;41:193-202. [Crossref] [PubMed]
- Furlan JC, Kalsi-Ryan S, Kailaya-Vasan A, et al. Functional and clinical outcomes following surgical treatment in patients with cervical spondylotic myelopathy: a prospective study of 81 cases. J Neurosurg Spine 2011;14:348-55. [Crossref] [PubMed]
- Boldin C, Raith J, Fankhauser F, et al. Predicting neurologic recovery in cervical spinal cord injury with postoperative MR imaging. Spine (Phila Pa 1976) 2006;31:554-9. [Crossref] [PubMed]
- Jones JG, Cen SY, Lebel RM, et al. Diffusion tensor imaging correlates with the clinical assessment of disease severity in cervical spondylotic myelopathy and predicts outcome following surgery. AJNR Am J Neuroradiol 2013;34:471-8. [Crossref] [PubMed]
- Zariffa J, Kapadia N, Kramer JL, et al. Feasibility and efficacy of upper limb robotic rehabilitation in a subacute cervical spinal cord injury population. Spinal Cord 2012;50:220-6. [Crossref] [PubMed]
- Rao RD, Gourab K, David KS. Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am 2006;88:1619-40. [Crossref] [PubMed]
- Gok B, Sciubba DM, McLoughlin GS, et al. Surgical treatment of cervical spondylotic myelopathy with anterior compression: a review of 67 cases. J Neurosurg Spine 2008;9:152-7. [Crossref] [PubMed]
- Ghasemi AA, Behfar B. Outcome of laminoplasty in cervical spinal cord injury with stable spine. Asian J Neurosurg 2016;11:282-6. [Crossref] [PubMed]
- Chagas H, Domingues F, Aversa A, et al. Cervical spondylotic myelopathy: 10 years of prospective outcome analysis of anterior decompression and fusion. Surg Neurol 2005;64 Suppl 1:S1:30-5; discussion S1:35-6.
- Berry JG, Harrison JE, Yeo JD, et al. Cervical spinal cord injury in rugby union and rugby league: are incidence rates declining in NSW? Aust N Z J Public Health 2006;30:268-74. [Crossref] [PubMed]
- Mazaki T, Ito Y, Sugimoto Y, et al. Does laminoplasty really improve neurological status in patients with cervical spinal cord injury without bone and disc injury? A prospective study about neurological recovery and early complications. Arch Orthop Trauma Surg 2013;133:1401-5. [Crossref] [PubMed]
- Kadanka Z, Bednarík J, Vohánka S, et al. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J 2000;9:538-44. [Crossref] [PubMed]
- Kong LD, Meng LC, Wang LF, et al. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med 2013;6:852-6. [Crossref] [PubMed]
- Elsawaf A. Outcome of surgical versus conservative management of cervical spine myelopathy secondary to cervical tuberculosis. Neurosurg Rev 2013;36:621-8; discussion 628. [Crossref] [PubMed]
- Konomi T, Yasuda A, Fujiyoshi K, et al. Clinical outcomes of late decompression surgery following cervical spinal cord injury with pre-existing cord compression. Spinal Cord 2018;56:366-71. [Crossref] [PubMed]
- Li FN, Li ZH, Huang X, et al. The treatment of mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spinal Cord 2014;52:348-53. [Crossref] [PubMed]
- Kawano O, Ueta T, Shiba K, et al. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: a multicenter prospective study. Spinal Cord 2010;48:548-53. [Crossref] [PubMed]
- Gu Y, Chen L, Dong RB, et al. Laminoplasty versus conservative treatment for acute cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J 2014;14:344-52. [Crossref] [PubMed]
- Wang J, Li J, Cai L. Effects of Treatment of Cervical Spinal Cord Injury without Fracture and Dislocation in A Medium-to Long-Term Follow-Up Study. World Neurosurg 2018;113:e515-20. [Crossref] [PubMed]
- Xu Z, Xiong M, Zeng Q, et al. Comparison of Operative and Conservative Therapy for Central Cervical Cord Injury without Fracture and Dislocation. Chinese Journal of Clinical Medicine 2013;20:321-323.
- Holly LT, Matz PG, Anderson PA, et al. Clinical prognostic indicators of surgical outcome in cervical spondylotic myelopathy. J Neurosurg Spine 2009;11:112-8. [Crossref] [PubMed]
- Baron EM, Young WF. Cervical spondylotic myelopathy: a brief review of its pathophysiology, clinical course, and diagnosis. Neurosurgery 2007;60:S35-41. [Crossref] [PubMed]
- Papadopoulos SM, Selden NR, Quint DJ, et al. Immediate spinal cord decompression for cervical spinal cord injury: feasibility and outcome. J Trauma 2002;52:323-32. [Crossref] [PubMed]
- Fehlings MG, Vaccaro A, Wilson JR, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the Surgical Timing in Acute Spinal Cord Injury Study (STASCIS). PLoS One 2012;7:e32037 [Crossref] [PubMed]
- Furlan JC, Fehlings MG. Hyponatremia in the acute stage after traumatic cervical spinal cord injury: clinical and neuroanatomic evidence for autonomic dysfunction. Spine (Phila Pa 1976) 2009;34:501-11. [Crossref] [PubMed]
- Kaner T, Sasani M, Oktenoğlu T, et al. Clinical outcomes following cervical laminoplasty for 19 patients with cervical spondylotic myelopathy. Turk Neurosurg 2009;19:121-6. [PubMed]
- Fehlings MG, Wilson JR, Kopjar B, et al. Efficacy and safety of surgical decompression in patients with cervical spondylotic myelopathy: results of the AOSpine North America prospective multi-center study. J Bone Joint Surg Am 2013;95:1651-8. [Crossref] [PubMed]
- Kadanka Z, Mares M, Bednaník J, et al. Approaches to spondylotic cervical myelopathy: conservative versus surgical results in a 3-year follow-up study. Spine (Phila Pa 1976) 2002;27:2205-10; discussion 2210-1. [Crossref] [PubMed]
- Kadaňka Z, Bednařík J, Novotný O, et al. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J 2011;20:1533-8. [Crossref] [PubMed]
- Liu Y, Qi M, Chen H, et al. Comparative analysis of complications of different reconstructive techniques following anterior decompression for multilevel cervical spondylotic myelopathy. Eur Spine J 2012;21:2428-35. [Crossref] [PubMed]
(English Language Editor: J. Teoh)






