Early integration of palliative care into oncology: evidence, challenges and barriers
Introduction
In the past three decades, improvements in prevention, early detection and treatment of cancer have dramatically changed cancer outcomes. The American Cancer Society estimated about 1.6 million new cancer cases and 58 thousand cancer deaths in the United States in 2015 (1). Those cancer patients and their families are experiencing tremendous physical and psychosocial issues during cancer treatment that have a huge negative impact on quality of life, the cost of care, and even survival (2). By WHO definition, palliative care is “an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” (3). Palliative care is an essential component in cancer care and has been recognized by professional societies and healthcare providers. The American Society of Clinical Oncology (ASCO) strongly recommends involvement of palliative care early during oncology care given the robust evidence of improvement in quality of life, better symptom control; reduced caregiver burden; and possible survival benefit (2,4,5).
Cancer patients can benefit from palliative care, regardless of their disease prognosis and stage (6). Palliative care used to be introduced to patients at a late stage of the cancer spectrum, and was mistakenly thought as end of life care and lumped together with hospice. In the past decade, palliative care has been among the top ten fast growing subspecialties in medicine, largely due to increasing needs (7). Traditionally, palliative care was incorporated in the late stage of cancer treatment, frequently as an inpatient consultation with a goal of care discussion, transition to hospice, and imminent death. In a 2009 study, lung cancer patients had high hospital mortality, high ICU mortality and were frequently discharged to hospice with just days to live. Only 8% of the patients with lung cancer at a cancer center received palliative care consultation, most to address end of life care during their last hospital stay (8). The experience of inpatient palliative care consultation in hematological malignancy patients at Johns Hopkins Hospital demonstrated a similar late referral pattern, just 6 to 9 days before death. Their special needs such as transfusions should be considered during their palliative care and hospice care enrollment (9). Only 5% of metastatic head and neck cancer patients ever received a palliative care consultation, which was disproportionally restricted to elderly, uninsured and patients with higher risks of mortality (10).
In the past decade, many researchers have focused on how to integrate palliative care with oncology care and have found consistent and compelling evidence to support an early incorporation model in recent multiple randomized clinical trials (11,12). In this review, we will summarize the current available evidence of models of palliative care in oncology patients and their advantages and limitations. We will discuss challenges and barriers during integration of palliative care to oncology care, and opportunities to overcome those difficulties.
What is the best model to integrate palliative care with cancer care?
Inpatient palliative care model
Hospital-based palliative care programs were developed to address the needs of patients with advanced illness for adequate pain and symptoms control, discussion of life sustaining treatment, and hospice referral (10,13-15). Gade et al. (13) conducted a multicenter randomized clinical trial to investigate the impact of an interdisciplinary inpatient palliative team (IDPCT) care service on patient satisfaction, clinical outcomes and subsequent health cost (Table 1). A total of 517 patients were randomized; 280 received the intervention and 237 received usual care; one third had cancer. On the intervention arm, there was a significant increase of advance directives at discharge (P<0.001), less death during the hospitalization and less total hospitalization cost ($6,766). However, there was no difference in overall survival (OS) or quality of life (QOL) on scales that included symptoms, emotional and spiritual support and quality of life. This study illustrated that inpatient palliative care provides a positive impact on goals of care and reduction of hospitalization cost but no improvement of patient QOL. It raised questions about whether inpatient PC is sufficient for symptom control when introduced in very late stages of disease.

Full table
Home based palliative care model
Brumley et al. investigated the in-home palliative care model by a large randomized controlled clinical trial to determine whether IDPCT can improve patient satisfaction and give better symptom control (16) (Table 1). In this study, a total of 298 patients with prognosis less than one year and recent hospital or emergency department (ED) visit were enrolled, including 138 patients with cancer. A total of 155 patients randomized into the intervention arm, which includes in-home multidisciplinary palliative care, and 155 patients in the usual care arm. The results showed lower rates of ED visits (P=0.01), hospital admissions (P<0.001), and lower medical cost of $7,500 (P=0.004), with patients more likely to die at home (P<0.001). There was no difference in hospice enrollment. This trial demonstrated a greater improvement of patient satisfaction and reduction of hospitalization stay and cost of care. The biggest limitation of this study is that the study did not measure quality of life, symptom control or survival.
Subsequent to these randomized studies showing equal survival, better satisfaction and lower costs, Kaiser Permanente adopted the IDPCT model nationwide (16,22-24).
Outpatient clinic palliative care model
The Educate, Nurture, Advise, Before Life Ends (ENABLE) II study was the first RCT focused on cancer patient palliative care during their cancer treatment in the clinic setting (17) (Table 1). The intervention was a nurse conducted education program with 322 patients randomized into the intervention arm (n=161) or usual care arm (n=161) and followed till death or study completion. The study included 41% with gastrointestinal tract malignancy, 35% lung cancer, 12% genitourinary cancer and 10% breast cancer. Patients in the intervention arm received at least monthly office follow up visits and structured telephone encounters. This trial demonstrated that concurrent palliative care along with anti-cancer treatment significantly improved quality of life (P=0.02) with less depressed mood (P=0.02). The intervention arm had decreased symptom burden and a median survival of 14 months as compared with usual care arm of 8.5 months (P=0.14), with a hazard ratio for death at 12 months of 0.7. Costs were not increased.
Based on The ENABLE II result, the ENABLE phase III RCT was implemented to identify the best time to initiate palliative care after cancer diagnosis. The result was recently published with strong evidence to support the survival benefits of the early integration palliative care into oncology care (18). Participants were randomized into an immediate or delayed entry group at a time point of 3 months after diagnosis of cancer. Compared to the delayed group, the early group had a risk of death hazard ratio of 0.72 at 1 year (P=0.003), with median survival of 18.3 months, and 11.8 months for delayed entry group. Kaplan-Meier 1-year survival rates were 63% in the early group and 15% higher than the delayed group (P=0.038). However, there wass no statistically significant difference among patient-reported outcomes and resources uses (18). Both ENABLE trials are consistent with the palliative care mantra “Better care at a cost we can afford”.
Early palliative care upon diagnosis in patients with metastatic non-small-cell lung cancer (mNSCLC)
The effect of early use of palliative care along with regular oncology care was studied in a RCT of new patients diagnosed with mNSCLC (19). Patients with mNSCLC have substantial symptoms burdens and aggressive cancer directed therapy, often even at the end of life (8,25,26). This study was a 1:1 randomization of 151 patients upon their diagnosis of mNSCLC (Table 1). Twenty-seven patients died at 12 weeks into study and 107 patients completed the whole assessments. All patients received standard oncology care. Seventy-seven patients were randomized to monthly outpatient palliative care, and palliative care consultation if the person was hospitalized, along with usual oncology care. Seventy-four patients received standard oncology care only. At 12 weeks, the early palliative care intervention group had better quality of life (P=0.03), less depression and anxiety and a better mood (P=0.01). Fewer patients in the early palliative care group received aggressive oncology care near the end of life (P=0.05). The patients in the palliative care group understood their prognosis better, were able to state that they had incurable illness more correctly, got less 4th and 5th line chemotherapy, and used hospice over twice as many days (25). The median survival of this group was longer (11.6 vs. 8.9 months, P=0.02). Costs were also reduced. There were substantial differences in what the oncologists and palliative care team documented, with much more emphasis on coping in the palliative care notes, suggesting that oncologists will need additional skills if they are going to do the palliative care role, too (25,27). This was the first study that demonstrated early palliative care intervention provides a survival benefit in cancer patients, as well as a reduction in symptom burden and depression.
Early palliative care for patient with advance cancer: a cluster-randomized controlled trial
Zimmermann et al. from Canada carried out a uniquely designed study as a clustered randomized controlled trial to assess early palliative care intervention effects in advanced cancer patients (20). Palliative care interventions in this study included outpatient clinic, inpatient, and home settings (Table 1). The clinic randomization was for clinics in the same cancer center, e.g., Tuesday a.m. lung cancer clinic versus Thursday clinic, not geographic sites. The tumor types including lung, gastrointestinal, genitourinary, breast and gynecological malignancies. Quality of life, severity of symptoms, and satisfaction with care were measured at baseline and every 4 months during this study. A total of 461 patients enrolled in the study, 228 intervention and 233 controls; 393 patients completed at least one follow up assessment. Quality of life was assessed by both the Functional Assessment of Chronic Illness therapy-Spiritual Well-being (FACIT-sp) scale and Quality of Life at the End of Life (QUAL-E) scale. At 3 months, there was significant improvement of quality of life by QUAL-E scale (P=0.05), but less difference in FACIT-sp scale (P=0.07), and significantly better satisfaction with care (P=0.0003). At 4 months, there were significant differences in all outcome measures favoring the intervention group. This study demonstrated again that early palliative care interventions provide benefit in quality of life, symptom relief, and satisfaction with care. This study did not show any difference of outcome in clinic settings or tumor sites. At least half of these Canadian oncologists had formal PC training, suggesting that the presence of an IDPCT—concentrated on PC—works better than the oncologist trying to do PC herself (28).
Ferrell et al. did a pre/post comparison of all lung cancer patients treated at the City of Hope after the requirement for concurrent palliative care. They showed significantly improved symptom scores and quality of life, less depression and anxiety, and improved survival with an intervention that was just four visits with the advance practice nurse (Ferrell et al. in press). Significant benefits were found for caregivers, too, with better quality of life, well being, and less distress (29). This illustrates again how simple, structured expert PC interventions make a large difference.
Randomized studies of PC in other diseases add to the evidence for palliative care referral and how long the effect is maintained for patients with multiple sclerosis
Higginson et al. (21,30) did a phase II trial of palliative care immediately, compared to delayed palliative care after 12 weeks in patients severely affected with multiple sclerosis. A total of 52 patients were recruited to this study. The MS patients benefited from immediate palliative care intervention by improvement of all the five most important symptom scale and markedly decreased caregiver burden, with lower costs (1,789 £GB over 12 weeks) to the National Health Service. After withdrawal of palliative care at 6 weeks, those effects were maintained at 12 weeks but not at 24 weeks. A large randomized phase III trial will demonstrate that PC intervention has both immediate and long-term benefits, including an OS benefit and lower costs. (Personal communication, Irene Higginson MD OBE).
A randomized trial of PC for 232 patients hospitalized for acute heart failure, comparing usual care to usual care plus a single PC consultation, showed similar benefits. The quality of life scores increased at 1 month (difference +4.92, P<0.001), symptoms were less at 1 month (+3.69, P<0.001), including significant reductions in pain, tiredness, depression, anxiety, and appetite. Advance care planning was also nearly tripled—from a single consultation. The trial was stopped because the cardiologists wanted PC consultation to become standard care (14).
To date, there is not a single study that shows survival is decreased with a palliative care intervention, laying to rest fears about a “death squad”. At least two other studies have shown a survival benefit to symptom management and palliative care in addition to usual care. Smith and colleagues randomized 202 patients with severe refractory cancer pain to best medical management by a trained expert team to the same care plus an intrathecal drug delivery system (IDDS) (31). The IDDS group had significantly better pain control, fewer drug toxicities, and lived 102 days longer (P value 0.06; one living patient disenrolled from the trial and was censored, and with her counted the P value was <0.05) (31,32).
Higginson and colleagues randomized 105 patients with severe breathlessness to usual pulmonologist care versus usual care plus an IDPCT integrating palliative care, respiratory medicine, physiotherapy, and occupational therapy. The main endpoint was mastery of breathlessness at 6 weeks, which was achieved. Survival was increased by an average of 6 months in the intervention group, with 94% versus 75% alive at the end of the study, P=0.048 (33). Other randomized IDPCT interventions in heart failure have shown substantial improvements in quality of life but the hazard ratio for death at 6 months was not significantly better or worse (14).
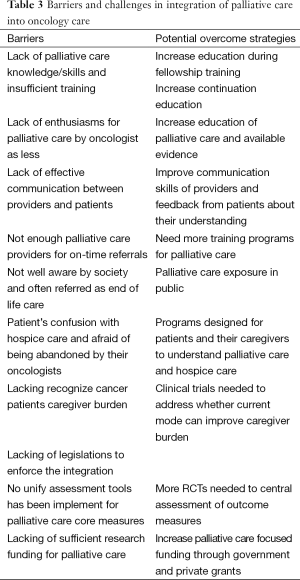
Barriers and challenges in integration of palliative care into oncology care and potential strategies to overcome
Multiple RCTs have shown convincing evidence of benefit by early palliative care alongside standard oncology care. Moreover, multiple different models of integration of both have been investigated including outpatient clinic, inpatient consultations and home palliative care and all have worked. The best model has not been established yet but from the mNSLCS and Enable III trial data, there is clear evidence supporting early intervention rather than later, upon the diagnosis of malignancy.
How should those data translate into oncologists’ daily practice? There are multiple layers of barriers and obstacles for oncologists to fully utilize palliative care. More research in this field is needed to identify those barriers and solutions for those challenges.
Oncologist perspectives
From the oncologist’s perspective, lack of awareness or knowledge is one main reason why PC is not used more (34). Emphasis on more training in palliative care during oncology fellowship curriculum can be an effective way, and increasing continued medical education on this topic is also very important for updated knowledge of palliative care (35-37). There can be less enthusiasm about palliative care due to the fear of losing patients from oncology practice, but in our experience this is unwarranted as most oncologists are already too busy (38,39). Oncologists may be concerned about the time that PC takes; in all the randomized trials, the PC intervention took at least an extra hour a month, with availability to answer phone calls and do education.
Oncologists play a vital role in the process of integration as they often manage pain and symptoms before referral to palliative care (40). We all often manage patient symptoms as best we can, till the time point that we feel not able to handle them on our own. However, not all oncologists have easy access to a palliative care team and have to deal those issues regardless whether we are comfortable or not (41). Basic palliative care skills are important for oncologists to address patients’ symptoms early before the formal referral (40,41) (Table 2).

Full table
Effective communication is an essential component of integration (46,47). The first encounter with the oncologist usually is focused on discussion of disease overall prognosis, treatment options and their adverse effects, and less time spent on palliative care. The goal of care is often discussed in the first visit but there is significant mis-understanding of disease prognosis and goal of care, even when the oncologist’s skill was rated good by their patients (48). Rather than a one-time point focus on this topic, goals of care should be addressed throughout the entire cancer treatment, especially at times of treatment and prognosis change (49). Patient’s reciprocal comments on their understanding of disease could help to identify gaps and bridge them with focused conversations (50), such as the oncologist asking “Now that we have discussed your prognosis and goals, what is your understanding of your situation?”.
Can primary care physicians (PCP) play a role in this process? PCPs have a long-term relationship with the patient and may have already known about the patient’s view of serious illness and end of life plans before the cancer diagnosis. At the same time, the patient is facing the same physician they have trust and even more like an old friend to talk about their concerns. It could be easier and less stressful for both providers and patients. Recently there was a discussion on New England Journal of Medicine on the topic of who should be responsible for advance directive discussion with patient: the medical oncologist (who has not broached the subject during six types of chemotherapy), the PCP, or the palliative care team (51). It would be interesting to know the opinions from the physicians’ perspective; importantly, it should be also included from patients’ view. Ultimately, this may provide some new angles to introduce palliative care early and smoothly. This is not meant to replace the responsibility of oncologists and PC providers; rather, we see it as similar to referral to a cardiologist for the management of trastuzumab-induced heart failure.
Resource barriers
Palliative care resources available to oncologists can be limited, but are increasing rapidly and nearly every community has available palliative care, accessed at www.getpalliativecare.org (52). The perceived shortage of qualified palliative care providers in home based, clinic and hospital settings is often just that—the oncologist has not reached out to available sources. Palliative care is one of fastest grow subspecialties in medicine in past decade but still not able to catch up increasing demands (53). We have an urgent need for palliative care providers including physicians, nurse practitioners, and social workers, and for oncologists to practice primary palliative care (54).
Public exposure
How society views palliative care is another factor in prompt integration of palliative care into oncology care. Cancer patients and their families, caregivers and society do not understand what exactly palliative care is. Often PC was understood as hospice care and interpreted as a “death sentence”, when in fact both hospice and PC are associated with better survival as well as better symptom management (26,55,56). In the past, when the oncologist mentioned palliative care, it raised concerns such as “no further treatment can be given”. Improving the general population understanding of the difference between PC and hospice care is critical for better integration of palliative care to oncology care (12).
Recent studies show that in the general population there is a high percentage of acceptance rate of palliative care, but in our own experience in the oncology clinic there is hesitancy and reluctance when patients and families hear about palliative care (57). Not surprisingly, decisions about loved ones or ourselves are a lot more difficult than general information. So, promoting general awareness of palliative care in society will be fundamental for integration of palliative care to oncology—especially the message about better quality of life AND longer survival—as will the direct referral from the oncologist.
Health care policy
Health care is undergoing major transformations. Integration of palliative care with oncology can provide a cost effective model as shown in multiple clinical trials. Most importantly, this model can improve patient satisfaction and reduce unnecessary studies and treatments which are not life prolonging nor improving quality of life. Incentives to improve coherence to palliative care guidelines and core structures are needed.
Furthermore, research funding in this era is significantly lacking, with palliative care only about 1% of overall NIH research funding (58). General health care police makers could recognize this discrepancy and increase funding support for palliative care and encourage more research on integration with other specialties like oncology. One ideal solution would be for both oncology and palliative care specialists to collaborate together to answer those questions and problems, and to focus on patient satisfactions, excellent communication and lower cost (Table 3).
Full table
Future directions and conclusions
Plenty of evidence has shown early palliative care can improve cancer care and overall outcomes in term of pain management, symptoms control, psychological relieve, patient satisfaction and even survival. Different models of early integration, incorporation of PC in clinics, hospital and home settings have been studied and clearly showed benefit to offering palliative care upon the diagnosis of cancer. Yet, this model is still facing multiple barriers and challenges from providers, patients, caregivers and healthcare policy as we have discussed in previous session.
To overcome those barriers, acceptance of the multiple large randomized clinical trials are needed to promote communication, awareness of palliative care, and the utility of palliative care. This integration process involves a multi-disciplinary team including the PCP, oncologists, palliative care providers, nurses, social workers and healthcare policy makers. This integration of palliative care to oncology care provides the best possible care to cancer patients. Palliative care in oncology care follows the same concept Dr. Edward Trudeau mentioned in the 1800s: “To cure sometimes, to relieve often, to comfort always”.
Acknowledgements
Funding: This work was supported by the P30 CA 006973 SKCCC Cancer Center Grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [PubMed]
- Davis MP, Bruera E, Morganstern D. Early integration of palliative and supportive care in the cancer continuum: challenges and opportunities. Am Soc Clin Oncol Educ Book 2013;144-50. [PubMed]
- Available online: http://www.who.int/cancer/palliative/definition/en/
- Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol 2012;30:880-7. [PubMed]
- Smith TJ, Schnipper LJ. The American Society of Clinical Oncology program to improve end-of-life care. J Palliat Med 1998;1:221-30. [PubMed]
- Von Roenn JH. Optimal cancer care: Concurrent oncology and palliative care. J Natl Compr Canc Netw 2013;11 Suppl 1:S1-2. [PubMed]
- Strand JJ, Mansel JK, Swetz KM, et al. The growth of palliative care. Minn Med 2014;97:39-43. [PubMed]
- Reville B, Miller MN, Toner RW, et al. End-of-life care for hospitalized patients with lung cancer: utilization of a palliative care service. J Palliat Med 2010;13:1261-6. [PubMed]
- Sexauer A, Cheng MJ, Knight L, et al. Patterns of hospice use in patients dying from hematologic malignancies. J Palliat Med 2014;17:195-9. [PubMed]
- Mulvey CL, Smith TJ, Gourin CG. Use of inpatient palliative care services in patients with metastatic incurable head and neck cancer. Head Neck 2014. [Epub ahead of print]. [PubMed]
- Bauman JR, Temel JS. The integration of early palliative care with oncology care: the time has come for a new tradition. J Natl Compr Canc Netw 2014;12:1763-71; quiz 1771.
- Parikh RB, Kirch RA, Smith TJ, et al. Early specialty palliative care--translating data in oncology into practice. N Engl J Med 2013;369:2347-51. [PubMed]
- Gade G, Venohr I, Conner D, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med 2008;11:180-90. [PubMed]
- Sidebottom AC, Jorgenson A, Richards H, et al. Inpatient palliative care for patients with acute heart failure: outcomes from a randomized trial. J Palliat Med 2015;18:134-42. [PubMed]
- Pierce B, Dougherty E, Panzarella T, et al. Staff stress, work satisfaction, and death attitudes on an oncology palliative care unit, and on a medical and radiation oncology inpatient unit. J Palliat Care 2007;23:32-9. [PubMed]
- Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;55:993-1000. [PubMed]
- Bakitas M, Lyons KD, Hegel MT, et al. The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: baseline findings, methodological challenges, and solutions. Palliat Support Care 2009;7:75-86. [PubMed]
- Bakitas MA, Tosteson TD, Li Z, et al. Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J Clin Oncol 2015;33:1438-45. [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [PubMed]
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383:1721-30. [PubMed]
- Higginson IJ, Booth S. The randomized fast-track trial in palliative care: role, utility and ethics in the evaluation of interventions in palliative care? Palliat Med 2011;25:741-7. [PubMed]
- Jang RW, Burman D, Swami N, et al. Impact of an oncology palliative care clinic on access to home care services. Am J Hosp Palliat Care 2013;30:425-31. [PubMed]
- Lo C, Burman D, Rodin G, et al. Measuring patient satisfaction in oncology palliative care: psychometric properties of the FAMCARE-patient scale. Qual Life Res 2009;18:747-52. [PubMed]
- Porzio G, Aielli F, Verna L, et al. Integrating oncology and palliative home care in Italy: the experience of the “L’Aquila per la Vita” Home Care Unit. Tumori 2013;99:225-8. [PubMed]
- Roeland E, Loprinzi C, Moynihan TJ, et al. In chemotherapy for lung cancer, sometimes less is more. J Natl Compr Canc Netw 2013;11:232-5. [PubMed]
- Saito AM, Landrum MB, Neville BA, et al. Hospice care and survival among elderly patients with lung cancer. J Palliat Med 2011;14:929-39. [PubMed]
- Yoong J, Park ER, Greer JA, et al. Early palliative care in advanced lung cancer: a qualitative study. JAMA Intern Med 2013;173:283-90. [PubMed]
- Hannon B, Swami N, Pope A, et al. The oncology palliative care clinic at the Princess Margaret Cancer Centre: an early intervention model for patients with advanced cancer. Support Care Cancer 2015;23:1073-80. [PubMed]
- Sun V, Grant M, Koczywas M, et al. Effectiveness of an interdisciplinary palliative care intervention for family caregivers in lung cancer. Cancer 2015. [Epub ahead of print]. [PubMed]
- Higginson IJ, Costantini M, Silber E, et al. Evaluation of a new model of short-term palliative care for people severely affected with multiple sclerosis: a randomised fast-track trial to test timing of referral and how long the effect is maintained. Postgrad Med J 2011;87:769-75. [PubMed]
- Smith TJ, Staats PS, Deer T, et al. Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol 2002;20:4040-9. [PubMed]
- Smith TJ, Coyne PJ, Staats PS, et al. An implantable drug delivery system (IDDS) for refractory cancer pain provides sustained pain control, less drug-related toxicity, and possibly better survival compared with comprehensive medical management (CMM). Ann Oncol 2005;16:825-33. [PubMed]
- Higginson IJ, Bausewein C, Reilly CC, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med 2014;2:979-87. [PubMed]
- Schenker Y, Crowley-Matoka M, Dohan D, et al. Oncologist factors that influence referrals to subspecialty palliative care clinics. J Oncol Pract 2014;10:e37-44. [PubMed]
- Roth M, Wang D, Kim M, et al. An assessment of the current state of palliative care education in pediatric hematology/oncology fellowship training. Pediatr Blood Cancer 2009;53:647-51. [PubMed]
- Ross DD, Shpritz D, Alexander CS, et al. Development of required postgraduate palliative care training for internal medicine residents and medical oncology fellows. J Cancer Educ 2004;19:81-7. [PubMed]
- Lefkowits C, Sukumvanich P, Claxton R, et al. Needs assessment of palliative care education in gynecologic oncology fellowship: we’re not teaching what we think is most important. Gynecol Oncol 2014;135:255-60. [PubMed]
- Head BA, Schapmire T, Hermann C, et al. The Interdisciplinary Curriculum for Oncology Palliative Care Education (iCOPE): meeting the challenge of interprofessional education. J Palliat Med 2014;17:1107-14. [PubMed]
- Mougalian SS, Lessen DS, Levine RL, et al. Palliative care training and associations with burnout in oncology fellows. J Support Oncol 2013;11:95-102. [PubMed]
- Rangachari D, Smith TJ. Integrating palliative care in oncology: the oncologist as a primary palliative care provider. Cancer J 2013;19:373-8. [PubMed]
- Reville B, Reifsnyder J, McGuire DB, et al. Education and referral criteria: impact on oncology referrals to palliative care. J Palliat Med 2013;16:786-9. [PubMed]
- Morris DA, Johnson KS, Ammarell N, et al. What is your understanding of your illness? A communication tool to explore patients’ perspectives of living with advanced illness. J Gen Intern Med 2012;27:1460-6. [PubMed]
- Dy SM, Asch SM, Lorenz KA, et al. Quality of end-of-life care for patients with advanced cancer in an academic medical center. J Palliat Med 2011;14:451-7. [PubMed]
- Taylor RM, Gustin JL, Wells-DiGregorio SM. Improving do-not-resuscitate discussions: a framework for physicians. J Support Oncol 2010;8:42-4. [PubMed]
- Quill TE, Abernethy AP. Generalist plus specialist palliative care--creating a more sustainable model. N Engl J Med 2013;368:1173-5. [PubMed]
- Johnson LA, Gorman C, Morse R, et al. Does communication skills training make a difference to patients’ experiences of consultations in oncology and palliative care services? Eur J Cancer Care (Engl) 2013;22:202-9. [PubMed]
- França JR, da Costa SF, Lopes ME, et al. The importance of communication in pediatric oncology palliative care: focus on Humanistic Nursing Theory. Rev Lat Am Enfermagem 2013;21:780-6. [PubMed]
- Granek L, Krzyzanowska MK, Tozer R, et al. Oncologists’ strategies and barriers to effective communication about the end of life. J Oncol Pract 2013;9:e129-35. [PubMed]
- van Vliet LM, Epstein AS. Current state of the art and science of patient-clinician communication in progressive disease: patients’ need to know and need to feel known. J Clin Oncol 2014;32:3474-8. [PubMed]
- Grainger MN, Hegarty S, Schofield P, et al. Discussing the transition to palliative care: evaluation of a brief communication skills training program for oncology clinicians. Palliat Support Care 2010;8:441-7. [PubMed]
- Tolle SW, Back AL, Meier DE. Clinical decisions. End-of-life advance directive. N Engl J Med 2015;372:667-70. [PubMed]
- Available online: http://www.getpalliativecare.org
- Smith AK, Thai JN, Bakitas MA, et al. The diverse landscape of palliative care clinics. J Palliat Med 2013;16:661-8. [PubMed]
- Schaefer KG, Chittenden EH, Sullivan AM, et al. Raising the bar for the care of seriously ill patients: results of a national survey to define essential palliative care competencies for medical students and residents. Acad Med 2014;89:1024-31. [PubMed]
- Connor SR, Pyenson B, Fitch K, et al. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manage 2007;33:238-46. [PubMed]
- Kelley AS, Deb P, Du Q, et al. Hospice enrollment saves money for Medicare and improves care quality across a number of different lengths-of-stay. Health Aff (Millwood) 2013;32:552-61. [PubMed]
- Munhoz BA, Paiva HS, Abdalla BM, et al. From one side to the other: what is essential? Perception of oncology patients and their caregivers in the beginning of oncology treatment and in palliative care. Einstein (Sao Paulo) 2014;12:485-91. [PubMed]
- Gelfman LP, Du Q, Morrison RS. An update: NIH research funding for palliative medicine 2006 to 2010. J Palliat Med 2013;16:125-9. [PubMed]


