
Balloon kyphoplasty combined with posterior pedicle screw fixation for the treatment of osteoporotic thoracolumbar burst fractures
Introduction
Vertebral burst fracture was proposed by Holdsworth in 1970 (1). In 1983, Denis proposed his 3-column theory (2), in which burst fracture was defined as compression of the anterior and middle column, retropulsion of the fragments into the spinal canal, and vertebral burst fractures in radiological examinations. Clinical data demonstrated that almost 90% of spinal fractures occur at the thoracolumbar junction, and thoracolumbar burst fractures (TLBFs) represent about 10–20% of all spinal fractures (3). Osteoporotic TLBF is a special type of fracture and comprises approximately 13–17.1% of all osteoporotic thoracolumbar compression fractures (TLCFs) (4,5). Compared with pure compression or burst fracture, osteoporotic TLBF is characterized by both osteoporosis and burst fracture. Consequently, the management of osteoporotic TLBFs is a more challenging than that of other vertebral fractures.
Posterior short-segment pedicle screw fixation has been widely accepted and used to treat TLBFs (6,7). However, loss of fracture reduction and screw loosening or breakage are consistently observed in patients with osteoporosis postoperatively. The failure rate has been reported at 53–77% (6,8), which could mainly be attributed to 2 factors: inadequate support for the anterior column of the injured vertebra and weak anchor strength between the bone-screw interfaces. To augment support for the anterior column, anterior instrumentation with strut autografts, mesh cages, and plates have been introduced and shown to be effective. However, the additional anterior surgery inevitably involves a further surgical invasion, more blood loss, lengthened hospital stays, and a higher morbidity (9).
The development of augmented pedicle screws, transpedicle bone grafting, vertebroplasty, and kyphoplasty with polymethylmethacrylate (PMMA) or calcium phosphate has enabled safer and sufficient anterior column reconstructions and vertebral augmentations. Both vertebroplasty and kyphoplasty are effective in managing osteoporotic vertebral fractures, and balloon kyphoplasty appears to provide a better adverse event profile than vertebroplasty (10). However, the condition of vertebral recollapse and implant failure after vertebral augmentation can potentially occur, with an incidence from 3–10% (11,12). Long-segment pedicle screw fixation with vertebroplasty augmentation in segments proximal and distal to the fractured vertebra has provided another alternative procedure to fix osteoporotic TLBFs; however, this procedure prolongs the operation time for up to 4 to 6 hours and increases blood loss (13).
The use of pedicle screws has recently been introduced to strengthen the posterior fixation of TLBFs (14). Pedicle screws in the fractured vertebra serve as mechanical cross-links that provide 3-point stabilization. Biomechanical studies have shown that screws placed at the level of the burst fractures could increase the stiffness of the short-segment fixation. Dick et al. (15) evaluated the biomechanical stability of 4- and 6-screw constructions on the lumbar spines of calves. Their data showed that 6-screw fixation had evident advantages over 4-screw fixation: the axial load stiffness, anti-bending capacity and torsional rigidity were 160%, 80%, and 38%, respectively, which are higher than those of 4-screw fixation. Anekstein et al. (16) also showed that the addition of intermediate screws at the level of a burst fracture significantly increases the stiffness of a short segment pedicular fixation.
In this study, 2 procedures (kyphoplasty and pedicle screw fixation) were combined to treat osteoporotic TLBFs. From February, 2012 to May, 2016, 24 patients with single burst fractures were treated with balloon kyphoplasty combined with posterior pedicle screw fixation in our hospital, and all participants had been experiencing incomplete neurologic impairments. The preliminary results were satisfactory and were reported as follows. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-21-665).
Methods
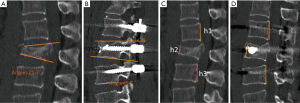
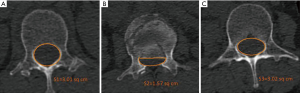
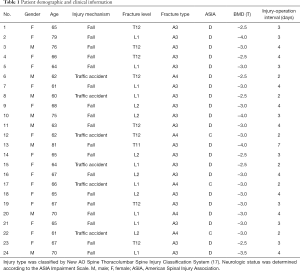
This study was a retrospective case analysis. It was completed in the Spine Surgery Department of Guanghua Hospital from February 2012 to May 2016, and approved by the medical ethical committee of the authors’ institution. A total of 24 patients (8 males and 16 females) with osteoporotic TLBFs were included in the study. The average age was 67 years (60–81 years). The injury mechanism included falls from height (n=18) and traffic accidents (n=6). Physical examinations showed percussion pain of the spinous process at corresponding segments. A neurologic examination showed that all participants had incomplete neurologic deficit. Scans, including X-ray, computed tomography (CT), magnetic resonance imaging (MRI), and bone mineral density (BMD) examinations were routinely performed before the operation. The sagittal spinal curve (Cobb angle), vertebral body height loss (VBHL), and BMD value (T value) were measured and recorded. The Cobb angle was measured from the superior endplate to the inferior endplate of the injured vertebra. The VBHL was defined as the ratio of anterior vertebral height (AVH) to the posterior vertebral height (PVH) and is represented as a percentage. The PVH was calculated according to the average height of the vertebra above and below the fractured vertebra. Both the Cobb angle and VBHL were measured by the Picture Archiving and Communication Systems (PACS, Figure 1). A T value less than −2.5 was regarded as the criteria of osteoporosis. The CT scans showed a spinal canal encroachment of 30–80% (Figure 2). The distribution of the affected vertebra was T11 [1], T12 [8], L1 [9], and L2 [6]. The subtypes of the fractures were A3 (n=19) and A4 (n=5) according to the New AO Spine Thoracolumbar Spine Injury Classification System (17). The patients’ demographic and clinical information (age, gender, injury mechanism, fracture level, fracture type, neurologic status, BMD, and interval from injury to operation) are listed in Table 1.
Full table
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Guanghua Hospital, Shanghai University of Traditional Chinese Medicine (No.: 2019-k-14) and informed consent was taken from all the patients.
Surgical procedure
The surgery was performed under general anesthesia. Patients were placed in a prone position with the abdomen suspended. A posterior median approach was applied. The injured vertebra and its laminar and facet joints were exposed, and the entry points were carefully identified. A total of 4 pedicle screws (EXPEDIUM, Depuy Spine, Raynham, Massachusetts, USA) were bilaterally inserted into the adjacent vertebra above and below the fractured vertebra. For the injured vertebra, 1 screw was placed through the pedicle and the outer sleeve of cannula was implanted on the other side to prepare for kyphoplasty. The position of pedicle screws was checked with anterior-posterior (AP) and lateral fluoroscopic views. Once positioning was satisfactory, a rod of appropriate length was fixed to the pedicle screws on 1 side to temporarily preserve vertebral correction.
An expandable balloon was introduced along the pedicle cannula to the injured vertebral body, and contrast agent was injected for the radiolucent examination. The balloon was slowly inflated to restore the vertebral height under continuous fluoroscopic monitoring. The balloon was then deflated and removed, and PMMA (Tecres S.P.A, Sommacampagna, Italy) was injected until the cement diffusion reached the anterior and middle columns of the injured vertebral body. The pedicle screw was placed along the kyphoplasty channel. A second rod was placed over the pedicle screws to achieve a rigid fixation.
Total laminectomy or hemilaminectomy was performed at the fracture level for the patients with neurological impairments. For patients with retropulsed fragments in the vertebral canal, an L-shaped retractor was used to push the fragments into vertebral column. The dura theca and nerve roots were carefully examined to confirm the absence of compression. Following irrigation of the incision, posterolateral fusion was performed using allograft bone. A total of 2 drainage tubes were routinely retained and the incision was sutured layer by layer.
Postoperative management
After the operation, antibiotic prophylaxis was conventionally used (2 g Cefotiam during operation and 2 g twice in the following 48 hours) and the drainage tubes were removed when the volume of drainage less than 50 mL/d. The patients were encouraged to mobilize while wearing removable plastic jackets starting on the third or fourth day after the operation. Functional lumbar and lower limb exercises that could be performed in bed were advised, with the intensity gradually increased. Both X-ray and CT examinations were performed regularly 1, 2, 3, 6, 12, and 18 months after the operation. In addition, anti-osteoporosis treatment with calcium, calcitriol, and calcitonin was suggested.
Therapeutic evaluation
A VAS was applied to evaluate participants before and after the operation and at the follow-up. Daily activities and dysfunction before and after the operation were evaluated by the Oswestry Disability Index (ODI). Bone cement leakage and recovery of spinal canal encroachment were monitored by CT.
Statistical analysis
Statistical analysis was carried out using the statistical software SPSS 17.0 (IBM Corp., Armonk, NY, USA). The parameters were expressed as mean ± standard deviation. Continuous variables were analyzed for differences using Student’s t-test. A P value <0.05 indicated a significant difference.
Results
All operations were accomplished successfully. The average operation time was 122.5 min (90–200 min). The average estimated blood loss was 287.8 mL (110–550 mL). The average amount of cement augmentation was 4 mL (3–5 mL).
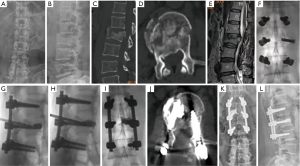
All participants were followed-up for an average of 18 months (12–36 months) and reported considerable lumbar pain relief after the operation. The participants with incomplete neurologic deficit were completely recovered following surgery. No screw loosening or recollapse of the injured vertebra were observed. A solitary participant suffered an adjacent vertebral fracture 3 years after the operation, and was healed after a second kyphoplasty. The CT scan showed that 2 participants had bone cement leakage into the paravertebral tissues, but no clinical symptoms were observed. The X-rays and CTs of 1 participant treated by balloon kyphoplasty with posterior pedicle screw fixation are shown in Figure 3.
We found the preoperative Cobb angle decreased from 23.2°±3.6° before the operation to 5.3°±2° after the operation and to 5.7°±2.2° at the last follow up (P<0.05). The VBHL improved from 56.8%±7.8% before the operation to 9.1%±1.6% after the operation and to 9.7%±1.9% at the last follow up (P<0.05). The average VAS score before the operation was 8.8±0.9 and improved to 2.5±0.4 after the operation and to 1.4±0.4 at the final follow up (P<0.05). The ODI score decreased from an average of 88.6%±3.5% before the operation to 32.3%±3.7% after the operation and to 17.5%±1.8% at the last follow up (P<0.05). Detailed dataare displayed in Table 2.
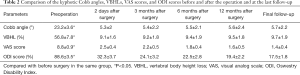
Full table
Discussion
This study demonstrated that osteoporotic TLBFs in elderly patients with neurologic deficits can be effectively treated by balloon kyphoplasty combined with posterior pedicle screw fixation through a single incision. Fracture reduction and fixation were achieved using pedicle screws in fractured vertebra, and adjacent upper and lower vertebra. Reconstruction of the anterior column was performed by balloon-assisted expansion and was followed by an injection of PMMA cement. Maintenance of the vertebral middle column height and Cobb angle was observed in all participants, and no screw breakage and secondary deformity were found.
At present, the common surgical methods for thoracolumbar burst fractures include short segment posterior fixation (SSPF), short segment posterior fixation with intermediate screws at fractured level (SSPFI), long segment posterior fixation (LSPF) and combined with bone cement. However, there is no unified conclusion about which internal fixation method can obtain better fixation effect. Because of suspension effect and quadrilateral effect, simple SSPF may lead to loss of correction and loosening or fracture of internal fixation (18,19). Although LSPF can obtain a more reliable fixation, it is not conducive to the postoperative recovery in the elderly due to its longer operation time and larger trauma. To avoid the above complications, SSPFI has been widely used in clinic in recent years. Biomechanical studies have verified that SSPFI can reduce screw stress, increase axial bearing capacity, anti-flexion ability, anti-rotation ability of internal fixation, and improve the stability of the spine when compared to SSPF (20,21). In this study, combined with balloon kyphoplasty, the immediate stability of the fixed segment after operation can be further improved without increasing the fixed segment.
Pedicle screw fixation with balloon kyphoplasty was developed after the emergence of transpedicular fixation, inflatable balloons, injectable PMMA, and other bone substitutes. Compared with single posterior short-segment pedicle screw fixation, kyphoplasty could offer additional support to the anterior column, thus improving fixation stability. Mermelstein et al. (22) investigated the biomechanical stability of TLBFs reinforced by calcium phosphate cement (CPC) in a cadaveric study and showed the transpedicular vertebral body reconstruction with hydroxyapatite cement could significantly reduce the incidence of pedicle screw bending by 59% in flexion and 38% in extension. Mean initial stiffness in the flexion-extension plane was increased by 40%. Verlaan et al. (23) performed balloon kyphoplasty after posterior short-segment reduction and fixation to treat traumatic burst fractures and showed that the technique was practical and effective. The postoperative radiographs and MRIs demonstrated a good fracture reduction and filling of the bone defect without unwarranted bone displacement. Similar results were also reported by Fuentes et al. (12,24,25).
Despite successful applications, kyphoplasty with PMMA combined with posterior fixation has been seldom reported as treatment for osteoporotic TLBFs. In this study, we performed the procedure in patients with osteoporosis, and found the results were promising. In this series, the Cobb angle changed from 23.2°±3.6° before surgery to 5.3°±2° immediately after surgery. The VBHL changed from 56.8%±7.8% to 9.1%±1.6% after surgery. Notably, loss of correction slightly occurred during following-up, which could mainly be contributed to 3 factors: reconstruction of the anterior column by kyphoplasty, use of pedicle screws, and posterolateral fusion. Pedicle screws could provide a 3-point fixation of the fractured segment, and significantly increase the stiffness of pedicle screw fixation. Anekstein et al. (16) compared the biomechanical stability of 4- and 6-screw constructs for unstable lumbar spine fractures and found that the addition of intermediate screws at the level of a burst fracture significantly increases the stiffness of a short segment pedicular fixation. Posterolateral fusion combined with pedicle screw fixation could provide better anterior and posterior support, lumbar lordosis, normal sagittal contour, and spinal biomechanics than fusion without screws (26).
In this study, the average duration of the operation was 122.5 min (90–200 min), and the average blood loss was 287.8 mL (110–550 mL). The average VAS score dropped significantly from 8.8±0.9 before the operation to 2.5±0.4 after operation and to 1.4±0.4 at the final follow up. The ODI score dropped from an average 88.6%±3.5% before operation to 32.3%±3.7% after operation and to 17.5%±1.8% at the last follow up. No implant failures were observed in this series. Our results are similar to the reports by Korovessis et al. (9), but are better than the results by Afzal et al. (20), which indicated that the mean operation times were 75 min with a blood loss of 350 mL and 142 min with an average 720 mL blood loss, respectively. All of these studies indicated that balloon kyphoplasty combined with posterior pedicle screw fixation was a preferable choice for osteoporotic TLBFs.
In the present study, PMMA rather than CPC was used to reconstruct the anterior column. A biomechanical study demonstrated that PMMA displayed similar behavior to CPC in human osteoporotic lumbar vertebra after prophylactic kyphoplasty (27). However, some studies have indicated that CPC is not an ideal bone substitute and has drawbacks including short freezing time, poor injectability, and early absorption (28-30). Piazzolla et al. (28) presented a case of vertebral body recollapse after kyphoplasty with CPC in a patient with L1 compression fracture. Ryu et al. (29) observed that the fractured vertebra was effectively reduced during the early postoperative time, but the recurrent progression of height loss was observed during the follow-up period because of the absorption of CPC. Due to the circumstance that all participants in this group were elderly (aged more than 60 years old), the PMMA that filled in the trabecular space could increase both the strength of screws and resistance to pullout in osteoporotic vertebra (31).
Restoration of the vertebral morphology and decompression of spinal canal are essential goals of surgical intervention for osteoporotic TLBFs. However, performing open reduction under direct visualization is unreasonable and unnecessary for all fractures. In this study, fracture reduction and canal encroachment were indirectly improved by the combination of posterior ligament distraction and the support from pedicle screws and rods. Most fractures recovered automatically after temporary instrumentation was placed on one side of the injured vertebra. Previous clinical studies have demonstrated that small fragments of bone will be absorbed and that narrow vertebra will recover spontaneously over time (32,33). Thus, the small fracture fragments occupying the spinal canal could be left in situ without special maneuvers.
The key points of balloon kyphoplasty augmentation are how to inject PMMA into the target vertebra and avoid cement leakage. In this study, the procedure was performed in 2 steps. Firstly, we inflated the vertebra with a balloon, restored the vertebral height, and compressed the surrounding cancellous bone to form a relatively closed cavity in the vertebra. Second, approximately 3 mL PMMA was injected under continuous fluoroscopy with low pressure to fill in bone defects. The optimal puncture target is at 1/3 anterior segment of the vertebra. During bone cement filling, cement diffusion at the anterior and middle columns of the injured vertebra needs to be ensured. When the bone cement diffuses over 1/4 of the posterior vertebra, the injection should be carefully monitored. The ideal diffusion condition is that the bone cement nears the upper and lower endplates in the lateral view, and is located bilaterally along the midline of the vertebra in the AP view. According to the spine 3-column theory, the anterior column bears 75–80% of the axial force (34), indicating that cement diffused over the anterior 2/3 of vertebra is sufficient for providing mechanical support. The injection should be stopped immediately when the bone cement is diffused evenly or leaks into the extraosseous space. Then, a pedicle screw was inserted along the cement channel to ensure that the pedicle screw could form a solid entity with the vertebra after the bone cement solidified. In this study, no looseness and breakage of the pedicle screws was observed, indicating that the procedure was safe and stable.
In this study, all participants were elderly and unwilling and intolerant to a secondary operation. However, implant removal is occasionally necessary for young patients. Technically, pedicle screw removal after bone cement reinforcement is feasible. Pare et al. (35) studied the biomechanical characters of standard and fenestrated pedicle screws augmented with PMMA in the osteoporotic spine, and found that the success rate of screw removal was 88%. The authors believed that screw loosening occurs earlier at the bone-cement interface than the screw-cement interfaces. Martín et al. (36) also reported the removal of PMMA augmentation screws and reoperations were not as complicated as expected. After screw removal, the use of new screws with 1 mm larger diameter could provide better fixation. In this study, no complications caused by retaining the implants have yet to be observed, but long-term effects should still be followed.
The occurrence of adjacent vertebral fracture is another common complication of vertebral body augmentation with cement. The literature on balloon kyphoplasty reports a subsequent fracture rate of 12–52% (37,38). In this study, 1 participant suffered an adjacent vertebral fracture, which was healed after a second kyphoplasty. The low incidence might be related to the small sample size and short follow-up period or to the standard anti-osteoporosis therapy and scientific rehabilitation processes. We provide the following suggestions based on our clinical observations and experiences. First, osteoporosis is the main cause of TLCF and TLBF, so long-term anti-osteoporosis treatment is necessary. We suggest that anti-osteoporosis therapy should be continued for at least half a year. Second, appropriate rehabilitation should be performed under the protection of a brace. All participants were recommended to wear a brace for 3 months after the operation and to avoid unnecessary activities. Third, surgeons must be well-experienced with spine surgery, and carefully controlled during the procedure.
Conclusions
Balloon kyphoplasty combined with posterior pedicle screw fixation was shown to be an effective treatment for osteoporotic TLBFs. This procedure has advantages such as single approach, reconstruction of 3 spinal columns, less blood loss, short operation time, and rapid recovery. However, due to the small number of participants and short follow-up period, long term follow-up and studies of larger sample size are needed to determine the value of the proposed method.
Acknowledgments
We are grateful to Professor Lianbo Xiao, Director of Shanghai Guanghua Hospital, and Professor Jiong Mei from the Department of Orthopedics, Shanghai Sixth People’s Hospital Affiliated with the Shanghai Jiao Tong University for their help and advice.
Funding: This study was supported by the general project of Shanghai Municipal Health Bureau (201840361), key project of Changning Science & Technology Association (CNKW 2017Z05), and project of Novel Interdisciplinary of Health System in Pudong New Area, Shanghai (PWXx2020-08).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-665
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-665
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-665). Dr. Ni reports that he received funding of Project of Novel Interdisciplinary of Health System in Pudong New Area, Shanghai (PWXx2020-08) during the past 36 months. Dr. Jia reports that he received funding of the general project of Shanghai Municipal Health Bureau (201840361) and key project of Changning Science & Technology Association (CNKW 2017Z05). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted according to the Helsinki Declaration (as revised in 2013) (Ethical Principles for Medical Research Involving Human Subjects) and was approved by the ethics committee of Guanghua Hospital, Shanghai University of Traditional Chinese Medicine (No.: 2019-k-14). All patients provided their written informed consent for the publication of their identifying photographs.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holdsworth F. Fractures, dislocations, and fracture-dislocations of the spine. J Bone Joint Surg Am 1970;52:1534-51. [Crossref] [PubMed]
- Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983;8:817-31. [Crossref] [PubMed]
- Wang P, Hu X. Biomechanical finite element analysis of superior endplate collapse after thoracolumbar fracture surgery. Ann Transl Med 2020;8:753. [Crossref] [PubMed]
- Ismail AA, Cooper C, Felsenberg D, et al. Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. Osteoporos Int 1999;9:206-13. [Crossref] [PubMed]
- Shin JJ, Chin DK, Yoon YS. Percutaneous vertebroplasty for the treatment of osteoporotic burst fractures. Acta Neurochir 2009;151:141-8. [Crossref] [PubMed]
- McLain RF, Sparling E, Benson DR. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 1993;75:162-7. [Crossref] [PubMed]
- Dai LY, Jiang LS, Jiang SD. Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures: a five to seven-year prospective randomized study. J Bone Joint Surg Am 2009;91:1033-41. [Crossref] [PubMed]
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976) 1994;19:1741-4. [Crossref] [PubMed]
- Korovessis P, Baikousis A, Zacharatos S, et al. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2–L4) burst fractures. Spine (Phila Pa 1976) 2006;31:859-68. [Crossref] [PubMed]
- Taylor RS, Taylor RJ, Fritzell P. Balloon kyphoplasty and vertebroplasty for vertebral compression fractures: a comparative systematic review of efficacy and safety. Spine (Phila Pa 1976) 2006;31:2747-55. [Crossref] [PubMed]
- Cho DY, Lee WY, Sheu PC. Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery 2003;53:1354-60. [Crossref] [PubMed]
- Fuentes S, Blondel B, Metellus P, et al. Percutaneous kyphoplasty and pedicle screw fixation for the management of thoraco-lumbar burst fractures. Eur Spine J 2010;19:1281-7. [Crossref] [PubMed]
- Aydogan M, Ozturk C, Karatoprak O, et al. The pedicle screw fixation with vertebroplasty augmentation in the surgical treatment of the severe osteoporotic spines. J Spinal Disord Tech 2009;22:444-7. [Crossref] [PubMed]
- Kanna RM, Shetty AP, Rajasekaran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J 2015;15:256-64. [Crossref] [PubMed]
- Dick JC, Jones MP, Zdeblick TA, et al. A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord 1994;7:402-7. [Crossref] [PubMed]
- Anekstein Y, Brosh T, Mirovsky Y. Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. J Spinal Disord Tech 2007;20:72-7. [Crossref] [PubMed]
- Vaccaro AR, Oner C, Kepler CK, et al. AO Spine Spinal Cord Injury & Trauma Knowledge Forum. AO Spine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37. [Crossref] [PubMed]
- Eno JJ, Chen L, Mitsunaga MM. Short same-segment fixation of thoracolumbar burst fractures. Hawaii J Med Public Health 2012;71:19-22. [PubMed]
- Tezeren G, Kuru I. Posterior fixation of thoracolumbar burst fracture short-segment pedicle fixation versus long-segment instrumentation. J Spinal disord Tech 2005;18:485-8. [Crossref] [PubMed]
- Li C, Zhou Y, Wang H, et al. Treatment of unstable thoracolumbar fractures through short segment pedicle screw fixation techniques using pedicle fixation at the level of the fracture: a finite element analysis. PLoS ONE 2014;9:e99156 [Crossref] [PubMed]
- Mahar A, Kim C, Wedemeyer M, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine 2007;32:1503-7. [Crossref] [PubMed]
- Mermelstein LE, McLain RF, Yerby SA. Reinforcement of thoracolumbar burst fractures with calcium phosphate cement: a biomechanical study. Spine (Phila Pa 1976) 1998;23:664-70. [Crossref] [PubMed]
- Verlaan JJ, Dhert W JA, Verbout AJ, et al. Balloon vertebroplasty in combination with pedicle screw instrumentation: a novel technique to treat thoracic and lumbar burst fractures. Spine (Phila Pa 1976) 2005;30:E73-9. [Crossref] [PubMed]
- Afzal S, Akbar S, Dhar SA. Short segment pedicle screw instrumentation and augmentation vertebroplasty in lumbar burst fractures: an experience. Eur Spine J 2008;17:336-41. [Crossref] [PubMed]
- Van Herck B, Leirs G, Van Loon J. Transpedicular bone grafting as a supplement to posterior pedicle screw instrumentation in thoracolumbar burst fractures. Acta Orthop Belg 2009;75:815-21. [PubMed]
- Madan S, Boeree NR. Outcome of posterior lumbar interbody fusion versus posterolateral fusion for spondylolytic spondylolisthesis. Spine (Phila Pa 1976) 2002;27:1536-42. [Crossref] [PubMed]
- Tomita S, Kin A, Yazu M, et al. Biomechanical evaluation of kyphoplasty and vertebroplasty with calcium phosphate cement in a simulated osteoporotic compression fracture. J Orthop Sci 2003;8:192-7. [Crossref] [PubMed]
- Piazzolla A, De Giorgi G, Solarino G. Vertebral body recollapse without trauma after kyphoplasty with calcium phosphate cement. Musculoskelet Surg 2011;95:141-5. [Crossref] [PubMed]
- Ryu KS, Shim JH, Heo HY, et al. Therapeutic efficacy of injectable calcium phosphate cement in osteoporotic vertebral compression fractures: prospective nonrandomized controlled study at 6-month follow-up. World Neurosurg 2010;73:408-11. [Crossref] [PubMed]
- Chen C, Lv G, Xu B, et al. Posterior short-segment instrumentation and limited segmental decompression supplemented with vertebroplasty with calcium sulphate and intermediate screws for thoracolumbar burst fractures. Eur Spine J 2014;23:1548-57. [Crossref] [PubMed]
- Cook SD, Salkeld SL, Stanley T, et al. Biomechanical study of pedicle screw fixation in severely osteoporotic bone. Spine J 2004;4:402-8. [Crossref] [PubMed]
- Dai LY, Wang XY, Jiang L S. Evaluation of traumatic spinal canal stenosis in thoracolumbar burst fractures: a comparison of three methods for measuring the percent canal occlusion. Eur J Radiol 2008;67:526-30. [Crossref] [PubMed]
- Mueller LA, Degreif J, Schmidt R, et al. Ultrasound-guided spinal fracture repositioning, ligamentotaxis, and remodeling after thoracolumbar burst fractures. Spine (Phila Pa 1976) 2006;31:E739-46. [Crossref] [PubMed]
- Goel VK, Kong W, Han JS, et al. A combined finite element and optimization investigation of lumbar spine mechanics with and without muscles. Spine (Phila Pa 1976) 1993;18:1531-41. [Crossref] [PubMed]
- Paré PE, Chappuis JL, Rampersaud R, et al. Biomechanical evaluation of a novel fenestrated pedicle screw augmented with bone cement in osteoporotic spines. Spine (Phila Pa 1976) 2011;36:E1210-4. [Crossref] [PubMed]
- Martín-Fernández M, López-Herrradón A, Piñera A R, et al. Potential risks of using cement-augmented screws for spinal fusion in patients with low bone quality. Spine J 2017;17:1192-9. [Crossref] [PubMed]
- Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 2004;25:175-180. [PubMed]
- Fribourg D, Tang C, Sra P, et al. Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976) 2004;29:2270-2276. [Crossref] [PubMed]


