
Clinical value of endobronchial ultrasound-guided aspiration and local isoniazid injection in the treatment of mediastinal tuberculous lymphadenitis
Introduction
Mediastinal lymph nodes are a common target of mycobacterium tuberculosis (MTB), and the upper mediastinal and right hilar lymph nodes are more susceptible to MTB infection. Patients with mediastinal tuberculous lymphadenitis (MTLA) may be symptomatic or asymptomatic, and abnormal findings on chest X-ray might be the unique manifestation (1). The clinical treatment of MTLA has been a challenge in clinical practice. Generally, the treatment of MTLA is long lasting and has no reliable efficacy. Moreover, the enlarged lymph nodes may compress the surround organs, causing corresponding symptoms, which may be life-threatening. The superficial tuberculous lymphadenitis with suppuration is often managed by operative drainage (2), but operative drainage is not applicable in the treatment of MTLA. Traditionally, MTLA with suppuration is managed by systemic chemotherapy and surgical intervention (3), but the surgical treatment is traumatic and costly, and often has some complications. Thus, clinicians have explored an efficient and simple method for the treatment of MTLA.
The endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) is an endoscopic technique with the combination of ultrasound and electronic bronchoscope. EBUS-TBNA is often used to explore the enlarged lymph nodes in the mediastinum and around the hilus of the lung, trachea and bronchus, and ultrasound-guided puncture can also be done with this technique. It has been reported that EBUS-TBNA can be employed for the diagnosis and staging of lung cancer (4-6). In recent years, favorable results have been achieved in the diagnosis of sarcoidosis and MTLA with EBUS-TBNA (7-9). In the past few years, we conducted EBUS-TBNA in some patients with refractory MTLA for the purulence aspiration and local isoniazid injection. Our experience showed the symptoms were significantly improved. This study was conducted to investigate the clinical value of EBUS-TBNA for purulence aspiration and local isoniazid injection in the management of refractory MTLA. Our results showed lymph node puncture, purulence aspiration and subsequent local isoniazid injection treatment were safe and reliable with few adverse reactions. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1809).
Methods
Study design and ethics
This was a single-center, retrospective clinical study. A total of 92 patients with suppurative mediastinal tuberculous lymphadenitis who met the inclusion criteria and received regular anti-tuberculosis treatment with complete clinical data between January 2015 and December 2018 were included into present study. They were divided into systemic chemotherapy (CT) group (n=49) and interventional therapy (IT) group (n=43) according to their treatment. In the CT group, patients received systemic chemotherapy with anti-tuberculosis drugs; in the IT group, patients received EBUS-TBNA for mediastinal lymph node aspiration and local isoniazid injection besides systemic chemotherapy. The inclusion and exclusion criteria were described in the following section. Finally, 70 patients were included for final analysis with 35 patients in each group. There were no significant differences in the gender, age, course of disease, body mass index (BMI), clinical symptoms, laboratory findings between two groups. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Shanghai Pulmonary Hospital (No. K20-009). Because this was retrospective study, informed consent for inclusion was waived (Figure 1).
Inclusion and exclusion criteria
Inclusion criteria were as follows: (I) patients were initially diagnosed with MTLA with or without pulmonary tuberculosis and aged 17–70 years; (II) poor treatment response after one month of chemotherapy as defined by: mediastinal lymph node liquefaction; largest diameter of liquefaction on enhanced chest CT >1.5 cm, or maximum diameter <1.5 cm, but presence of persistent clinical symptoms such as fever >38.5 °C or dyspnea; (III) patients were tolerant to EBUS-TBNA and had complete medical record; (IV) patients completed the anti-tuberculosis treatment.
Exclusion criteria were as follows: (I) drug sensitivity examinations showed MTB was resistant to any first-line anti-tuberculosis drug; (II) patients had a history of allergy to the selected therapeutic drug; (III) patients were pregnant or breast-feeding; (IV) patients had other lung diseases such as lung tumor, and pneumoconiosis; (V) patients had concomitant diabetes mellitus or immune diseases.
Instruments and materials
EBUS-TBNA: CV-290 endoscope image processing device (Olympus, Japan), CLV-290SL endoscope xenon cold light (Olympus, Japan), EU-ME2 PREMIER PLUS Ultrasonic endoscope image processing device (Olympus, Japan), BF-UC206FW ultrasound bronchoscope (Olympus, Japan) and NA-201SX-4021 needle (Olympus, Japan) were used in the present study.
Chemotherapy
All the patients were treated with directly observed treatment (DOT) of short course and received anti-tuberculosis treatment with 3HREZ/9HRE protocol (H: isoniazid, R: rifampicin, E: ethambutol, Z: pyrazinamide) for 12 months (10).
Interventional therapy
In the IT group, patients received EBUS-TBNA for purulence aspiration and local isoniazid injection (once every 2–3 weeks). The dose of isoniazid was determined based on the size of lymph node abscess: 0.3 g of isoniazid was injected when the abscess was <1 cm in maximum diameter; 0.45 g of isoniazid was injected when the abscess was 1–2 cm; 0.6 g of isoniazid was injected when the abscess was >2 cm. Local treatment lasted until purulence aspiration was infeasible.
Procedures for interventional therapy
Before the operation, patients received food and water deprivation for 4 h. Local anesthesia was done with 2% lidocaine (total 10 mL, Shanghai Pharmaceutical Group Co., Ltd. Xinyi Pharmaceutical General Factory). The bronchoscope was inserted through the nose, and the lymph nodes and surrounding blood vessels were observed in the ultrasound mode. The lymph nodes were grouped according to the criteria in the American Thoracic Society (ATS) map of region pulmonary nodes. The size, boundary, sonogram, and blood flow of target lymph nodes were recorded on the ultrasound image. Once the extent and direction of the abscess were confirmed, puncture was performed under real-time ultrasound guidance (Figure 2). The pus was aspired as much as possible by negative pressure suction (20 mL negative air pressure). The pus was subjected to pathological and bacteriological examinations. Then, the needle was gradually withdrawn, and isoniazid was injected slowly.

Observations
During the anti-tuberculosis treatment, all patients were followed up regularly in accordance with the Chinese Guidelines for the Tuberculosis Treatment. The medical record was carefully reviewed, the course of disease, imaging findings, symptoms and adverse effects were recorded, and the findings related to recurrence of tuberculosis within 2 years after therapy discontinuation were also recorded. The changes in the mediastinal lymph nodes and lung lesions were assessed by 2 or more radiologists after enhanced chest CT.
Size of mediastinal lymph nodes
The maximum diameter of mediastinal lymph nodes was measured according to the chest enhanced CT at the end of treatment, and the changes were assessed based on the mediastinal lymph nodes: (I) complete remission: lymph node enlargement was absent or the enlarged lymph nodes were ≤5 mm in diameter; (II) remission: the size of enlarged lymph nodes was reduced by >1/2 or the enlarged lymph nodes were ≤10 mm in diameter; (III) stability: the size of enlarged lymph nodes was reduced by <1/2, and the enlarged lymph nodes were >10 mm in diameter; (IV) deterioration: the lymph nodes continued to enlarge or presence of new enlarged lymph nodes. The lymph node outcomes were recorded and compared between two groups.
Bacterial examination
The sputum was collected at 2, 6 and 12 months and processed for acid resistant smear and mycobacterium culture. The time to negative results in sputum culture was recorded and compared between two groups.
Changes of lung lesion
The recovery of lung lesion was assessed at the end of the treatment.
Improvement of symptoms
The symptoms were assessed according to the criteria in supplementary Table 1. The time to improvement of clinical symptoms was recorded and compared between two groups.
Full table
Statistical analysis
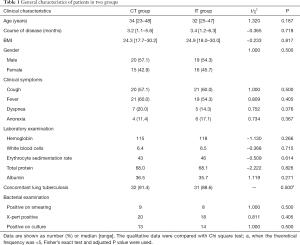
Patients lost to follow up or with incomplete data were not included in final analysis. SPSS version 19.0 was used for statistical analysis. The quantitative data with normal distribution are expressed as mean ± standard deviation or median (interquartile range). The t test was used for comparisons between groups. A value of P<0.05 was considered statistically significant. The qualitative data are expressed as “number” or “rate”, and compared with Chi square test (Fisher’s exact test was used if the theoretical frequency was less than 5). A value of P<0.05 was considered statistically significant. The statistical ratio of patients in different treatment groups was 1:1. The demographics are shown in Table 1. The recovery rate of mediastinal lymph nodes was calculated and compared between two groups, followed by calculation of OR and 95% CI.
Results
Baseline characteristics
The baseline characteristics of patients included are shown in Table 1. There were no marked differences in the age, course of disease, BMI, gender and main clinical symptoms between two groups. In addition, the laboratory findings and results from bacterial examinations were also comparable between groups.
Therapeutic effectiveness
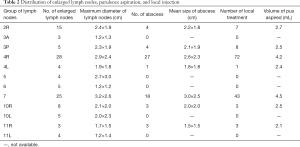
Treatments and lymph node size
In the IT group, the incidences of multiple mediastinal lymphadenopathy and mediastinal lymph node suppuration were 82.9% (29/35) and 77.1% (27/35), respectively. In the CT group, the incidences of multiple mediastinal lymphadenopathy and mediastinal lymph node suppuration were 85.7% (30/35) and 77.1% (27/35), respectively. As shown in Table 2, purulence aspiration and local injection were done 137 times in the IT group. The most common sites of puncture were 4R (52.6%) and 7 groups of lymph nodes (31.4%). The median number of local treatment was 3 times, and the median duration of local injection was 29 days. At the end of treatment, the incidence of complete remission was 88.6% (31/35) and 57.1% (20/35) in the IT group and CT group, respectively, and there was significant difference between two groups (χ2=8.741, P<0.05; OR =5.813, 95% CI: 1.686–20.044).
Full table
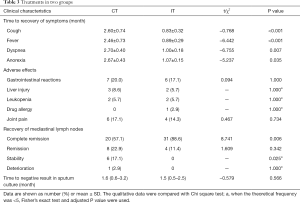
Clinical symptoms
As shown in Table 3, the time to recovery of clinical symptoms in the IT group was significantly shorter than in the CT group.
Full table
Safety analysis
As shown in Table 3, there was no marked difference in the incidence of main adverse effects. Drug-induced liver injury was observed in 1 patient in each group, and then rifampicin was replaced with rifampin. All the procedures were done under local anesthesia. Small blood loss was observed at the site of puncture in 2 patients, but other serious complications (such as fever, pneumothorax, mediastinal emphysema, injury to major vessels) were not observed. After treatment, patients received follow up for 2 years, and recurrence was not noted.
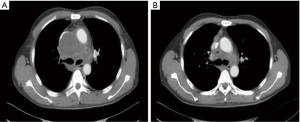
Representative cases
As shown in Figure 3, 4R lymph nodes became significantly enlarged and compressed the superior vena cava. Thus, EBUS-TBNA was performed for purulence aspiration in 4R lymph nodes, followed by local isoniazid injection (4 times). Chest CT 3 months later showed significant reduction of lymph node size.
Discussion
MTLA is a chronic disease caused by MTB invading the mediastinal lymph nodes. Previously, MTLA was mainly found in children (1,11), but the incidence of MTLA in adults is increasing in recent years (12,13). MTLA can affect all groups of lymph nodes in the mediastinum. The lymph nodes may become smaller in some patients after systemic anti-tuberculosis treatment, but other patients are non-responsive to systemic anti-tuberculosis treatment and the lymph nodes continue to enlarge and compress surrounding organs. Moreover, the tuberculous lymph nodes may even rupture into the tracheobronchial lumen and lungs, causing obstructive pneumonia or atelectasis. Advanced tuberculous lymph nodes with abscess often fuse, the extent of caseous necrosis increases to form an abscess cavity, and the lesion may even penetrate the surrounding soft tissues. If the necrotic tissues are not removed in time, they may invade the heart, aorta and esophagus, form fistulas, and cause esophageal mediastinal fistula (14), thyroid tuberculosis (15), esophageal fistula (16,17), and bronchial lymph node pericardial fistula (18), which are usually life-threatening (19). In addition to systemic treatment, the MTLA is traditionally managed by surgery. However, the surgical treatment may cause trauma, has some complications (3) and is often costly.
Mehta et al. (20) reported the diagnostic yield of conventional TBNA was 347/400 (86.75%) (tuberculosis: 43%; sarcoidosis: 25.5%; malignancy: 18.25%). As compared to TBNA, the location, size, and blood flow of lymph nodes can be observed in a real time manner on EBUS-TBNA. In a study of Lin et al. (21), a total of 240 patients received EBUS-TBNA, and finally 21 patients were diagnosed with MTLA. When combined with histologic examination and traditional microbiologic examinations, the diagnostic accuracy of EBUS-TBNA may reach 57.1%. If TB-PCR is also utilized, the diagnostic accuracy will significantly increase to 71.4%. In addition, this technique is more accurate and has fewer side effects when the lymph nodes are small and difficult to puncture. The uneven echo and characteristics of necrosis in the lymph nodes on EBUS are the specific signs of MTLA (22). In the present study, EBUS-TBNA was used to increase the accurate rate of lymph node puncture based on the location of abscess on ultrasonography. In addition, the purulence aspiration and lymph node size can be observed in a real time manner, which is helpful to adjust the location of the needle. The real time puncture can control the depth of needle insertion and achieve multi-point injection, which ensure that the drug can be evenly distributed in the lymph nodes, improving the therapeutic efficacy.
Our results showed at the end of treatment, the rate of complete remission was 88.6% in the IT group and 57.1% in the CT group, showing marked difference between two groups (χ2=8.741, P<0.05). This suggests that the outcome of mediastinal lymph nodes in the IT group was significantly better than in the CT group. The common symptoms of MTLA patients were cough, fever, dyspnea and anorexia, and the time to recovery of these symptoms in the IT group was 0.83±0.32, 0.89±0.29, 1.00±0.18 and 1.07±0.15 months, respectively, which were markedly shorter than in the CT group (2.60±0.74, 2.46±0.73, 2.70±0.40 and 2.67±0.43 months). This indicates that IT may benefit the recovery of clinical symptoms in MTLA patients as compared to CT. The main adverse reactions of anti-tuberculosis treatment included gastrointestinal reactions, liver injury, leukopenia, drug allergies and joint pain. However, there was no marked difference in the incidence of adverse reactions between IT group and CT group.
An et al. (23) found the lymph nodes became significantly smaller after local treatment in some patients with MTLA. However, the response to anti-tuberculosis treatment is often relatively long in patients with MTLA, which may be ascribed to the complete capsule of lymph nodes and low blood flow in the lymph nodes. In addition, the lymphatic transportation is blocked after lymph node enlargement. Thus, the effective drug concentration is very low in the lymph nodes. Moreover, the excretion and absorption of necrotic tissues are usually difficult. Therefore, the systemic chemotherapy frequently achieves a poor efficacy. In China, systemic chemotherapy combined with local drug injection has been used for a long time in the treatment of cervical tuberculous lymphadenitis (24). This not only reduces the size of lymph nodes, but also improves the clinical efficacy and reduces the recurrence rate. In recent years, bronchoscopic cryotherapy combined with drugs infusion was employed in the treatment of transbronchial tuberculosis in addition to systemic anti-tuberculosis treatment, achieving favorable efficacy (25). In the present study, MTLA, especially the refractory or suppurative MTLA, patients were recruited, and EBUS-TBNA was performed for purulence aspiration and local isoniazid injection besides systemic anti-tuberculosis treatment. The therapeutic efficacy was assessed.
Our results show that purulence aspiration and local isoniazid injection on EBUS-TBNA in the presence of systemic anti-tuberculosis treatment can not only improve the rate of complete remission, but also alleviate the clinical symptoms of refractory MTLA. Moreover, it is safe and reliable, and has fewer adverse reactions. The complete capsule of mediastinal lymph nodes and low internal blood flow reduce the amount of drugs entering the lymph nodes in the systemic anti-tuberculosis treatment, and thus anti-bacterial effect is compromised, which lowers the therapeutic efficacy. On EBUS, the lesioned lymph nodes can be accurately punctured via adjusting the position and angle of needle, the pus is aspired to remove necrotic tissues as much as possible. Then, the anti-tuberculosis drug is injected to the lymph nodes at multiple sites, which assure the concentration of anti-tuberculosis drug in the lymph nodes. This technique promotes the recovery of tuberculous lymph nodes and also alleviate the compression of lymph nodes on surrounding tissues.
In this study, anti-tuberculosis drug isoniazid was locally injected in the lymph nodes of patients with refractory MTLA according to the opinions from some experts on the anti-tuberculosis drugs used in the airway. This drug has been widely used in clinical treatment of tuberculosis with few adverse reactions and definite effectiveness. It can not only be systematically used, but also locally employed in the tracheobronchial lesions (25). In addition, atomization of isoniazid and injection of isoniazid into the superficial lymph nodes have also been reported (26,27).
Our results showed lymph node puncture, purulence aspiration and subsequent local isoniazid injection treatment are safe and reliable with favorable short-term effectiveness and few adverse reactions. Of note, this study was a single-center study, and the sample size was small. In the future, more multi-center prospective studies are needed to further confirm our findings, standardize the therapeutic protocol and facilitate the application of this treatment.
Acknowledgments
Funding: This study was funded by the Shanghai Clinical Research Center for infectious disease (tuberculosis) (19MC1910800).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1809
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1809
Peer Review File: Available at http://dx.doi.org/10.21037/apm-20-1809
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1809). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Ethics Committee of Shanghai Pulmonary Hospital (No. K20-009) and informed consent for inclusion was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jacob B, Parsa R, Frizzell R, et al. Mediastinal tuberculosis in Bradford, United Kingdom: the role of mediastinoscopy. Int J Tuberc Lung Dis 2011;15:240-5. i. [PubMed]
- Li Z, Li J, Liao X, et al. The surgical options of cervical tuberculous lymphadenitis. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2015;29:1190-3, 1212.
- Zuo T, Gong FY, Chen BJ, et al. Video-assisted thoracoscopic surgery for the treatment of mediastinal lymph node tuberculous abscesses. J Huazhong Univ Sci Technolog Med Sci 2017;37:849-54. [PubMed]
- Fernández-Villar A, Mouronte-Roibas C, Botana-Rial M, et al. Ten Years of Linear Endobronchial Ultrasound: Evidence of Efficacy, Safety and Cost-effectiveness. Arch Bronconeumol 2016;52:96-102. [Crossref] [PubMed]
- Vaidya PJ, Kate AH, Yasufuku K, et al. Endobronchial ultrasound-guided transbronchial needle aspiration in lung cancer diagnosis and staging. Expert Rev Respir Med 2015;9:45-53. [Crossref] [PubMed]
- Žemaitis M, Musteikiene G, Miliauskas S, et al. Diagnostic Yield of Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration Cytological Smears and Cell Blocks: A Single-Institution Experience. Medicina (Kaunas) 2018;54:19. [Crossref] [PubMed]
- Erer OF, Erol S, Anar C, et al. The diagnostic accuracy of endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) in mediastinal tuberculous lymphadenitis. Turk J Med Sci 2017;47:1874-9. [Crossref] [PubMed]
- Prasad KT, Muthu V, Sehgal IS, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in HIV-infected patients with undiagnosed intrathoracic lymphadenopathy. Lung India 2018;35:379-83. [Crossref] [PubMed]
- Senturk A, Arguder E, Hezer H, et al. Rapid diagnosis of mediastinal tuberculosis with polymerase chain reaction evaluation of aspirated material taken by endobronchial ultrasound-guided transbronchial needle aspiration. J Investig Med 2014;62:885-9. [Crossref] [PubMed]
- Minakuchi M, Tanaka E, Inoue T, et al. An adult case of cervico-mediastinal lymph nodes tuberculosis followed by the development of pulmonary lesions during the treatment with antituberculous drugs. Kekkaku 2005;80:19-23. [PubMed]
- . efremova SN, Dovgaliuk IF, Sakharova I. Estimation of the specific sensitization in a child and other immunological parameters in tuberculosis of intrathoracic lymph nodes during therapy. Probl Tuberk Bolezn Legk 2007;22-5. [PubMed]
- Chhajed PN, Vaidya PJ, Mandovra NP, et al. EBUS-TBNA in the rapid microbiological diagnosis of drug-resistant mediastinal tuberculous lymphadenopathy. ERJ Open Res 2019;5:00008-2019 [Crossref] [PubMed]
- Dhamija A, Ganga VB, Guliani A, et al. Endobronchial ultrasound for tubercular mediastinal adenopathy and its comparison with traditional tools. Int J Tuberc Lung Dis 2019;23:907-12. [Crossref] [PubMed]
- Ko Y, Lee HY, Lee YS, et al. Esophagomediastinal Fistula Secondary to Multidrug-resistant Tuberculous Mediastinal Lymphadenitis. Internal Medicine 2014;53:1819-24. [Crossref] [PubMed]
- Chandanwale SS, Buch AC, Vimal SS, et al. Thyroid tuberculosis: presenting symptom of mediastinal tuberculous lymphadenitis--an unusual case. Indian J Tuberc 2014;61:84-7. [PubMed]
- Liao LY, Wu H, Zhang NF, et al. Bronchoesophageal fistula secondary to mediastinal lymph node tuberculosis: a case report and review of the literature. Zhonghua Jie He He Hu Xi Za Zhi 2013;36:829-932. [PubMed]
- Madan K, Venkatnarayan K. Successful medical management of tuberculous broncho-oesophageal fistula. BMJ Case Rep 2014;2014:bcr2013202560 [Crossref] [PubMed]
- Lee S, Lee K, Ko JK, et al. Polymicrobial Purulent Pericarditis Probably caused by a Broncho-Lymph Node-Pericardial Fistula in a Patient with Tuberculous Lymphadenitis. Infect Chemother 2015;47:261-7. [Crossref] [PubMed]
- Bae K, Jeon KN, Kim HC, et al. Tuberculosis presenting as isolated bronchonodal fistula in a patient with systemic lupus erythematosus: Case report. Medicine (Baltimore) 2017;96:e8764 [Crossref] [PubMed]
- Mehta RM, Singla A, Balaji AL, et al. Conventional Transbronchial Needle Aspiration: The Original Guard Who Still Has a Role in Mediastinal Lymph Node Sampling. J Bronchology Interv Pulmonol 2017;24:290-5. [Crossref] [PubMed]
- Lin CK, Keng LT, Lim CK, et al. Diagnosis of mediastinal tuberculous lymphadenitis using endobronchial ultrasound-guided transbronchial needle aspiration with rinse fluid polymerase chain reaction. J Formos Med Assoc 2020;119:509-15. [Crossref] [PubMed]
- Erol S, Anar C, Erer OF, et al. The Contribution of Ultrasonographic Characteristics of Mediastinal Lymph Nodes on Differential Diagnosis of Tuberculous Lymphadenitis from Sarcoidosis. Tanaffos 2018;17:250-6. [PubMed]
- An H, Wang Z, Chen H, et al. Clinical efficacy of short-course chemotherapy combined with topical injection therapy in treatment of superficial lymph node tuberculosis. Oncotarget 2017;8:109889-93. [Crossref] [PubMed]
- Qin L, Ding WM, Zhang JY, et al. Efficacy and safety of cryotherapy combined with balloon dilatation through electronic bronchoscope in the management of airway occlusion caused by scar stenosis type of tracheobronchial tuberculosis. Zhonghua Jie He He Hu Xi Za Zhi 2018;41:857-62. [PubMed]
- Zhang JX, Bai C, Huang HD, et al. Bronchoscopic cryotherapy combined with drugs infusion in the treatment of transbronchial tuberculous. Zhonghua Jie He He Hu Xi Za Zhi 2011;34:898-903. [PubMed]
- Sibum I, Hagedoorn P, Frijlink HW, et al. Characterization and Formulation of Isoniazid for High-Dose Dry Powder Inhalation. Pharmaceutics 2019;11:233. [Crossref] [PubMed]
- Wyszogrodzka-Gaweł G, Dorozynski P, Giovagnoli S, et al. An Inhalable Theranostic System for Local Tuberculosis Treatment Containing an Isoniazid Loaded Metal Organic Framework Fe-MIL-101-NH2-From Raw MOF to Drug Delivery System. Pharmaceutics 2019;11:687. [Crossref] [PubMed]



