
Effect analysis of embracing breast milk sucking to relieve pain of neonatal heel blood sampling: a randomized controlled trial
Introduction
Heel blood sampling of newborns plays an important role in the diagnosis of genetic and metabolic diseases, such as hypothyroidism and phenylketonuria (1,2). However, heel blood sampling is a painful procedure, and newborns experience pain that can cause their metabolism to increase and stress reactions, such as increased heart rate and abnormal immune function (3). In addition, repeated painful stimulation is likely to damage the development of neonatal nerve cells, causing a series of behavioral changes in childhood, affecting their normal motor and brain function development in the future (4,5). Effective intervention is needed to relieve the pain of newborns with heel blood sampling. As the physiological functions of newborns are not yet fully developed, drugs cannot be used to relieve pain; therefore, non-drug-based interventions are particularly important for newborns with heel blood sampling (6). The non-drug interventions studied by scholars at home and abroad include oral sucrose or glucose solution, breast milk sucking, music therapy, kangaroo nursing and non-nutritional sucking, etc., which are effective in preventing and alleviating mild to moderate pain (7). Breastfeeding does not have the potential side effects of sucrose administration, while hugging can increase the sense of security of newborns (8). A number of studies have reported on the effects of milk on procedural pain in term neonates. Although the findings from these studies have been variable (9). We aimed to combined with the influence of the mother’s hug and breastfeeding on the pain score and physiological indexes of heel blood collection, to find a simple, effective, safe and easy to implement nursing intervention measures to relieve the pain caused by heel blood collection of premature infants.
Few studies to date, however, have examined the effects of EBMS on procedural pain in neonates. Hence, the aim of this randomized controlled trial was to determine whether EBMS reduces procedural pain associated with heel lancing in preterm neonates.
We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/apm-21-329).
Methods
Patient selection
A total of 96 neonates undergoing heel blood screening were selected from June 2019 to June 2020, and were randomly divided into 2 groups (n=48 cases in each group). In the control group, there were 28 males and 20 females (age 2–29 days, average age: 12.15±3.21 days, weight: 2,500–4,000 g, average weight: 3,215.65±10.97 g). In the observation group, there were 30 males and 18 females (age 2–29 days, average age: 12.20±3.15 days, weight 2,500–4,000 g, average weight: 3,290.41±10.65 g). There were no statistically significant differences in general data between the 2 groups (P>0.05). Inclusion criteria were as follows (I) heel blood sampling was not performed within 30 days of birth; (II) Apgar score ≥8 points in 5 min; and (III) body temperature ranged from 37 to 37.5 °C, and heart rate ranged from 110 to 160 beats/min. Exclusion criteria were as follows: (I) heel blood sampling was previously unsuccessful; (II) complicated with sepsis, respiratory distress syndrome, and other diseases; (III) need for oxygen or other respiratory assistance; (IV) congenital heart disease or other cardiovascular diseases; (V) received sedative or analgesic injection within 24 h before blood sampling; and (VI) the mother of the newborn had a cold or fever and had used sedatives and analgesics before blood sampling. The study was approved by the Ethics Committee of Haian People’s Hospital [ethics approval number: (2019) KY033] and was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Mothers of every neonate provided informed consent.
Interventions
The control and observation groups had the same blood collection method. The specific operation steps are as follows. The heel of the newborn was exposed, and the medical staff used the left hand to firmly grasp the newborn’s foot, relaxed after a while, and then firmly grasped. This was repeated 2 times. Second, a vertical line along the front edge of the newborn’s lateral ankle to the lateral edge of the plantar was measured, and the puncture point was the junction between the vertical line and the lateral edge of the plantar. Third, after the puncture point was determined, the medical staff disinfected the skin surface of the puncture point with medical alcohol and used a triangular needle to collect blood. The needle was inserted into the skin at an angle of 60°, with a depth of about 2–3 mm. After the puncture was made, the newborn’s heel was relaxed. Fourth, the medical staff should fix the newborn’s foot with their left hand, and the fixation strength should be appropriate to avoid harm to the newborn. Two fingers of the medical staff’s right hand were used to gently squeeze the needle around. After the blood flowed out, the first drop of blood was wiped with a cotton swab. The feet were repeatedly squeezed and relaxed, and blood was then collected after the formation of large blood drops. Fifth, used filter paper when taking blood to avoid contact with newborn skin. The filter paper directly touched the blood drop, so that the blood could penetrate both sides of the filter paper. Each blood drop diameter was ≥8 mm. Finally, a dry cotton swab was to press the puncture point to stop bleeding.
The control group was given routine intervention as follows: (I) medical staff prepared 3-sided blood sampling needles, medical alcohol, sterilized cotton swabs, and other items in advance for blood sampling; (II) prior to heel blood sampling, the medical staff controlled the indoor temperature to about 23 °C and about 60% humidity; (III) dedicated medical staff bathed the newborns and disinfected and collected blood from the heels of the newborns after the bath; and (IV) the newborn was wrapped in a quilt during blood collection to keep them warm.
The observation group was given EBMS on the basis of routine intervention, as follows. First, the room temperature and humidity were controlled before blood collection, and the medical staff guided the newborn mother to complete the preparations before blood sampling. Second, after the newborn was bathed, they were placed on the mother’s chest for skin-to-skin contact. The mother supported the newborn’s buttocks with 1 hand and the back with the other. Third, medical staff guided the mother to simulate the process of communicating with the newborn during pregnancy, and comforted the newborn. Finally, medical staff carried out heel blood sampling when the newborn was quiet.
Evaluation indexes
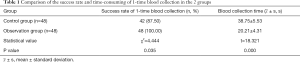
Success rate and time-consuming of 1-time blood collection
The 1-time success rate of neonatal blood sampling was observed and recorded. The blood collection time was from the beginning of the needle insertion to the successful collection of blood, and a stopwatch was used to time it.
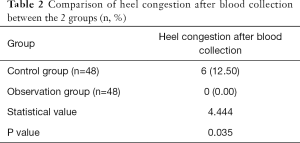
Heel congestion after blood collection
The condition of neonatal heel congestion after blood sampling was observed and recorded.
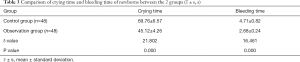
Crying time and bleeding time of newborns
“Cry” refers to the sound of a newborn crying. Use a stopwatch to record the crying time (s) and skin bleeding time (s) of the newborn during blood collection. The longer the duration, the more severe the neonatal pain is.
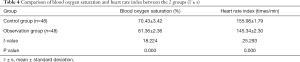
Blood oxygen saturation and heart rate index
Non-invasive blood oxygen saturation was used for monitoring, and probes were used to detect the end of the newborn’s finger, toe or earlobe, and other areas with abundant capillaries. The oxyhemoglobin oxygen content and hemoglobin oxygen capacity were measured, and the final blood oxygen saturation level was measured. The stethoscope was placed on the heart of the newborn, and the number of heartbeats and any changes in heart rate will be recorded.
Pain condition
The Neonatal Infant Pain Scale (NIPS) was used to evaluate neonatal pain (10). The scale is based on neonatal facial expressions (0–1 points), crying (0–2 points), breathing patterns (0–1 points), upper limb movements (0–1 points), lower limb movements (0–1 points), and the state of awakening (0–1 points). The total score is 0–7 points; 0–2 points indicate that the newborn has little or no pain, 3–4 points indicate that the newborn has moderate pain, and 5–7 points indicate that the newborn has severe pain.
Statistical analysis
SPSS version 20.0 (IBM, Armonk, NY, USA) was used for the statistical analysis. The blood collection time, crying time and bleeding time of newborns, blood oxygen saturation and heart rate index, and pain condition were expressed as mean ± standard deviation and compared using 2-tailed t-tests. The success rate of 1-time blood collection and heel congestion after blood collection was expressed by rate and percentage, and compared using the χ2-test or rank-sum test. P<0.05 was considered statistically significant.
Results
Success rate and time-consuming of 1-time blood collection
In the observation group, 48 cases were successfully collected at one-time blood sampling, and 42 cases in the control group were successfully collected at one-time blood sampling. The success rate of the observation group was higher than that in the control group (χ2=4.444, P=0.035). The blood collection time of the observation group was 20.21±4.31 s and that of the control group was 38.75±5.53 s. Comparing the 2 groups, the blood collection time of the observation group was significantly shorter than that of the control group (t=18.321, P=0.000) (Table 1).
Full table
Heel congestion after blood collection
There were 6 cases of heel congestion in the control group, and the incidence of heel congestion after blood sampling was 12.5%. There were no cases of heel congestion in the observation group, and the incidence of heel congestion after blood sampling was 0%. Comparing the 2 groups, heel congestion in the observation group was better than that in the control group after blood sampling (χ2=4.444, P=0.035) (Table 2).
Full table
Crying time and bleeding time of newborns
The crying time of the observation group was 45.12±4.26 s and the bleeding time was 2.68±0.24 s. In the control group, the crying time was 69.76±6.57 s and the bleeding time was 4.71±0.82 s. Comparing the 2 groups, the crying time and bleeding time of newborns in the observation group were significantly shorter than those in the control group (t=21.802, t=16.461, respectively; P=0.000, P=0.000, respectively) (Table 3).
Full table
Blood oxygen saturation and heart rate index
The blood oxygen saturation of the observation group was 81.36±2.36 (%) and the heart rate was 145.34±2.30 (times/min). In the control group, the blood oxygen saturation of the control group was 70.43±3.42 (%), and the heart rate was 155.98±1.79 (times/min). Comparing the 2 groups, the blood oxygen saturation of the observation group was higher than that of the control group, and the heart rate index was lower than that of the control group (t=18.224, t=25.293, respectively; P=0.000, P=0.000, respectively) (Table 4).
Full table
Pain condition
The scores of facial expression, crying, breathing pattern, upper limb movement, lower limb movement, the state of awakening and the total NIPS score of the observation group were 0.44±0.10 points, 0.41±0.09 points, 0.32±0.08 points, 0.29±0.07 points, 0.43±0.11 points, 0.24±0.05 points. and 2.13±0.25 points, respectively. In the control group, they were 0.76±0.19 points, 1.21±0.55 points, 0.68±0.14 points, 0.55±0.12 points, 0.61±0.13 points, 0.71±0.16 points, and 4.52±0.58 points, respectively. Comparing the 2 groups, the total NIPS score of the observation group was lower than that of the control group (t=26.217, P=0.000) (Table 5).
Discussion
Neonatal heel blood screening refers to the use of rapid and sensitive laboratory methods to screen for genetic metabolic diseases, congenital endocrine abnormalities, and serious genetic diseases in newborns (11,12). Heel blood screening is important for the early diagnosis and treatment of diseases, and effectively avoids irreversible damage to the body’s tissues and organs (13). However, heel blood sampling can cause varying degrees of pain to newborns. Newborns have a longer and stronger perception of pain than adults. When heel blood sampling is carried out, painful stimulation will cause them to cry and twist their bodies, making it difficult to successfully complete blood collection. At the same time, painful stimulation with too frequency and too long time are likely to cause the newborns to experience sleep quality, decreased appetite, or immune function, and affect their normal development (14,15). Newborns are unable to communicate effectively. Through the intervention of EBMs, the newborn can get the comfort of the mother, which can improve the sense of security and comfort of the newborn, thus eliminating the stress response, reducing the stimulation pain, and achieving the effect of pain relief and reducing adverse reactions. It has a good application prospect in relieving the operational pain of the newborn (16).
In the present study, we found that the success rate of 1-time blood collection in the observation group was higher than that in the control group, and the blood collection time was shorter than that in the control group (P<0.05). The results showed that EBMS can increase the success rate of 1-time blood collection and shorten the time-consuming blood collection. EBMS not only provides a familiar and comfortable environment but the newborn also has access to breast milk, which reduces their perception of changes in the surrounding environment as much as possible, and will make blood collection easier for medical staff (3). This could be the reason why EBMS improves the success rate of 1-time blood collection and reduces the blood collection time.
In the present study, heel congestion in the observation group was better than that in the control group (P<0.05). The findings indicated that EBMS can improve heel congestion after blood collection. The main reasons for this are that EMBS provides the newborn with a familiar environment to ensure a stable mood, effectively shortening the time for blood collection and minimizing needle damage to the neonatal subcutaneous blood vessels, thereby avoiding local heel congestion (17).
In the present study, the crying time and bleeding time of newborns in the observation group were significantly shorter than those in the control group (P<0.05). The results showed that EBMS can shorten the crying time and bleeding time of the newborn. The main reasons this are that EBMS can not only provides newborns with a temperature-controlled environment and insulation measures but they also have comfort in their mother’s arms. A mild and good environment can effectively meet the emotional needs of newborns, enabling them to have a calm and happy state, and can ensure the smooth completion of blood collection work, effectively reducing the crying time and bleeding time of newborns (18).
In the present study, the blood oxygen saturation of the observation group was higher than that of the control group, and the heart rate was lower than that of the control group (P<0.05). The results showed that EBMS can effectively increase neonatal blood oxygen saturation, reduce heart rate, and ensure that the 2 indicators are within the normal range. This could be because tryptophan in breast milk can increase the concentration of β-endorphin, and the sweetness of breast milk can activate endogenous opioids. β-endorphin not only has an analgesic effect but can effectively shorten the recovery time of blood oxygen saturation. The pain caused by heel blood sampling increases the heart rate of newborns. The sweetness of breast milk can stimulate the pleasure center of the newborn’s brain, activate endogenous opioids, promote the secretion of 5-hydroxy tryptamine and dopamine, reduce the transmission of pain mediators, and effectively reduce their heart rate (19).
The findings of the present study also indicated that the total NIPS score of the observation group was lower than that of the control group (P<0.05). EBMS was found to significantly reduce the newborn’s NIPS score. The EBMS model can create an environment similar to the uterus for newborns, increase their sense of security, and have a certain sedative effect, reducing their pain. The EBMS model can also increase neural excitement of the newborn through mother-newborn contact, thereby reducing their pain (20). In addition, during breastfeeding, the concentration of β-endorphin in the newborn will increase, effectively reducing pain (21).
Conclusions
EBMS can improve the success rate of 1-time blood collection; shorten the time of blood collection; ensure that blood oxygen saturation and heart rate are at normal values; and effectively reduce the occurrence of heel congestion after blood collection, crying time and bleeding time of newborn heel blood collection, and neonatal pain.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-329
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-329
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-329). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of Haian People’s Hospital [ethics approval number: (2019) KY033] and was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Mothers of every neonate provided informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sok P, Lupo PJ, Richard MA, et al. Utilization of archived neonatal dried blood spots for genome-wide genotyping. PLoS One 2020;15:e0229352 [Crossref] [PubMed]
- van der Burg S, Oerlemans A. Fostering caring relationships: Suggestions to rethink liberal perspectives on the ethics of newborn screening. Bioethics 2018;32:171-83. [Crossref] [PubMed]
- Murphy MSQ, Chakraborty P, Pervin J, et al. Incidental screen positive findings in a prospective cohort study in Matlab, Bangladesh: insights into expanded newborn screening for low-resource settings. Orphanet J Rare Dis 2019;14:25. [Crossref] [PubMed]
- Nazeri P, Shariat M, Mehrabi Y, et al. Is there an association between thyrotropin levels within the normal range and birth growth parameters in full-term newborns. J Pediatr Endocrinol Metab 2018;31:1001-7. [Crossref] [PubMed]
- Rodrigues LP, Tanaka SCSV, Haas VJ, et al. Heel prick test: maternal-fetal conditions that may have an effect on the test results in newborns admitted to the intensive care unit. Rev Bras Ter Intensiva 2019;31:186-92. [Crossref] [PubMed]
- Goel N, Shrestha S, Smith R, et al. Screening for early onset neonatal sepsis: NICE guidance-based practice versus projected application of the Kaiser Permanente sepsis risk calculator in the UK population. Arch Dis Child Fetal Neonatal Ed 2020;105:118-22. [Crossref] [PubMed]
- Ou-Yang MC, Chen IL, Chen CC, et al. Expressed breast milk for procedural pain in preterm neonates: a randomized, double-blind, placebo-controlled trial. Acta Paediatr 2013;102:15-21. [Crossref] [PubMed]
- Diallo DA, Guindo A, Touré BA, et al. Targeted newborn screening for sickle-cell anemia: Sickling test (Emmel test) boundaries in the prenatal assessment in West African area. Rev Epidemiol Sante Publique 2018;66:181-5. [Crossref] [PubMed]
- Ozdogan T, Akman I, Cebeci D, et al. Comparison of two doses of breast milk and sucrose during neonatal heel prick. Pediatr Int 2010;52:175-9. [Crossref] [PubMed]
- Davari S, Borimnejad L, Khosravi S, et al. The effect of the facilitated tucking position on pain intensity during heel stick blood sampling in premature infants: a surprising result. J Matern Fetal Neonatal Med 2019;32:3427-30. [Crossref] [PubMed]
- Moat SJ, Dibden C, Tetlow L, et al. Effect of blood volume on analytical bias in dried blood spots prepared for newborn screening external quality assurance. Bioanalysis 2020;12:99-109. [Crossref] [PubMed]
- McClean S, Baerg K, Smith-Fehr J, et al. Cost savings with transcutaneous screening versus total serum bilirubin measurement for newborn jaundice in hospital and community settings: a cost-minimization analysis. CMAJ Open 2018;6:E285-91. [Crossref] [PubMed]
- Vubil A, Nhachigule C, Loquiha O, et al. Viral load assay performs comparably to early infant diagnosis assay to diagnose infants with HIV in Mozambique: a prospective observational study. J Int AIDS Soc 2020;23:e25422 [Crossref] [PubMed]
- Goodwin S, Supachana N. A safety lancet for neonatal blood spot tests: a design that facilitates pain-free, atraumatic samples. Br J Nurs 2019;28:S24-8. [Crossref] [PubMed]
- Al Juraibah F, Alothaim A, Al Eyaid W, et al. Cord blood versus heel-stick sampling for measuring thyroid stimulating hormone for newborn screening of congenital hypothyroidism. Ann Saudi Med 2019;39:291-4. [Crossref] [PubMed]
- Alvarez OA, Hustace T, Voltaire M, et al. Newborn Screening for Sickle Cell Disease Using Point-of-Care Testing in Low-Income Setting. Pediatrics 2019;144:e20184105 [Crossref] [PubMed]
- Allaf B, Couque N, Montalembert M. Newborn screening of sickle cell disease and management of care. Rev Prat 2019;69:411-6. [PubMed]
- Goto T, Inoue T, Kamiya C, et al. Neonatal pain response to automatic lancet versus needle heel-prick blood sampling: A prospective randomized controlled clinical trial. Pediatr Int 2020;62:357-62. [Crossref] [PubMed]
- Bhattacharya M, Bhaumik P, Kumar-Dey S. Telomere length comparison between oral cells and blood cells among neonates. Turk J Pediatr 2019;61:520-4. [Crossref] [PubMed]
- Aysola AE, Duque MA, Williams P, et al. Comparison of heel stick sample with placental blood sample for pretransfusion testing. Transfusion 2018;58:2227-31. [Crossref] [PubMed]
- Whittaker GA, Munteanu SE, Menz HB, et al. Corticosteroid injection for plantar heel pain: a systematic review and meta-analysis. BMC Musculoskelet Disord 2019;20:378. [Crossref] [PubMed]
(English Language Editor: R. Scott)



