
Randomized trial of the application value of comprehensive nursing intervention in the perioperative period of ruptured bleeding of ectopic pregnancy
Introduction
Ectopic pregnancy refers to the implantation and development of fertilized eggs outside the cavity of the uterus. The typical symptoms are menopause, abdominal pain, and vaginal bleeding (1). At present, the incidence of ectopic pregnancy is increasing year by year. According to statistics, ectopic pregnancy accounts for 1–2% of pregnancies and 2.7% of pregnancy-related deaths, and leads to a high incidence of ectopic pregnancy in subsequent pregnancies (2,3). Ectopic pregnancy rupture and bleeding are common acute abdomen in obstetrics and gynecology, and are also important causes of death in women during the first trimester. More than 95% of ectopic pregnancies are fallopian tube pregnancies, and the other 2.5% occur in the uterine horns. A very small number may occur in the ovaries, cervix, or abdominal cavity (4). Because these parts are not conducive to placental implantation and embryo development, rupture and the possibility of heavy bleeding exists at any time.
Laparoscopic surgery is the first choice for the treatment of ectopic pregnancy (5). Its intraoperative vision is clear, which can help doctors quickly find the lesion and remove it in time. In addition, laparoscopic surgery is performed in an almost completely closed pelvic cavity, which can prevent the exposure of organs to the air and damage to tissues by gloves and gauze, and reduce the occurrence of pelvic and abdominal adhesions. With the continuous improvement of the technical level and the proficiency of surgeons, as well as the continuous improvements in laparoscopic equipment, even the patients with ectopic pregnancy rupture, bleeding or even shock can be effectively treated during the operation through active anti-shock (6). However, laparoscopic surgery is still an invasive operation, and the incision may also have complications such as bleeding, infection, incisional hernia, and subcutaneous emphysema (7). The occurrence of complications not only increases the patient’s pain, but may also affect wound healing and cause surgical failure.
Perioperative period refers to the period of time between the establishment of surgical treatment and the completion of the treatment related to the operation (8,9). In recent years, laparoscopic surgery has been widely used in the surgical treatment of ectopic pregnancy. With the continuous development of laparoscopic technology, perioperative nursing intervention carried out in conjunction with laparoscopic surgery has also progressed from a traditional single nursing model to a new type with strong comprehensiveness. This nursing mode is helpful for promoting the recovery of patients and reducing the occurrence of complications. To this end, the purpose of this study was to compare nursing interventions in 164 patients with ectopic pregnancy hemorrhage who were admitted to the Department of Gynecology in our hospital from January 2015 to January 2020 who were given either comprehensive nursing intervention or basic nursing intervention during the perioperative period. The objective is to provide a relevant basis for clinical care and promote faster recovery of patients. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/apm-21-692).
Methods
General information
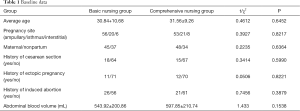
From January 2015 to January 2020, 164 patients with rupture and bleeding of ectopic pregnancy who needed laparoscopic treatment in the gynecology department of our hospital were selected and randomly divided into the basic nursing group and comprehensive nursing group, with 82 cases each. There were no significant differences between the two groups in terms of baseline data (Table 1).
Full table
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all individual participants. The study was approved by Zhuji Maternal and Child Health Care Hospital (No.:2014-1832).
Nursing plan
Basic perioperative nursing plan: (I) preoperative care: after the patient was admitted to the hospital, the nurse assisted the doctor to ask for a detailed medical history, conduct a comprehensive physical examination, connect several parameter monitors, and determine the patient’s condition as soon as possible based on the degree of abdominal pain, complexion, pulse, respiration, central venous pressure, urine output, severity, quick and accurate establishment to a venous channel, rapid fluid rehydration, blood transfusion, and close observation of the patient’s vital signs. Oxygen was inhaled at 4–6 L/min, and if necessary, the face mask was pressurized to maintain oxygen saturation above 95%. Absolute bed rest was required, and the abdomen was not pressed. The amount of vaginal bleeding was observed and recorded. The nurse promptly replenished the effective circulating blood volume and treated shock according to the doctor’s advice. While fighting shock, all preoperative preparations were quickly completed, including instructing patients to abstain from eating and drinking, indwelling urinary catheters, and preparing skin for the operation area. Cross-matching blood and blood transfusion bought time for patients to get surgical treatment early.
(II) Intraoperative care: the doctor was assisted in performing general anesthesia, and the patient was placed in a supine position with abduction fixation; vital signs were monitored to keep the airway unobstructed; the pressure of CO2 pneumoperitoneum was maintained at 10–15 mmHg, the airflow speed was controlled; the patient’s body was prevented from being compressed and from touching metal devices.
(III) Postoperative care: the patient was returned to the ward, and the patient’s blood pressure, heart rate, respiration, blood oxygen saturation, were continually monitored to keep the airway unobstructed, and to keep the infusion and urinary tubes unobstructed. The amount of entry and exit for 24 hours after the operation was accurately recorded to maintain a balance of entry and exit. Patients were required to fast after the operation. After 6 hours, they could have liquid, and after 12 hours, they could have semi-liquids. When the bowel sounds were restored and the anus was exhausted, they were changed to a normal diet. After the blood pressure had stabilized 6 hours after the operation, patients were placed in a semi-recumbent position and turned over appropriately.
Comprehensive perioperative nursing plan: on the basis of the basic perioperative nursing program, the perioperative psychological intervention and health education, infection preventive nursing intervention, thermal insulation nursing intervention, and discharge guidance were strengthened.
(I) Health education and psychological intervention: most patients lack disease and medical knowledge, and the prominent psychological response is anxiety and panic, especially in young patients. Before the operation, the procedure was patiently and carefully explained, and patients were comforted to eliminate the patient’s worries. Relevant medical knowledge, successful cases of conservative treatment, and the pros and cons of surgical treatment were introduced if necessary to both the patients and their families, and questions raised by patients and their families were answered patiently. Preoperative health education for patients and their families before surgery was carried out to inform them of the purpose of laparoscopic surgery, and increase patients’ understanding of laparoscopic surgery. After the operation, due to the small surgical incision, the patients could tolerate the local soreness caused by the accumulation of carbon dioxide. Psychological comfort and encouragement were given to the patients.
(II) Insulation nursing intervention: an electric blanket was laid on the operating table 1 hour before the operation to warm it up to a suitable temperature. At the same time, the insulation blanket was spread to cover the parts outside the surgical area. Close attention was paid to the patient’s core body temperature during the operation. If it was found that their body temperature was less than 37.5 °C, an electric blanket was used. If it was above 37.5 °C, the electric blanket was turned off temporarily. During the operation, the infusion warmer was used to heat the blood and liquid, and the flushing liquid was heated to approximately 38 °C in advance, so that the input of various liquids was close to the body temperature. The humidification heat exchanger was connected to the patient’s tracheal tube to maintain a constant temperature and moderateness in the respiratory tract. The blood circulation pump pressure belt and foot cover were tied to the patient’s lower limbs to provide good preconditions for venous return and warmth.
(III) Infection preventive nursing intervention: the puncture hole was replaced daily and kept clean to prevent infection. For patients with a drainage tube, the color and quantity of the drainage fluid was observed 1 to 2 hours after surgery, and removed after 24 to 48 hours.
(IV) Discharge guidance: nurses carefully taught patients about the precautions after discharge, and instructed patients not to engage in heavy physical labor within 2 weeks, strengthen nutrition, and try to eat high-calorie, high-protein, rich in vitamins, light, and easy-to-digest foods. Patients were told to keep warm daily and avoid catching a cold. The patients were also informed that human chorionic gonadotropin (HCG) would be reviewed 1 week after surgery, and to do a good job of using contraception within 1 month to prevent pregnancy. If the patient had abdominal pain, increased vaginal bleeding, and other abnormalities, they were followed up in time.
Observation indicators
The time to the clearance of the abdominal hemorrhage, the time to anus exhaust, the time for the abdominal pain to disappear, the recovery time of bowel sounds, the time to get out of bed, the length of hospitalization, the degree of recovery at discharge, the occurrence of complications, and the blockage of the fallopian tubes were recorded. The stress levels of all patients before and after surgery were measured. The Visual Analogue Scale (VAS) was performed on all patients after the operation. The Hamilton Depression Scale (HAMD) scores and Hamilton Anxiety Scale (HAMA) scores before and after psychological intervention were compared. Recurrence was determined at follow-up.
Statistical analysis
SPSS 22.0 statistical software was used for processing. Measurement data were expressed as mean ± standard deviation (), LSD-t-test was used for inter-group comparison, and paired t test was used for intra-group comparison. Enumeration data were expressed as rate (%), and χ2 test was used for comparison between groups. P<0.05 indicated that the difference was statistically significant.
Results
Surgical outcomes
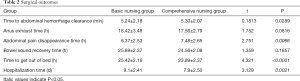
The research process is shown in Figure 1. The disappearance time of abdominal pain, the time to get out of bed, and the length of hospital stay in the comprehensive care group were significantly shorter than those in the basic care group (P<0.05) (Table 2).
Full table
Changes in stress levels before and after surgery
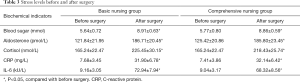
After surgery, blood sugar levels, aldosterone, cortisol, C-reactive protein (CRP), and IL-6 in the two groups were significantly higher than those before surgery (P<0.05), but there was no statistically significant difference between the groups (P>0.05) (Table 3).
Full table
Postoperative VAS scores
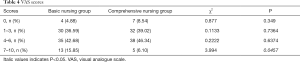
After the operation, the proportion of patients in the comprehensive nursing group with a VAS score of 7–10 was significantly lower than that in the basic nursing group (P<0.05) (Table 4).
Full table
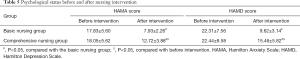
Psychological status before and after nursing intervention
Before the intervention, the HAMA and HAMD scores of the two groups of patients were compared, and the differences were not statistically significant (P>0.05). After the intervention, the HAMA and HAMD scores of the comprehensive nursing group were significantly lower than those of the basic nursing group (P<0.05) (Table 5).
Full table
Nursing effect
The fallopian tube recanalization rate of patients in the comprehensive care group was significantly higher than that of the basic care group (P<0.05), and the complication rate was significantly lower than that of the basic care group (P<0.05). There was no significant difference in the 1 year recurrence rate between the two groups (P>0.05) (Table 6).

Full table
Discussion
Ectopic pregnancy is one of the most common clinical acute abdomen conditions, with sudden onset and rapid development. The blood vessels at the site of pregnancy can easily rupture and cause massive bleeding. If rescue is not timely, it may be life-threatening. Therefore, if the patient has symptoms such as menopause, abdominal pain, and vaginal bleeding, diagnosis and treatment in hospital are immediately required (10). Laparoscopic surgery is an ideal surgical method for the treatment of ectopic pregnancy. Correct diagnosis and treatment with laparoscopic surgery can greatly reduce the mortality rate of patients and improve the prognosis of patients. For experienced laparoscopic doctors, if the patient can anesthesia and monitoring of a patient’s various vital signs, coupled with supportive care as necessary, patients can still choose laparoscopic surgery even if there is internal bleeding or hemodynamic changes. In addition to correct medical measures, postoperative nursing intervention is also of great significance for the recovery of patients and the improvement of quality of life (11,12). Studies have pointed out that active nursing measures can facilitate successful operation of patients with ruptured bleeding in ectopic pregnancy, and promote clinical efficacy (13).
Comprehensive perioperative nursing intervention can be traced back to the 19th century. The United States first proposed case management, that is, to manage patients as a whole. At that time, it was mainly to solve the problem that scarce medical resources could not benefit every citizen, and to improve the health care system so that working people and immigrants could receive the same medical treatment. After a century of development, the term ‘integrated management’ was formally devised in the middle of the 20th century. Comprehensive nursing intervention developed from this, and formed the thinking mode of integrating nursing process (14). It is a comprehensive, dynamically changing, decision-making, and feedback process. In the practice of comprehensive nursing intervention, it is necessary to use multidisciplinary knowledge to deal with the health problems of the client, and make adjustments at any time with the continuous changes of health problems. Furthermore, it involves helping the client decide to take appropriate nursing measures, through the evaluation and appropriate adjustment of cases, plans, implementation, and feedback to meet the health needs of patients. At present, comprehensive perioperative nursing intervention has been widely used in various clinical fields including pancreatectomy (15), and has achieved certain results. Mathlouthi et al. (16) performed comprehensive care during laparoscopic surgical treatment of ectopic pregnancy. The results showed that all 160 patients achieved the expected curative effect, and there were no infections and complications after surgery. Ganesh et al. (17) also showed that appropriate nursing intervention can reduce the incidence of complications. The above research suggests that laparoscopic surgery should improve various preoperative preparations, strengthen intraoperative nursing cooperation, and may strengthen the treatment of ectopic pregnancy. For other aspects of nursing, close observation of the patient’s postoperative state, active treatment of complications, and detailed discharge guidance are key to achieving the expected curative effect. At present, comprehensive perioperative nursing intervention has also formed a complete nursing system, but the nursing intervention in each specialty field is very different.
The comprehensive perioperative care plan of this study was as follows: On the basis of the basic perioperative nursing plan, the perioperative psychological intervention and health education, infection preventive nursing intervention, thermal insulation nursing intervention, and discharge guidance were strengthened. The results showed that the disappearance time of abdominal pain, the time to get out of bed, and the length of hospital stay in the comprehensive nursing group were significantly shorter than those in the basic nursing group (P<0.05). The fallopian tube recanalization rate of patients in the comprehensive care group was significantly higher than that of the basic care group (P<0.05), and the complication rate was significantly lower than that of the basic care group (P<0.05). The comprehensive care group had a VAS score of 7–10. The ratio was significantly lower than that of the basic nursing group (P<0.05). The above results indicate that the comprehensive perioperative nursing program is more effective. It can improve the pain level of the patient to a certain extent, the patient can recover quickly, and it can significantly reduce the occurrence of complications. The HAMA and HAMD scores of the comprehensive nursing group after the nursing intervention were significantly lower than those before the intervention, and were significantly lower than those of the basic nursing group (P<0.05). Health education and psychological intervention are helpful for improving the patient’s ability to master relevant knowledge, reduce false cognition, improve patients’ acceptance of treatment and nursing, cooperate more with nursing staff, and improve compliance. At the same time, targeted psychological counseling can relieve the poor mental state of patients with ectopic pregnancy, help them establish an optimistic attitude, and actively receive treatment.
In summary, a comprehensive nursing program during the perioperative period can improve the treatment effect and significantly shorten the recovery time of patients, which is worthy of clinical promotion.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-692
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-692
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-692). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was taken from all individual participants. The study was approved by Zhuji Maternal and Child Health Care Hospital (No.:2014-1832).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Escobar-Padilla B, Perez-López CA, Martínez-Puon H. Risk factors and clinical features of ectopic pregnancy Rev Med Inst Mex Seguro Soc 2017;55:278-85. [PubMed]
- Hendriks E, Rosenberg R, Prine L. Ectopic Pregnancy: Diagnosis and Management. Am Fam Physician 2020;101:599-606. [PubMed]
- Brady PC. New Evidence to Guide Ectopic Pregnancy Diagnosis and Management. Obstet Gynecol Surv 2017;72:618-25. [Crossref] [PubMed]
- ACOG Practice Bulletin No. 191 Summary: Tubal Ectopic Pregnancy. Obstet Gynecol 2018;131:409-11. [Crossref] [PubMed]
- Beyan E, Kanmaz AG, Budak A, et al. Uterine manipulator requirement in laparoscopic surgery of Ectopic Pregnancy. Pak J Med Sci 2020;36:105-10. [PubMed]
- Chen L, Wen H, Xu D, et al. Management and pregnancy outcomes of heterotopic pregnancy. Zhonghua Fu Chan Ke Za Zhi 2018;53:768-75. [PubMed]
- Ahmad G, Baker J, Finnerty J, et al. Laparoscopic entry techniques. Cochrane Database Syst Rev 2019;1:CD006583 [PubMed]
- Brown Will SE. Perioperative Nursing Care in Obstetrics and Gynecology. AORN J 2019;110:130-3. [Crossref] [PubMed]
- Sillero-Sillero A, Zabalegui A. Safety and satisfaction of patients with nurse’s care in the perioperative. Rev Lat Am Enfermagem 2019;27:e3142 [Crossref] [PubMed]
- Goettler S, Zanetti-Dällenbach R. Heterotopic Pregnancy. Heterotopic Pregnancy. N Engl J Med 2016;375:1982. [Crossref] [PubMed]
- Tenzel NS, Patel D. Laparoscopic diagnosis and treatment of an advanced ectopic pregnancy in an asymptomatic woman. Minim Invasive Gynecol J 2017;24:S188. [Crossref]
- Xu Y, Wang H, Yang M. Preoperative nursing visit reduces preoperative anxiety and postoperative complications in patients with laparoscopic cholecystectomy: A randomized clinical trial protocol. Medicine (Baltimore) 2020;99:e22314 [Crossref] [PubMed]
- Fields L, Hathaway A. Key Concepts in Pregnancy of Unknown Location: Identifying Ectopic Pregnancy and Providing Patient-Centered Care. J Midwifery Womens Health 2017;62:172-9. [Crossref] [PubMed]
- Tuominen L, Stolt M, Meretoja R, et al. Effectiveness of nursing interventions among patients with cancer: An overview of systematic reviews. J Clin Nurs 2019;28:2401-19. [Crossref] [PubMed]
- Nahabedian MY, Nahabedian AG. Panniculectomy: Perioperative nursing considerations. Nursing 2017;47:32-8. [Crossref] [PubMed]
- Mathlouthi N, Slimani O, Fatnassi A, et al. Ultrasound diagnosis of ectopic pregnancy: prospective study of 200 cases. Tunis Med 2013;91:254-7. [PubMed]
- Ganesh D, Rajkumar A, Rajkumar JS, et al. Ruptured Ectopic Pregnancy with Contralateral Ovarian Serous Cyst Adenoma Torsion: Laparoscopic Management of Double Trouble. Case Rep Obstet Gynecol 2016;2016:2980941 [Crossref] [PubMed]
(English Language Editor: C. Betlazar-Maseh)



