
Effects of off-pump coronary artery bypass graft on the clinical efficacy, surgical indicators, and cardiac function of patients with coronary heart disease
Introduction
The term coronary heart disease (CHD) collectively refers to the status of narrowing or obstruction caused by vascular lumen coronary artery atherosclerosis, or changes in coronary artery function that causes coronary artery spasm, myocardial ischemia, and hypoxia (1). In recent years, along with the general trend of lifestyle change, the incidence of CHD has increased significantly. A large number of studies have found that CHD can cause a variety of complications. If not treated in time, CHD will cause a variety of organ damage or failure, and seriously threaten the life of patients (2).
With the continuous development of medical technology, coronary artery bypass graft has been widely applied in clinical practice. Coronary artery bypass surgery is often divided into 2 different intervention methods, including extracorporeal coronary artery bypass graft and off-pulmonary bypass graft. Studies have shown that extracorporeal coronary artery bypass graft can easily induce systemic inflammatory response syndrome, and cause tissue and organ damage, thereby diminishing the therapeutic effect; while off-pump coronary artery bypass graft can effectively avoid myocardial ischemia and hypoxia or perfusion re-injury, and has the advantages of less trauma, fast recovery, and minimal complications (3). In this study, patients with CHD treated in our hospital were administrated with extracorporeal coronary artery bypass graft surgery and off-pulmonary bypass coronary artery bypass surgery, respectively. The the clinical efficacy, surgical indicators, and cardiac function of the 2 different surgical options for CHD patients were analyzed. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2560).
Methods
General information
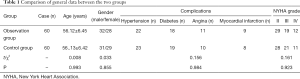
A total of 120 patients with CHD undergoing surgical treatment in our hospital from May 2017 to May 2020 were randomly selected as the research cohort, and the clinical data of these participants were studied. The participants were divided into 2 groups according to their different surgical methods: the observation group included participants treated with off-pump coronary artery bypass graft, and participants in the control group were treated with extracorporeal coronary artery bypass graft. There were 60 cases in each group. The inclusion criteria were as follows: (I) patients were diagnosed with CHD by clinical laboratory, imaging, and other related examinations; (II) patients with complete clinical data; (III) patients with no surgical contraindications; (IV) patients with no mental, cognitive, or communication disorders; (V) patients with no coagulation dysfunction. The exclusion criteria for participation were as follows: (I) patients were intolerant to the surgical treatment or did not meet the indications for this operation; (II) patients with serious diseases of vital organs such as the liver and heart; (III) patients lacking laboratory test diagnosis or those who withdrew from treatment midway. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Second Hospital of Hebei Medical University (No. 2020-P045). Individual consent for this retrospective analysis was waived. Comparison of the general data showed no significant difference in the general information between participants in the 2 groups of (P>0.05, Table 1).
Full table
Surgical methods
Participants in both groups underwent complete preoperative examinations, and the surgeries were performed by experienced physicians with experience above the director level.
Participants in the 2 groups were given intravenous inhalation combined anesthesia, with tracheal intubation in the supine position. For participants in the control group, a midline sternal incision was made, and the vein was heparinized throughout the body. The activated clotting time was maintained for 275 seconds (up and down for no more than 25 seconds). The pericardial traction line was placed, the coronary artery branches were exposed, the target blood vessel was fixed, and then the cardiopulmonary bypass coronary artery bypass graft was performed with the heart beating normally. The coronary artery was anastomosed with the internal mammary artery, the aortic wall was clamped, the outer membrane of the aorta was opened and perforated, and anastomosis was performed at the venous bridge and the proximal end of the ascending aorta. In the observation group, an intra-aortic balloon counterpulsation was inserted through femoral artery puncture, the catheter position was determined by X-ray, heparin was used for anticoagulation, and the activated clotting time was maintained for 160–200 seconds. The intra-aortic balloon counterpulsation was not removed until the circulation was stable, and the puncture site was bound up with pressure for 20 minutes.
Observation indicators and judgment standards
The findings of comparison of clinical efficacy between the 2 groups of patients (4) were categorized as follows: significantly effective, the patients did not have palpitations, chest pain, vomiting or other related clinical symptoms after treatment, and the degree of improvement in CHD was grade II or above; effective, the clinical symptoms such as palpitations, chest pain, and vomiting were alleviated after treatment compared to those before treatment, and the degree of improvement of CHD was grade I; not effective, the relevant clinical symptoms of patient still existed after the treatment.
The total effective rate = (significantly effective case + effective cases)/total number of cases × 100%
We conducted comparison of the relevant surgical indicators of the 2 participant groups, including intraoperative blood loss, intraoperative blood transfusion, operation time, and hospital stay.
Comparison of cardiac function of participants in the 2 groups was performed before and after treatment. The cardiac function was detected by echocardiography, and the cardiac index (CI), ejection fraction (EF), stroke volume (SV), and cardiac output (CO) of the participants were detected by professionals.
The myocardial injury of the 2 groups was compared: 4 mL of arterial blood was collected at four time points including before and immediately after surgery, 6 h and 24 h after surgery, then without any anticoagulant, blood was centrifuged for 15 min (3,000 r/min). And then the serum samples were collected for examination. The activity of creatine kinase-MB (CK-MB) was measured using OlymPus AUl000 (OlymPus, Japan). The content of cardiac troponin I (cTnI) was determined by ELISA. The degree of cardiac autonomic nerve imbalance in the 2 groups was compared. The American HP Holter heart rate variability (HRV) was used for analysis to detect the supervised distributed neural networks (SDNN), total power (TP), low frequency (LF) power and high frequency (HF) power, and total heart rate spectrum before and after treatment.
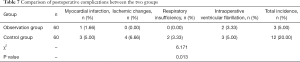
Comparison of complications in the 2 groups after treatment was conducted, including myocardial infarction, ischemic changes, respiratory insufficiency, intraoperative ventricular fibrillation, and some other complications.
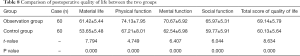
Comparison was made of postoperative quality of life between the 2 groups. The postoperative quality of life of participants were measured using a questionnaire survey according to the Comprehensive Quality of Life Assessment Scale (GQOLI-74) (5). There were 4 dimensions including material life, physical function, mental function, and social function. The higher the score, the better the quality of life.
Statistical analysis
All data were statistically analyzed using the software SPSS version 22.0 (IBM, Armonk, New York, USA). The measurement data were described as mean ± standard deviation (
Results
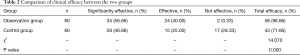
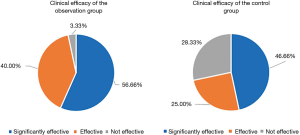
Comparison of the clinical efficacy of patients in the two groups
The total effective rate of the observation group was significantly higher than that of the control group (96.66% vs. 71.66%, P<0.05) (Table 2, Figure 1).
Full table
Comparison of the relevant surgical indicators of patients in the two groups
The relevant surgical indicators including the amount of intraoperative blood loss, operation time, intraoperative blood transfusion, and hospital stay in the observation group were significantly better than those in the control group. The comparison between the 2 groups was statistically significant (P<0.05, Table 3).
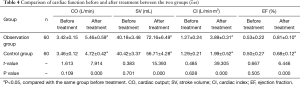
Comparison of the heart function of the two groups before and after treatment
There was no significant difference in cardiac function between the observation group and the control group before treatment (P>0.05). while after treatment, the CO, SV, CI, and EF levels of the observation group and control group were all higher than those before treatment, especially in the observation group (P<0.05, Table 4).
Full table
Comparison of myocardial injury of patients in the two groups
Levels of CK-MB and cTnI were significantly increased in both groups at each time point after surgery compared with that before operation, but which in the observation group were significantly lower than that in the control group at each time point after operation (P<0.05, Table 5).
Comparison of the degree of cardiac autonomic nerve imbalance between the two groups
There was no significant difference in cardiac autonomic nerve index between the two groups before treatment (P>0.05). After treatment, SDNN, LF, HF and TP in the two groups were all increased compared with those before treatment, which was significant in the observation group (P<0.05, Table 6).
Comparison of postoperative complications in the two groups
There were significantly fewer participants with complications such as myocardial infarction, ischemic changes, respiratory insufficiency, and intraoperative ventricular fibrillation in the observation group than in the control group (P<0.05, Table 7).
Full table
Comparison of the quality of life between the two groups one year after surgery
The score of the quality of life in the observation group was (69.14±5.79) points, which was significantly higher than that in the control group (60.13±5.64) points (P<0.05, Table 8).
Full table
Discussion
As a common clinical cardiovascular disease, CHD results from the combination of abnormal lipid metabolism and blood excessive lipid deposits on the arterial intima, white plaques, arterial stenosis, obstruction of blood flow, cardiac ischemia, and angina pectoris. Prolongation of CHD will cause heart rupture and ventricular embolism, endangering the life of the patient (6). Patients with CHD show the characteristics of high morbidity, high progression rate, and high mortality. Therefore, it is of great importance that patients receive timely and effective treatment (7).
Coronary artery bypass surgery is an effective way to treat CHD in clinical practice. The purpose of the operation is to replace the obstructed frontal coronary artery, which could improve the blood supply of the myocardium and promote patient recovery (8). Cardiopulmonary bypass coronary artery bypass graft requires the body to remain in a state of shock, and then the cardiopulmonary bypass is performed for related interventions, which has shown a certain clinical effect (9). However, Borde et al. (10) found that cardiopulmonary bypass coronary artery bypass graft causes a certain degree of damage to the patient’s body. When the body is in a state of shock, inflammation is easily induced, as are symptoms such as vasoconstriction and thrombocytopenia. Conversely, the off-pump coronary artery bypass graft has no special requirements for the patient and the state of the body. Off-pump coronary artery bypass graft surgery can be carried out while maintaining the patient’s normal physiological state, thus avoiding myocardial ischemia and reperfusion injury. In addition, during the operation, the doctor adopts the aortic anastomosis first, followed by adopting the coronary anastomosis, which can recover the blood supply of the ischemic myocardium as soon as possible, minimize the movement of the heart, and also increase the safety of the operation (11,12). Ozsin et al. (13) performed surgical treatment on 100 patients with CHD and found that those treated with off-pump coronary artery bypass graft showed a significant clinical efficacy. In this study, the results showed that the clinical efficacy of the observation group was significantly better than that of the control group, and the incidence of complications was lower in the observation group. These results are consistent with the study of Zheng et al. (14), which indicated that off-pump coronary artery bypass graft has better clinical efficacy and higher safety in the treatment of patients with CHD. In addition, by comparing the surgical indications of the 2 groups of participants, we found that the observation group was significantly better than the control group in terms of intraoperative blood loss, operation time, intraoperative blood transfusion, and hospitalization time. This was because during the operation of off-pump coronary artery bypass graft, the incision is minimally invasive, and the heart stabilization device is used to directly bridge the beating heart to shorten the operation time. Besides, the small dose of heparin used during the operation can effectively reduce the amount of intraoperative blood loss, reduce the amount of blood transfusion, and facilitate postoperative recovery (15).
As an effective indicator of cardiovascular disease, cardiac function examination is of great significance for assessing the progress of CHD patients. Among the measurements of cardiac function, EF is a reliable indicator reflecting the systolic function of the left ventricle and is closely related to the prognosis of heart disease, because it has the advantages of slight affection from the left ventricular preload, high accuracy, and strong reproducibility. The CO is an important indicator in evaluating the efficiency of the circulatory system; when the level of CO decreases, it indicates that cardiogenic shock will occur. The reference indicators CI and SV are important for reflecting heart disease, and play important roles in the reflection of the heart condition (16,17). Relevant studies have shown that the heart structure of patients with CHD changes, which will cause hypofunction of the heart. Among them, 69% of patients have diastolic dysfunction, predominantly caused by changes in hemodynamics due to hypertension and retention of water and sodium, which causes changes in myocardial hypertrophy, decrease of left ventricular filling and diastolic compliance (18). In this study, CHD patients who underwent different surgical treatments all had significantly increased levels of CO, SV, CI, and EF after treatment; the significance was higher in the observation group, indicating that off-pump coronary artery bypass graft surgery has an important role in improving patients’ cardiac function. Compared with the control group, cTnI and CK-MB in the observation group were significantly reduced at each time point after surgery, indicating that compared with the control group, the myocardial injury in the observation group was reduced, as well as the production of oxygen free radicals, thus playing a certain degree of myocardial protection effect. The results of comparing the quality of life scores one year after surgery in the 2 groups showed an average score of 69.14±5.79 points in the observation group, which was significantly higher than the control group score of 60.13±5.64 points. This difference indicated that the treatment of off-pump coronary artery bypass graft can promote the recovery of patients and improve their quality of life.
The relationship between the cardiac autonomic nervous system and CHD patients has always been one of the hot issues in the field of electrophysiology. The autonomic nerve regulates the electrophysiological activity of the heart through its special conduction pathway and mechanism of action. And the autonomic nerve control imbalance caused by nerve reconstruction and electrical reconstruction in ischemic heart disease are important mechanisms for the occurrence of ventricular arrhythmia (19). HRV is currently recognized as the best quantitative indicator for determining neural activity by heart rate variability. In this study, it is found that off-pump coronary artery bypass grafting is of great significance for regulating autonomic nerve dysfunction. In addition, off-pump coronary artery bypass grafting surgery requires more highly trained surgical operators, and clinicians should continuously strengthen their operational proficiency, and be proficient in surgical methods, indications, and complications of disease, At the same time, in order to ensure the surgery effect, avoid postoperative systemic inflammation and oxidative stress, perioperative protection of lung function should be strengthened in patients with coronary heart disease, such as no smoking, shorten the extracorporeal circulation time as far as possible, application of aprotinin before surgery, and reasonable use of ventilators, strict lung management after surgery, so as to reduce the occurrence of pulmonary complications and ensure the success rate of the operation.
In summary, off-pump coronary artery bypass graft for CHD patients shows a good clinical efficacy, which can significantly improve heart function, cardiac autonomic nerve imbalance state, reduce myocardial injury, decrease the incidence of complications, and improve the quality of life of CHD patients. Therefore, off-pump coronary artery bypass graft is worthy of clinical application. However, the number of patients included in this study was limited, so the experimental results were inevitably biased. As for the specific mechanism of off-pump coronary artery bypass grafting, it is necessary to extend the study time and expand the sample size for further study.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2560
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2560
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2560). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Second Hospital of Hebei Medical University (No. 2020-P045). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bowen FU, Lihong G. Clinical Efficacy of Gelan Xinning Soft Capsule in Treatment of Coronary Heart Disease and Its Effect on Serum ICAM-1 and Ang II. Journal of Liaoning University of Traditional Chinese Medicine 2020;33:21-30.
- Neumann A, Vöhringer L, Fischer J, et al. Off-Pump Coronary Artery Bypass Grafting in Acute Coronary Syndrome: Focus on Safety and Completeness of Revascularization. Thorac Cardiovasc Surg 2020;68:679-86. [PubMed]
- atkovic M, Tutus V, Bilbija I, et al. Long Term Outcomes of The Off-Pump and On-Pump Coronary Artery Bypass Grafting In A High-Volume Center. Sci Rep 2019;9:8567.
- Wang H, Li JJ, et al. Comparison of the effects of different anastomosis method in off-pump coronary artery bypass grafting. Ningxia Medical Journal 2019;27:341-2.
- Park J, Lee JH, Kim KA, et al. Effects of Preoperative Statin on Acute Kidney Injury After Off-Pump Coronary Artery Bypass Grafting. J Am Heart Assoc 2019;8:e010892. [Crossref] [PubMed]
- Xiao L, Huang XS. Clinical Research on the Curative Effect of a Combination Treatment of Off Pump Coronary Artery Bypass Grafting and Novel Mitral Valvuloplasty on Patients with Mild and Moderate Ischemic Mitral Regurgitation. Chinese Journal of Medicinal Guide 2019;16:241-2.
- Gao F, Hu J, Chen XP, et al. Application of Dexmedetomidine Combined With Methoxymine in Off-pump Coronary Artery Bypass Grafting. Chinese Journal of Minimally Invasive Surgery 2019;18:342-6.
- Wang Z, Xia LM, Song K, et al. Impact of discontinuation of aspirin and clopidogrel before off-pump coronary artery bypass grafting on postoperative bleeding and transfusion requirement. Zhonghua Wai Ke Za Zhi 2019;57:187-93. [PubMed]
- Li Z, Fan G, Zheng X, et al. Risk factors and clinical significance of acute kidney injury after on-pump or off-pump coronary artery bypass grafting: a propensity score-matched study. Interact Cardiovasc Thorac Surg 2019;28:893-9. [Crossref] [PubMed]
- Borde D, Joshi P, Joshi S, et al. Changes in Right Ventricular Function After Off-Pump Coronary Artery Bypass Grafting. J Cardiothorac Vasc Anesth 2020;10:413-4. [Crossref] [PubMed]
- Thomson P, Howie K, Mohan ARM, et al. Evaluating Perceptions of Self-efficacy and Quality of Life in Patients Having Coronary Artery Bypass Grafting and Their Family Caregivers. J Cardiovasc Nurs 2019;34:250-7. [Crossref] [PubMed]
- Meng G, Wu W, Feng HH, et al. Prophylactic Use of Intra-aortic Balloon Pump before Off-pump Coronary Artery Bypass Grafting in Patients with Different EuroSCORE. Journal of Medical Research 2019;22:172-4.
- Ozsin KK, Sanri US, Toktas F, et al. Effect of SYNTAX score II on postoperative atrial fibrillation in patients undergoing off-pump coronary artery bypass grafting surgery. The Kuwait medical journal: KMJ: the official journal of the Kuwait Medical Association 2019;51:366-72.
- Zheng TF, Jiang HB, An M, et al. Study on stress response and wake quality in patients of off-pump coronary artery bypass grafting under different anesthesia methods. Chinese Heart Journal 2019;14:371-2.
- Wang YP, Ma J, Dong R, et al. Application of intra-aortic balloon pump in elderly patients undergoing off-pump coronary artery bypass grafting. China Medicine 2019;26:382-6.
- Guan Z, Guan X, Gu K, et al. Short-term outcomes of on- vs off-pump coronary artery bypass grafting in patients with left ventricular dysfunction: a systematic review and meta-analysis. J Cardiothorac Surg 2020;15:84. [Crossref] [PubMed]
- Yang F, Sun ZW. Effects of ANH on hemodynamics, blood components and allogeneic blood volume during off-pump coronary artery bypass grafting. Academic Journal of Chinese PLA Medical School 2019;12:197-201.
- Zhao TF, Wang SY, Zhang CX, et al. Effect of papaverine on instant venous graft in off-pump coronary artery bypass grafting. Journal of Cardiovascular and Pulmonary Diseases 2019;31:672-3.
- Jiang HB, Zhang TF, An M, et al. Effects of different anesthesia agents on MMSE scores and Ramsay scores in patients undergoing off-pump coronary artery bypass grafting surgery. Chinese Heart Journal 2019;14:274-6.
(English Language Editor: J. Jones)





