
The effect of Plan-Do-Check-Act cycle nursing management of gynecological surgery: a systematic review and meta-analysis
Introduction
The operating theatre is a location for surgical implementation related to the treatment and diagnosis of patients. It is also one of the most important locations where medical activities are performed. Surgical management requires medical staff to standardize nursing management, strictly carry out various nursing operations, improve the quality of nursing management, and reduce the possibility of risks during surgery. At the same time, nursing staff needs to pay attention to the emotional status of patients to ensure patients do not get distressed and to promote recovery from illness. In particular, gynecological surgery involving women and girls with poor immunity and high susceptibility to disease have a number of risks. There are slight differences in the rate for gynecological surgical infections among different hospitals in China, with a general incidence between 0.5% and 3%. A meta-analysis showed that the incidence of incision infection during cesarean sections is about 1.8% in hospitals with Grade-II or above in Chinese Hospital Classification Standard. In particular, the incidence of incision infection in secondary institutions (2.3%) was higher than that in tertiary institutions (1). The most commonly performed gynecological surgeries are cesarean sections, hysteroscopies, and laparoscopic surgeries; for all of these procedures, the risk of surgical infection is extremely high. The infection has serious consequences and affects maternal and child health. Therefore, high-quality nursing care is critical in these contexts.
In recent years, some studies have proposed applying the Plan-Do-Check-Act (PDCA) cycle management in various types of surgical management, where it plays a positive role in the nursing management of the diagnosis and treatment of various diseases (2,3). The PDCA cycle, also known as the Daiming cycle, is an effective way to solve problems and implement solutions (4). Four consecutive stages characterize it: (I) Plan: find, describe, and dissect problems; (II) Do: study and discuss effective countermeasures; (III) Check: test the specific implementation effect of protocols and analyze whether there are methods and measures for improvement; (IV) Act: specifically apply the scheme to clinical practice. The purpose of this meta-analysis is to comprehensively evaluate whether the application of PDCA cycle management has a positive impact on the quality of nursing management following gynecological surgery compared with routine nursing. We present the following article in accordance with the PRISMA reporting checklist (available at https://dx.doi.org/10.21037/apm-21-1590).
Methods
Inclusion criteria
Type of study
Retrospective or prospective clinical trials of PDCA cycle management in gynecological and obstetric surgical care management.
Type of participants
Inclusion criteria: (I) all cases required gynecological surgery after clinical diagnosis; (II) no psychoneurotic disorders, able to communicate normally; and (III) all signed the informed consent form for the clinical trial.
Exclusion criteria: (I) presence of organic disease or mental illness; (II) the patients themselves or their family members were unwilling to participate in the clinical trial; and (III) duplicate study or insufficient data provided.
Intervention type
(I) The control group used the management method of routine clinical nursing; (II) the PDCA cycle management method was applied in the intervention group. The PDCA cycle management method is implemented in the nursing management of patients undergoing gynecological surgery as follows at each step: (i) Plan: the nursing staff needs to develop the nursing management plan and the corresponding quantitative assessment according to nursing needs, work content, surgical methods and the basic situation of patients; (ii) Do: the nursing work at each stage is smoothly implemented, and the planned protocol is evaluated to ensure the hygiene and cleanliness of the patient’s operation and inpatient environment. Moreover, prevention and/or intervention concerning the patient’s psychological status, dietary habits, and complications are implemented as needed. The stability and fluency of the whole nursing process are ensured. (iii) Check: the nursing conditions of the department are checked periodically to detect the shortcomings during the nursing work promptly, and the nursing plane is appropriately adjusted. (iv) Act: adjustments and improvements are made to rectify any problems during nursing to improve the quality of surgical care further.
Result type
The outcome measures of the studies included at least one of the following: satisfaction with nursing care, evaluation of nursing quality, or Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) assessments. The critical value of SAS and SDS scores was 49 and 54 points respectively. Participants with scores below the cut-off values were considered to have no negative emotions. Those with scores above the cut-off scores were considered to have high levels of anxiety and depression.
Research method
Five electronic databases, including PubMed, Web of Science, Embase, China National Knowledge Infrastructure, and Wanfang Database, were searched to identify relevant studies published between 2013 and 2020. Only publications in English and Chinese were included. The searches were performed independently by two reviewers. Keywords included were: “PDCA cycle management, Obstetrics & Gynecology, Surgical Care Management, Meta-analysis”, (“#1 PDCA cycle management method”) and (“#2 Obstetrics and Gynecology” or “obstetrics-gynecology”) and (#3 “Surgical nursing management”) and (#4 “meta analysis”). Different combinations of search words were included to maximize the number of identified studies. In addition, we searched through the reference lists of retrieved studies and review articles to comprehensively identify all relevant studies. The risk of bias in the literature was assessed based on the presence of random allocation methods, allocation concealment, blinding, complete outcome data, and selective reporting.
Data extraction
Two reviewers screened the title, abstract, and keywords of each record identified through the search strategy and retrieved the full text of potentially relevant trials and records of unclear relevance. Each potentially relevant trial was independently screened against the inclusion and exclusion criteria. If there were differences of opinion, they were resolved through discussion with a third reviewer until consensus was reached.
Statistical analysis
Data synthesis: input data to Stata 16.0. Quantitative evaluation of heterogeneity was performed with a Q test and I2. I2=0% indicates that no heterogeneity was observed, and larger values indicate enhanced heterogeneity. A random effects model was applied when I2>50%. Pooling of dichotomous results was reported in the form of odds ratios (ORs) and 95% confidence intervals (CIs), and pooling of numerical results were expressed as standardized mean differences (SMD) and 95% CI. P<0.05 was considered statistically significant. Sensitivity analysis was applied to evaluate the reliability of the results of this meta-analysis.
Results
Research result
We initially screened 207 articles and eliminated 160 ineligible articles based on the title, abstract, and/or full text. Meeting minutes, case reports, and duplicate data were excluded. Finally, 14 articles were included in the meta-analysis (5-18). The literature screening procedure is shown in Figure 1. A total of 1,629 participants were included (815 in the PDCA group, 814 in the control group). The study types were retrospective clinical trials, with sample sizes ranging from 30 to 286. The age of the intervention group participants was between 31.1 and 48.4 years, and the age of the control group members between 30.6 and 48.4 years. There was no statistical difference in the age of participants between the study types. Ten studies compared the satisfaction rate of the two groups of care, seven studies compared quality-of-care scores, and five studies compared SAS and SDS scores. The basic characteristics of the included articles are shown in Table 1.
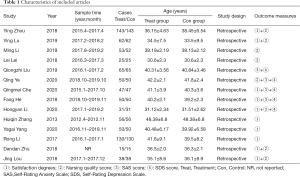
Full table
Meta-analysis and clinical effect evaluation
Satisfaction with nursing care
Ten studies (n=622) reported on the impact of PDCA cycle management on patient satisfaction in gynecological surgical care. The pooled data showed little heterogeneity among studies (I2=0.00%, P=0.980), and the fixed-effect model was used. Meta-analysis showed that after the application of the PDCA cycle management method, nursing satisfaction was significantly higher compared to the control group, OR =6.57 (95% CI, 4.01, 10.76), P<0.001 (Figure 2).
Nursing quality, SAS, and SDS scores
Seven studies (n=647) reported results of nursing quality scores. The studies showed high heterogeneity (P<0.001, I2=97.30%), and as such a random-effects model was used. It was found that the quality-of-care score was significantly improved in the PDCA cycle management group compared with usual care, SMD =4.98 (95% CI 3.32, 6.64), P<0.001 (Figure 3A).
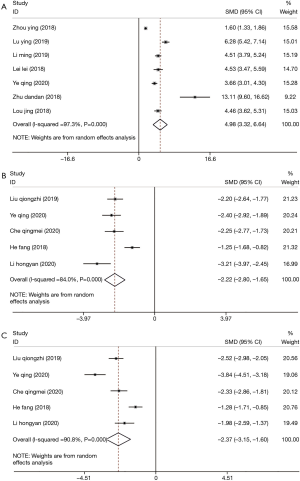
Five studies (n=486) evaluated SAS scores. There was significant heterogeneity among the studies (P<0.001, I2=84.00%), and as such a random-effects model was used. Compared to the control groups, the application of the PDCA cycle management method significantly reduced anxiety scores [SMD =−2.22 (95% CI, −2.80, −1.65), P<0.001] (Figure 3B).
Five studies (n=486) evaluated SDS scores. A heterogeneity test revealed significant heterogeneity (P<0.001, I2=90.80%), and therefore a random-effects model was used. The result showed that the application of the PDCA cycle management method in the intervention group significantly reduced SDS scores [SMD =−2.37 (95% CI, −3.15, −1.60), P<0.001] (Figure 3C).
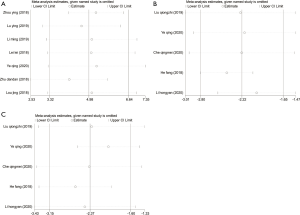
Sensitivity analysis
Sensitivity analysis was performed on the results of nursing satisfaction (Figure 4), nursing quality (Figure 5A), SAS (Figure 5B), and SDS scores (Figure 5C). None of the indices changed after pooling. This indicates that the sensitivity of the results of this included study was low, and the results of this meta-analysis are robust and credible.
Discussion
Modern medical care has developed rapidly, and the operating room is an important place for the diagnosis and treatment of patients in hospitals. Risks and unsafe events during surgery are ubiquitous and uncertain. More and more attention has been paid to risks that occur during medical procedures, and both domestic and international scholars are increasingly studying risks that occur during medical treatments. Perfecting the nursing management system in the operating theatre is conducive to enhancing the doctor-patient relationship, improving the quality of surgery, and better-ensuring treatment and rehabilitation of patients. Traditional routine care has been unable to meet the needs of current diagnosis and treatment service management (19). The PDCA cycle management method has been used widely in clinical practice and is an important approach to improve the quality of care in clinical practice (20-24). This meta-analysis assesses the effects of the PDCA cycle management method applied to the nursing management of gynecological surgery.
A total of 14 relevant studies published between 2013 and 2020 were included in this study. It was found that after the application of the PDCA cycle management method in gynecological surgery nursing, the nursing satisfaction of the intervention groups was significantly higher than that of the control groups. Nursing satisfaction involves aspects such as surgical process, daily nursing quality, professional nursing performance, and nursing service attitude, all of which are closely related to nursing quality. They are key indicators for evaluating the nursing management model and the quality of nursing work, and they can provide a reference for hospital administrators to develop strategies and continuously improve nursing work (25). Applying the PDCA cycle management method as a nursing model improves patients’ perceptions of the quality of nursing services.
Seven studies found that nursing care quality scores were significantly improved in the PDCA cycle management group compared to usual care. This shows that the quality of care for patients receiving PTCA cycle nursing care in obstetrics and gynecology improved and that such patients received quality care services. Five studies found significant reductions in SAS and SDS scores using the PDCA cycle management method. Anxiety and depression are negative emotional states that are detrimental to both the treatment and rehabilitation of the patient’s illness. Studies have found that preoperative anxiety is closely related to postoperative pain (26), and relevant studies have reported that the preoperative anxiety rate of surgery is about 18% to 35% (25). Some studies have also shown that the female gender is an independent risk factor for the development of anxiety, and the incidence of anxiety and depression in female patients is significantly higher than that in male patients (27,28). These findings indicate that reducing patients’ anxiety and depression levels is important, especially in the gynecological surgery population. It can reduce the occurrence of adverse hazards, such as postoperative nausea and vomiting, postoperative pain, etc. (29), which is likely to further enhance treatment’s beneficial effects.
Nursing theory has gradually changed from being patient-centered to meeting the needs of patients at multiple levels, including general nursing, regulation of disease emotions, etc. Therefore, in recent years, the related research on improving the quality of nursing management has gradually increased both domestically and abroad and includes theoretical approaches including self-care defect nursing theory, health promotion model, comfort theory, the Failure Model and Effects Analysis (FMEA) model, and humanized nursing (30). The ultimate purpose of exploring new nursing models is to improve the quality of nursing services. They aim to meet the needs of patients and promote disease rehabilitation. Some recent related studies have also proposed new nursing management models, such as the FMEA model. At present, the theoretical approaches to nursing have not been promoted in clinical practice. The FMEA model is a risk analysis evaluation mode that monitors the risks of a procedure and allows nursing staff to adjust and improve their approach promptly. This can help to eliminate risk factors and improve the quality of care (31-33). Humanized nursing is a patient-centered approach to nursing work. It aims to improve patients’ subjective experience and to promote patients’ active cooperation with treatment (34,35). Only one of the effective models of care was discussed in this meta-analysis. It has not been compared with other evidence-based models of nursing care. New nursing management models require more randomized clinical trials and meta-analyses to study their application effects. The establishment and implementation of high-quality and effective nursing management models also need to be in line with the characteristics of particular hospital settings and the patient’s unique situation.
In conclusion, the implementation of PDCA cycle management can improve satisfaction with nursing services and the quality of nursing care in the operating theatre. At the same time, it can reduce the anxiety and depression levels of patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://dx.doi.org/10.21037/apm-21-1590
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/apm-21-1590). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li Q, Li J, Ma H. Meta analysis on incidence of surgical site infection after cesarean section in secondary and above medical institutions in China. Chinese Journal of Infection Control 2017;12:36-42.
- Ueda A, Saito T, Ueda M, et al. Introduction and PDCA-Management of a Liaison-Clinical Pathway with Cancer Patients after a Curative Operation. Gan To Kagaku Ryoho 2015;42:1197-201. [PubMed]
- Leitmann A, Reinert S, Weise H. Surgical suture course for dental students with the Peyton-4-step approach versus the PDCA cycle using video assisted self-monitoring. BMC Oral Health 2020;20:365. [Crossref] [PubMed]
- Meehan CD, Silvestri A, Street ED. Improving blood glucose monitoring in a hospital setting using the PDCA approach. Plan, do, check, act cycle. J Nurs Care Qual 1993;7:56-63. [Crossref] [PubMed]
- Zhou Y. Effect of PDCA circulation Management on Nursing Quality in Gynaecology and Obstetrics Operating Room. Journal of Rare and Uncommon Diseases 2018;25:48-50.
- Lu Y. Effect of PDCA Circulation Management on Nursing Quality in Gynecological and Obstetric Operating Room. Journal of Mathematical Medicine 2019;32:153-4.
- Li M. Analysis on the effect of PDCA Circulation Management in the Nursing Management in the Department of Gynecology and Obstetrics. China Rural Health 2019;11:62.
- Lei L. Effective application of PDCA Circulation Management in the Nursing Management in the Department of Gynecology and Obstetrics. China Health Industry 2018;358:57-8.
- Liu QZ. Application of PDCA Circulation Management in Gynecological Operation Management. Psychologies 2019;14:76-7.
- Ye Q. Analyze the application value of PDCA circulation management method in nursing management of gynecological surgery. Jia You Yun Bao 2020;2:51-2.
- Che Q. A Study on the Clinical Effect of PDCA Management in Nursing Management of Gynaecology and Obstetrics Surgery. China Health Standard Management 2018;9:189-90.
- He F. A Study on the Clinical Effect of PDCA Management in Nursing Management of Gynaecology and Obstetrics Surgery. Inner Mongolia Medical Journal 2018;50:1536-7.
- Li H, Zhou P. Application and Experience of PDCA Circulation management in Nursing Management of Gynecological Surgery. China Health Care & Nutrition 2020;30:172.
- Zhang H. Evaluation on Application and Effect of PDCA Circulation Method in Gynecological High Quality Nursing. Chinese Journal of Healthy Birth & Child Care 2013;19:136-7.
- Yang Y, Liu S, Li H. Observation on the effect of PDCA Circulation Management in the Nursing Management in the Department of Gynecology and Obstetrics. Clinical Research 2020;28:157-9.
- Li R. Application of PDCA Circulation Management in the Nursing Management in the Department of Gynecology and Obstetrics. China Health Industry 2017;14:1-2.
- Zhu D. Application of PDCA Circulation Management Method in Nursing Management of Gynecological Surgery. Guide of China Medicine 2018;16:258-9.
- Lou J, Guo J. Evaluation on the Effect of PDCA Circulation Nursing Model on the Management of Gynecological Patients. Journal of Modern Medicine & Health 2018;34:1436-17.
- Chen Y, Wang S. Problems and Countermeasures of Hospital Appointment Diagnosis and Treatment Service Management. Journal of Nurses Training 2018;33:730-1.
- Zhang J. Impact of the PDCA Care Management Model on Prevention of Post-extrac-tion Infection and Patient Care Satisfaction. China Health Industry 2020;424:45-7.
- Zhao J. Application Effect and Advantage Analysis of PDCA Nursing Model in Children with Bronchopneumonia. China Practical Medical 2019;14:142-4.
- Wang H. The Application Value of PDCA Mode in Diet Nursing for Children with Allergic Purpura. Chinese and Foreign Medical Research 2020;18:122-4. [Crossref]
- Zhang Y, Zhao R. Effect Evaluation of PDCA Model in PICC Catheter Nursing for Patients with Advanced Hepatocellular Carcinoma. China Medical Herald 2014;11:123-5.
- Zhang B. Effect of PDCA Nursing Model on Angina Pectoris Attack and Quality of Life in Patients with Myocardial Infarction after Discharge. Heilongjiang Medicine And Pharmacy 2019;42:247-8.
- Huang L. Application of Sensitive Nursing Quality Index Based on Evidence-based Theory in Continuous Improvement of Nursing Quality in Operating Room. Laboratory Medicine and Clinic 2017;14:3409-11.
- Gong W, Liu X. Relation of pain threshold and effect of postoperative analgesia with preoperative anxiety in patients with hysteromyoma. Chinese Mental Health Journal 2010;24:86-8.
- Phillips Bute B, Mathew J, Blumenthal JA, et al. Female gender is associated with impaired quality of life 1 year after coronary artery bypass surgery. Psychosom Med 2003;65:944-51. [Crossref] [PubMed]
- Li L, Eamjoy W. The study on the relationship between preoperative anxiety and social support in patients with abdominal operation. Journal of Nurses Training 2000;15:171-4.
- Ali A, Altun D, Oguz BH, et al. The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparascopic cholecystectomy. J Anesth 2014;28:222-7. [Crossref] [PubMed]
- Xu L. Establishment of High Quality nursing service model and its effect analysis. Shan Dong University, 2014.
- Li L, Jiang Y, Liu J, et al. Application of FMEA in reducing incidence of postoperative respiratory tract obstruction after anterior cervical operation. China Practical Medical 2017;12:162-4.
- Chen B, Li X, Zhang Z, et al. Application of FMEA in Preventing Obstetric Patients from Falls. Hospital Management Forum 2017;34:16-8.
- Han Q, Ye Q, Luo Y. Application of failure mode and effect analysis (FMEA) in patients receiving endometrial ablation using NovaSure impedance-controlled system. Journal of Nursing Science 2016;31:19-23.
- Jouzi M, Vanaki Z, Mohammadi E. Factors affecting the communication competence in Iranian nursing students: a qualitative study. Iran Red Crescent Med J 2015;17:e19660 [Crossref] [PubMed]
- Ke M. Influence of Humanized Service on Psychology and Quality of Life of Aged Diabetic Patients. Guangdong Medical Journal 2014;9:1463-4.
(English Language Editors: B. Meiser and J. Chapnick)





