
Cardiovascular medication and long-term outcome among intensive care unit survivors: a retrospective study
Introduction
In-hospital mortality has decreased among critically ill patients admitted to the intensive care unit (ICU) due to advances in critical care medicine and improvements in patient management (1-3). Accordingly, the number of ICU survivors has increased in recent years. Compared to the general population, these survivors have been reported to experience posttraumatic stress, depression, cognitive impairment, and physical weakness more frequently and to have poorer long-term survival outcomes (1,4). Therefore, ICU physicians must understand and improve the factors that affect the long-term outcomes of ICU survivors (5).
Cardiovascular medications, such as aspirin, beta-blockers, and statins, are used to treat or prevent cardiovascular disease. In the general population, these medications are frequently administered for long-term use in clinical practice (6). Considerable evidence indicates that the long-term use of cardiovascular medications may improve the outcome of critically ill patients. For example, a recent observational study reported that the use of angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARB) was associated with decreases in the incidence of sepsis and mortality among patients with chronic obstructive pulmonary disease (7). Another observational study reported an association between the use of calcium channel blockers prior to administration and improved outcomes in patients with sepsis (8,9). However, these observational studies focused mostly on patients with sepsis and did not address ICU survivors.
ICU survivors are reported to face a high risk of major adverse cardiovascular events after discharge (10). Therefore, the post-discharge use of cardiovascular medication may improve the long-term outcomes of these patients. However, data related to this topic remain scarce. Accordingly, the present study aimed to investigate the association between the prescription of cardiovascular medications at the time of ICU discharge and 1-year mortality in a sample of ICU survivors. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1786).
Methods
This retrospective observational study was conducted with approval from the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (SNUBH) (IRB approval number: B-1902/522-105). The requirement to obtain informed consent from each patient was waived by the IRB, given the retrospective observational study design and inclusion of medical records from patients who had completed treatment. The study also conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Data source and patient population
The present study obtained data from the electronic medical records stored in the Bundang Hospital Electronic System for Total Care (BESTCare) at SNUBH (11). Moreover, the dates of death of all patients, including those lost to follow-up, were collected from the Statistics Korea database (http://kostat.go.kr/portal/eng). The causes of death were classified according to the Korean standard classification of disease and cause of death (KCD) 7th edition, a publication of Statistics Korea.
The study population comprised ICU survivors, or members of the general ICU adult population aged ≥18 years who were admitted to the ICU between January 2012 and December 2016 and later discharged alive. As the study involved ICU survivors, the analysis included only the final ICU admission for patients admitted two or more times. Additionally, those with incomplete or missing medical records concerning regular cardiovascular medication at ICU discharge were excluded from the final analysis.
Main independent variable
We defined “cardiovascular medication of ICU survivor” as the cardiovascular medication prescribed to ICU survivors for continued use after ICU discharge. Data were collected on the following cardiovascular medications: calcium channel blockers, beta-blockers, ACE inhibitors, ARB, thiazide, furosemide, aspirin, clopidogrel, and statins. Patients who were prescribed any cardiovascular medication at ICU discharge were classified as the CV MED group, all other patients were classified as the non-CV MED group. In general, calcium channel blockers, beta-blockers, ACE inhibitors, ARBs, thiazides, and furosemide were prescribed with indication for hypertension, while aspirin, clopidogrel, and statins were prescribed to prevent primary or secondary adverse cardiovascular events among the adult population in South Korea. For example, aspirin, clopidogrel, or statins were prescribed not only for dyslipidemia patients but also for those who had risk factors for acute cardiovascular events, such as tobacco use, old age, lack of exercise, obesity, diabetes, and family history of heart disease.
Study outcomes
The primary outcome of the study was the association between 1-year mortality among ICU survivors after ICU discharge and CV medication, as determined by a comparison between the CV MED group and the non-CV MED group. Here, “1-year mortality after ICU discharge” was defined as the mortality of ICU survivors within 1 year of the date of ICU discharge. The secondary outcome was 1-year mortality according to each cause of death (e.g., cardiovascular disease-related, cancer-related, neurologic disease-related, or injury or trauma-related deaths), compared between the CV MED and non-CV MED groups.
Covariates
The following covariate data were collected: (I) physical characteristics [sex, age, body mass index (BMI, kg/m2)]; (II) socioeconomic status related information (insurance type, highest educational attainment, occupation and marital status at ICU admission); (III) Acute Physiology and Chronic Health Evaluation II; (IV) comorbidities at ICU discharge (hypertension, diabetes mellitus, history of coronary disease and cerebrovascular disease, liver disease [hepatitis, liver cirrhosis, and fatty liver], chronic obstructive lung disease, chronic kidney disease, anemia and cancer); (V) main diagnosis at ICU admission (severe sepsis or septic shock; kidney failure; cardiac disease; vascular disease; respiratory insufficiency or failure; post cardiac arrest; neurologic disease; drug intoxication; trauma; gastrointestinal bleeding, ischemia, or perforation; hemorrhagic shock; and unstable heart rate or blood pressure); (VI) and length of ICU and hospital stay (day). The International Classification of Disease-10 diagnostic system was used when collecting comorbidity-related information, and main diagnosis at ICU admission was collected from the physician’s admission note. At the time of this study, there were two main types of health insurance in South Korea, a medical aid program and the national health insurance program. Patients in the medical aid program are classified as having low income, and most of their hospital charges are paid by the government. Meanwhile, for patients in the national health insurance program, approximately two-thirds of their hospital charges are covered by the government.
Statistical analysis
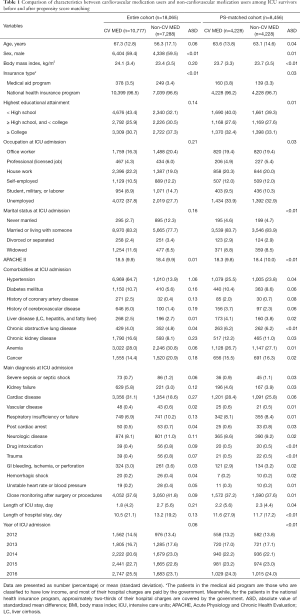
The patients’ baseline characteristics are presented as means with standard deviations or numbers with percentages. As the body mass index (BMI) on the day of ICU discharge was missing from 17.8% of the cases (3,216/18,071), we used PROC MI to perform multiple imputations to lessen bias. Here, we generated 5 data sets and substituted each missing value with the mean BMI value of five data sets (12). Next, we performed propensity score (PS) matching between the CV MED group and non-CV MED group to reduce confounders (13). For the PS matching, the nearest neighbor method was used by 1:1 ratio without replacement at caliper 0.1. As cardiovascular medication is usually prescribed to prevent cardiovascular or cerebrovascular disease, patients in the CV MED and non-CV MED groups might have differences in comorbidities (e.g., hypertension) or other characteristics. Therefore, we decided to use a conservative caliper of 0.1 to match the two groups. To determine balance between the two groups before and after PS matching, absolute standardized difference (ASD) was used. An ASD of <0.1 for the covariates indicated that the two groups were sufficiently balanced.
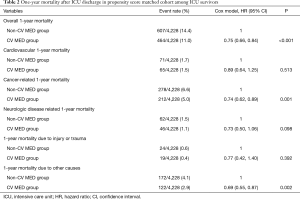
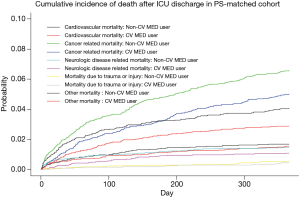
After PS matching, we used a Cox regression model to investigate the hazard ratio (HR) with 95% confidence interval (CI) of the CV MED group for 1-year mortality after ICU discharge, compared to the non-CV MED group. Next, we investigated cause-specific HRs for different causes of 1-year mortality (cardiovascular disease, cancer, neurologic disease, injury or trauma, and others) in the PS-matched cohort as a competing risk analysis. Additionally, cumulative incidence of the mortality due to different causes (cardiovascular disease, cancer, neurologic disease, injury or trauma, and others) between the two groups in PS-matched cohort was shown as a graph.
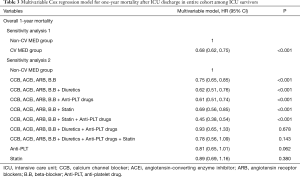
We then performed two sensitivity analyses. First, to determine that the results in the PS-matched cohort were generalizable in the entire cohort of ICU survivors, we performed multivariable Cox regression analysis for 1-year mortality using all covariates. Second, to determine the effect of combinations of cardiovascular drugs, the CV MED group was divided into nine groups, and all groups were included in the multivariable Cox regression model. To avoid multi-collinearity, the two sensitivity analyses were performed in different models. Each multivariable Cox regression analysis that satisfied the central assumption of a Cox proportional hazard model was verified using a log-log plot. The absence of multi-collinearity within each multivariable model was confirmed based on a variance inflation factor <2.0. Finally, the compliance rates (%) of each cardiovascular medication at 90 days after ICU discharge was determined by evaluating 100 patients per medication; these patients were randomly selected among ICU survivors who were followed up at our institution. To detect a 2% difference in the incidence of the 1-year mortality between the CV MED group and non-CV MED group with a 0.05 chance of type 1 error and 80% power in a PS-matched cohort, a total of 8,288 patients (4,144 patients in each group) were required.
The packages of ‘MatchIt’, ‘Cmprsk’, and ‘Survival’ of the R program (Version 3.6.0; R Foundation for Statistical Computing, Vienna, Austria) were used for propensity score matching, competing risk analysis, and Kaplan-Meier estimation, respectively. All other statistical analyses were performed with SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA), and P<0.05 was considered significant.
Results
A total of 34,245 ICU admissions involving 25,079 patients were recorded between January 2012 and December 2016. After excluding multiple ICU admissions for single patients (n=9,166), 25,079 patients/final ICU admission cases were included in the analysis. Subsequently, the following patients were further excluded: 4,925 children (age: <18 years); 1,505 patients who died during their stay in the ICU; and 261 patients with inaccurate or missing information about cardiovascular medication prescribed at ICU discharge. Consequently, the final analysis included 18,065 ICU survivors, of whom 2,218 (12.3%) died within 1 year of ICU discharge. Of these deaths, 291 were cardiovascular-related (1.6%), 1,046 were cancer-related (5.8%), 203 were neurologic disease-related (1.1%), and 101 were injury or trauma-related (0.6%). Additionally, 577 deaths (3.2%) were not included in the four categories mentioned above (Figure 1). Among a total of 18,065 ICU survivors, 10,777 and 7,288 patients were categorized into the CV MED group and non-CV MED group, respectively. After PS matching, a total of 8,456 patients (4,228 patients in each group) were included in the analyses. The characteristics of patients in the CV MED and non-CV MED groups before and after PS matching are presented in Table 1. The two groups were well balanced after PS matching (ASD < 0.1), and distribution of propensity scores were similar after PS matching (Figure S1). Compliance for each cardiovascular medication in the 90 days after ICU discharge, evaluated by randomly selecting 100 patients per medication from among ICU survivors, is presented in Table S1.
Full table
Survival analysis
Table 2 shows the results of the survival analysis in the PS-matched cohort. In the Cox regression model, overall 1-year mortality after ICU discharge was 25% lower in the CV MED group, compared to the non-CV MED group (HR: 0.75, 95% CI: 0.66 to 0.84; P<0.001). In the competing risk analysis, cancer-related 1-year mortality was 26% lower in the CV MED group (HR: 0.74, 95% CI: 0.62 to 0.89; P=0.001) The cumulative incidence for mortality due to each cause after ICU discharge in the PS-matched cohort is presented in Figure 2.
Full table
Sensitivity analysis
Table 3 shows the results of the sensitivity analyses. In the multivariable Cox regression model of the entire cohort, 1-year mortality in the CV MED group was 32% lower (HR: 0.68, 95% CI: 0.62 to 0.75; P<0.001; sensitivity analysis 1) than that in the non-CV MED group. The HRs with 95% CI for 1-year mortality of other covariates are presented in Table S2. In the second sensitivity analysis (Table 3), group 1 (calcium channel blocker, ACE inhibitor, ARB, beta-blocker), group 2 (calcium channel blocker, ACE inhibitor, ARB, beta-blocker + diuretics), group 3 (calcium channel blocker, ACE inhibitor, ARB, beta-blocker + anti-platelet drugs), group 4 (calcium channel blocker, ACE inhibitor, ARB, beta-blocker + statin), and group 5 (calcium channel blocker, ACE inhibitor, ARB, beta-blocker + statin + anti-platelet drug) showed lower 1-year mortality than the non-CV MED group.
Full table
Discussion
This retrospective study demonstrated associations of the use of various cardiovascular medications (calcium channel blockers, beta-blockers, ARB, ACE inhibitor, aspirin, and statins) with decreases in the rates of 1-year mortality among ICU survivors. This association was more evident for cancer-related 1-year mortality. Our results suggest that the prescription of cardiovascular medications might have potential benefits for the long-term outcomes of ICU survivors.
This study is significant because it provides the first concrete evidence of associations between the use of cardiovascular medications at the time of ICU discharge and long-term mortality in ICU survivors. The first noteworthy point is the identification of associations between three anti-hypertensive medications (calcium channel blockers, beta-blockers, and ARB or ACE inhibitors) with decreases in overall 1-year mortality among ICU survivors. Several factors may have contributed to this outcome. The effective regulation of chronic hypertension, which is known to play an important role in reducing mortality and morbidity in the general population (14), may have also played an important role in improving 1-year mortality among critically ill patients, including ICU survivors (15). Hypertension causes damage to organs and thereby represents a primary risk factor for increased cardiovascular events and related mortality (16). As ICU survivors have a higher risk of post-discharge major adverse cardiovascular events relative to the general population (10), our findings suggest a close association between the active management of hypertension and improved prognosis in ICU survivors.
The secondary effects of anti-hypertensive medications may also have affecting the results of this study. Sepsis, a common complication among critically ill patients, is associated with increased Ca2+ activity in many cell types and, consequently, cytotoxicity or cell death (17). Related cohort studies have reported an association of the use of pre calcium channel blockers prior to admission with reduced mortality in patients with sepsis (8,9). Unlike other anti-hypertensive medications, beta-blockers are associated with a reduction in heart rate. Consistent with this characteristic, a randomized controlled trial and observational studies have reported that beta-blockers can reduce mortality among patients with sepsis or critically illness (18,19). An elevated heart rate was found to correlate with an increased risk of major cardiac events among critically ill patients (20). Therefore, the reduced heart rate consequent to beta-blocker use may be associated with the observed improvement in 1-year mortality among ICU survivors.
The results of the competing risk analysis in the PS-matched cohort are also interesting. While cardiovascular medication prescribed at ICU discharge was not associated with cardiovascular or neurologic disease-related 1-year mortality among ICU survivors, it was related with cancer-related 1-year mortality. We focused on relatively older patients who had survived critical illness in the ICU; thus, it is possible that some of the patients could have been prescribed various cardiovascular medications by their primary physician in the community, after hospital discharge. Therefore, it cannot be guaranteed that the non-CV MED group never used any cardiovascular medication during the first year after ICU discharge. As cardiovascular medication is known to prevent coronary event or stroke (21), the effect of cardiovascular medication on cardiovascular or neurologic disease-related 1-year mortality could have been attenuated if any of the non-CV MED ICU survivors began to take CV medication after ICU discharge.
On the other hand, the effects of cardiovascular medication on cancer are controversial. Various types of anti-hypertensive medications were reported to have an association with cancer risk (22,23), but were also reported to have no association (24). However, 17.0% (3,075/18,065) of our cohort of ICU survivors were patients who had been previously diagnosed with cancer, including cases of advanced cancer. Therefore, the 1-year cancer-related mortality might be related to the progression of cancer in that population, rather than reflecting newly diagnosed cancer patients. Among the various cardiovascular medications, statins are known to have the potential benefit of reducing cancer progression or cancer-related mortality (25). Beta blockers also have a potential survival benefit in patients with ovarian cancer, pancreatic cancer, and melanoma (26). Furthermore, one epidemiological study reported that ARB use reduced cancer-specific mortality in patients with esophageal cancer (27). However another study reported that post-diagnostic calcium channel blocker use had no benefit for breast cancer mortality (28), and it has even been reported that aspirin use in healthy adults could increase cancer-related mortality (29). Furthermore, a recent cohort study in South Korea reported that various cardiovascular medications, such as aspirin and statins, were associated with a lower incidence of lung cancer and lung cancer-related mortality (30). Although evidence has been increasingly reported regarding the lower cancer risk benefits of cardiovascular medications (22,23,26,27,30), additional study is needed to identify risks of various cardiovascular medications for the long-term outcome of patients, especially among ICU survivors.
The present study has some additional limitations. First, the use of a retrospective design may have led to selection bias. Second, this was a single-center study, and therefore the findings may not be generalizable to other populations. Third, the ICU survivors in this study were heterogenous (patients from internal medicine, neurological, or surgical departments), which might have affected our results. Fourth, cardiovascular medications were investigated at the time of discharge from the ICU. Although we investigated the compliance rate in the 90 days after ICU discharge by evaluating 100 randomly-selected ICU survivors per medication, adherence to cardiovascular medication is not guaranteed in our entire cohort. Lastly, non-CV MED users at ICU discharge could have started to take cardiovascular medication after ICU discharge, which also could have affected our results.
Conclusions
The present study revealed associations of the uses of various cardiovascular medications (calcium channel blockers, beta-blockers, ARB, aspirin, ACE inhibitor, and statins) at ICU discharge with decreases in 1-year overall mortality among ICU survivors, compared to those who did not use cardiovascular medication at ICU discharge. This association was more evident for cancer-related 1-year mortality. Our result suggested that with proper indication, cardiovascular medications might have beneficial long-term outcomes among ICU survivors.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1786
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1786
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1786). Both authors have no other conflicts of interest to declare.
Ethical Statement: the authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This retrospective observational study was conducted with approval from the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (SNUBH) (IRB approval number: B-1902/522-105). The requirement to obtain informed consent from each patient was waived by the IRB, given the retrospective observational study design and inclusion of medical records from patients who had completed treatment. The study also conformed to the provisions of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Brinkman S, de Jonge E, Abu-Hanna A, Arbous MS, de Lange DW, de Keizer NF. Mortality after hospital discharge in ICU patients. Crit Care Med 2013;41:1229-36. [Crossref] [PubMed]
- Goldhill DR, Sumner A. Outcome of intensive care patients in a group of British intensive care units. Crit Care Med 1998;26:1337-45. [Crossref] [PubMed]
- Moreno R, Morais P. Outcome prediction in intensive care: results of a prospective, multicentre, Portuguese study. Intensive Care Med 1997;23:177-86. [Crossref] [PubMed]
- Winters BD, Eberlein M, Leung J, et al. Long-term mortality and quality of life in sepsis: a systematic review. Crit Care Med 2010;38:1276-83. [Crossref] [PubMed]
- Gayat E, Cariou A, Deye N, et al. Determinants of long-term outcome in ICU survivors: results from the FROG-ICU study. Crit Care 2018;22:8. [Crossref] [PubMed]
- Rossello X, Pocock SJ, Julian DG. Long-Term Use of Cardiovascular Drugs: Challenges for Research and for Patient Care. J Am Coll Cardiol 2015;66:1273-85. [Crossref] [PubMed]
- Lai CC, Wang YH, Wang CY, et al. Risk of Sepsis and Mortality Among Patients With Chronic Obstructive Pulmonary Disease Treated With Angiotensin-Converting Enzyme Inhibitors or Angiotensin Receptor Blockers. Crit Care Med 2019;47:e14-e20. [Crossref] [PubMed]
- Lee CC, Lee MG, Lee WC, et al. Preadmission Use of Calcium Channel Blocking Agents Is Associated With Improved Outcomes in Patients With Sepsis: A Population-Based Propensity Score-Matched Cohort Study. Crit Care Med 2017;45:1500-8. [Crossref] [PubMed]
- Wiewel MA, van Vught LA, Scicluna BP, et al. Prior Use of Calcium Channel Blockers Is Associated With Decreased Mortality in Critically Ill Patients With Sepsis: A Prospective Observational Study. Crit Care Med 2017;45:454-63. [Crossref] [PubMed]
- Park S, Lee S, Kang MW, et al. Postdischarge Major Adverse Cardiovascular Events of ICU Survivors Who Received Acute Renal Replacement Therapy. Crit Care Med 2018;46:e1047-54. [Crossref] [PubMed]
- Yoo S, Lee KH, Lee HJ, et al. Seoul National University Bundang Hospital's Electronic System for Total Care. Healthc Inform Res 2012;18:145-52. [Crossref] [PubMed]
- Pedersen AB, Mikkelsen EM, Cronin-Fenton D, et al. Missing data and multiple imputation in clinical epidemiological research. Clin Epidemiol 2017;9:157-66. [Crossref] [PubMed]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41-55. [Crossref]
- Danaei G, Ding EL, Mozaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med 2009;6:e1000058 [Crossref] [PubMed]
- Salgado DR, Silva E, Vincent JL. Control of hypertension in the critically ill: a pathophysiological approach. Ann Intensive Care 2013;3:17. [Crossref] [PubMed]
- Redon J, Tellez-Plaza M, Orozco-Beltran D, et al. Impact of hypertension on mortality and cardiovascular disease burden in patients with cardiovascular risk factors from a general practice setting: the ESCARVAL-risk study. J Hypertens 2016;34:1075-83. [Crossref] [PubMed]
- Song SK, Karl IE, Ackerman JJ, et al. Increased intracellular Ca2+: a critical link in the pathophysiology of sepsis? Proc Natl Acad Sci U S A 1993;90:3933-7. [Crossref] [PubMed]
- Morelli A, Ertmer C, Westphal M, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 2013;310:1683-91. [Crossref] [PubMed]
- Schmittinger CA, Dunser MW, Haller M, et al. Combined milrinone and enteral metoprolol therapy in patients with septic myocardial depression. Crit Care 2008;12:R99. [Crossref] [PubMed]
- Sander O, Welters ID, Foex P, et al. Impact of prolonged elevated heart rate on incidence of major cardiac events in critically ill patients with a high risk of cardiac complications. Crit Care Med 2005;33:81-8; discussion 241-2. [Crossref] [PubMed]
- Fleg JL, Aronow WS, Frishman WH. Cardiovascular drug therapy in the elderly: benefits and challenges. Nat Rev Cardiol 2011;8:13-28. [Crossref] [PubMed]
- Huang T, Poole EM, Eliassen AH, et al. Hypertension, use of antihypertensive medications, and risk of epithelial ovarian cancer. Int J Cancer 2016;139:291-9. [Crossref] [PubMed]
- Li CI, Daling JR, Tang MT, et al. Use of antihypertensive medications and breast cancer risk among women aged 55 to 74 years. JAMA Intern Med 2013;173:1629-37. [Crossref] [PubMed]
- Boudreau DM, Koehler E, Rulyak SJ, et al. Cardiovascular medication use and risk for colorectal cancer. Cancer Epidemiol Biomarkers Prev 2008;17:3076-80. [Crossref] [PubMed]
- Mei Z, Liang M, Li L, et al. Effects of statins on cancer mortality and progression: A systematic review and meta-analysis of 95 cohorts including 1,111,407 individuals. Int J Cancer 2017;140:1068-81. [Crossref] [PubMed]
- Na Z, Qiao X, Hao X, et al. The effects of beta-blocker use on cancer prognosis: a meta-analysis based on 319,006 patients. Onco Targets Ther 2018;11:4913-44. [Crossref] [PubMed]
- Busby J, McMenamin U, Spence A, et al. Angiotensin receptor blocker use and gastro-oesophageal cancer survival: a population-based cohort study. Aliment Pharmacol Ther 2018;47:279-88. [Crossref] [PubMed]
- Busby J, Mills K, Zhang SD, et al. Post-diagnostic calcium channel blocker use and breast cancer mortality: a population-based cohort study. Epidemiology 2018;29:407-13. [Crossref] [PubMed]
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of Aspirin on All-Cause Mortality in the Healthy Elderly. N Engl J Med 2018;379:1519-28. [Crossref] [PubMed]
- Kang J, Jeong SM, Shin DW, et al. Associations of aspirin, statins, and metformin with lung cancer risk and related mortality: time-dependent analysis of population-based nationally representative data. J Thorac Oncol 2021;16:76-88. [Crossref] [PubMed]



