
Predictive efficacy of weaning index on mechanical ventilation evacuation
Introduction
The evacuation of mechanical ventilation occupies a large part of the time of patients on mechanical ventilation in intensive care units (ICUs). The issue of when to leave and when to remove a ventilator has to be considered even when mechanical ventilation is performed (1). The timely weaning of mechanical ventilation can shorten ICU stay times and reduce complications related to mechanical ventilation. Given that ICU doctors must always consider how to accurately determine the timing of weaning, guidance on weaning parameters is very helpful in ensuring successful weaning.
Many weaning parameters, including the rapid breathing index, maximum inspiratory negative pressure, P0.1/maximum inspiratory pressure (MIP), respiratory rate (RR), tidal volume (Vt), minute ventilation (MV), and compliance, respiratory rate, oxygenation and pressure (CROP), are relatively reliable predictive indexes in weaning guidelines (2). However, the issue of how to improve the accuracy of these parameters and select an available parameter remains elusive. Recently, a new parameter weaning index (WI) (3) was proposed for the rapid shallow breathing index (RSBI) to increase its predictive specificity (4). The following two correction factors were added: (I) elasticity index (EI) = peak inspiratory pressure (PIP)/MIP; and (II) ventilation demand index (VDI) = MV/10. The resultant RSBI × EI × VDI (also called the “weaning index”) was shown to have higher prediction ability than other parameters. As a comprehensive indicator, weaning index (WI) includes compliance of the respiratory system, minute ventilation and rapid shallow breathing index. Multi-angle evaluation of mechanically ventilated patients may increase the success rate of weaning. In the present study, MV was measured in assist/control (A/C) mode. At present, most ventilators do not have A/C mode, and patients are placed in a spontaneous breathing mode when weaning. Thus, whether the measurement of minute ventilation volume (MVV) in spontaneous breathing mode can replace A/C mode needs to be further studied to promote the clinical application of a WI. We present the following article in accordance with the STARD reporting checklist (available at http://dx.doi.org/10.21037/apm-21-105).
Methods
Subjects
Patients were enrolled in this study if they had suffered from respiratory failure (for any reason) and had received mechanical ventilation for a period of more than 48 hours in the ICU of the Fourth Hospital of Hebei Medical University from April 2020 to September 2020. To be eligible to participate in this study, patients had to meet the following inclusion criteria: (I) be aged 18 years or older; (II) have required mechanical ventilation due to respiratory failure (for any reason); (III) have been placed on mechanical ventilation for a period of 48 hours or more. Conversely, patients were excluded from the study if: (I) cachexia was caused by an advanced malignant tumor; (II) the patient had received a tracheotomy; (III) the patient was aged under 18; and/or (IV) the weak breathing or loss of spontaneous breathing was caused by brain damage. In total, 40 patients suffering from respiratory failure (for a variety of reasons) were treated in the ICU of the Fourth Hospital of Hebei Medical University, and received mechanical ventilation for more than 48 hours. Causes of respiratory failure included post-operative pulmonary, thoracic and abdominal infections, and acute exacerbation of chronic obstructive pulmonary disease (AECOPD) (see Table 1). The artificial airway of all patients was established by orotracheal intubation. The patients were allocated to the A/C group or the PSV group according to the MVV measured in the A/C and PSV modes. WI was measured before weaning, and the patients were divided into two groups according to the success or failure of the weaning. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of the Fourth Hospital of Hebei Medical University (No. 2020MEC106) and informed consent was taken from all the patients.
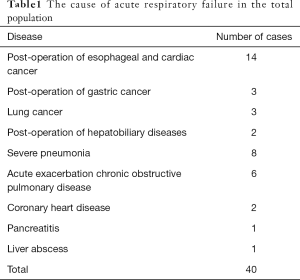
Full table
Measurements
Age, gender, ideal weight, cause of respiratory failure, mechanical ventilation duration, success or failure of weaning, Acute Physiology and Chronic Health Evaluation (APACHE) II score, blood pressure, heart rate, RR, oxygen saturation (SpO2), peak inspiratory pressure, maximum negative inspiratory pressure, MVV, and Vt were monitored and recorded. Vt was measured and RR and WI were observed at 1, 3, and 30 minutes during a spontaneous breathing test. Blood gas parameters were also measured during the spontaneous breathing test.
The patients were randomly divided into either the A/C group or the PSV group. The screening test for weaning was conducted every day. According to the mechanical ventilation guidelines of the Chinese Medical Association (5), the screening test for weaning should be administered when the cause of mechanical ventilation is improved or eliminated. The common screening criteria for a weaning test are: sufficient oxygenation (e.g., PaO2 ≥60 mmHg and FiO2 ≤0.35; PEEP ≤5–10 cmH2O; PaO2/FiO2 ≥150–300); a stable cardiovascular system (e.g., HR ≤140; stable blood pressure; no need for (or minimal) vasoactive drugs; no high fever; no obvious respiratory acidosis; hemoglobin ≥8–10 g/dL; good mental activity (e.g., arousable, GCS ≥13, and no continuous sedative infusion); stable metabolic state (e.g., an acceptable electrolyte level); a subjective clinical evaluation of disease recovery period; the physician’s opinion that weaning is possible; and evaluation of cough ability. All of these parameters were measured before weaning.
The patient’s mechanical ventilation mode was adjusted to A/C mode to measure the peak inspiratory pressure, and volume control ventilation was selected. The ideal weight was calculated according to the ideal weight calculation formula. The Vt was selected as 8 mL/kg, and the mechanical ventilation support frequency was set at 10 times/min. The patient was instructed to breathe calmly. Once the patient’s breathing rhythm was regular, the inspiratory peak pressure was read. The patient’s respiratory stability was then observed, after which the MVV of the A/C patient was read.
MV measurement: First, the parameters of mechanical ventilation were adjusted as follows: A/C group: Vt: 8 mL/kg, F: 10 times/min; and PSV group: pressure support (PS) =10 cmH2O, positive end-expiratory pressure (PEEP) =5 cmH2O. As the RR and Vt were greatly disturbed by emotion, the MVV was measured when the patient’s mood was stable. The patient’s breathing condition was closely observed when the patient’s breathing was stable and the MV fluctuation was small, and the MVV was read when the patient’s respiratory was stable.
As a PB840 ventilator cannot measure maximum inspiratory negative pressure, the monitoring of MIP was temporarily changed to the drager EVITA XL ventilator. As the patient had already begun to prepare for weaning, ventilator replacement had no effect on the patient’s weaning. The “special program” option on the ventilator display screen was then selected, after which the sub-option of “diagnosis” was selected, followed by the option corresponding to the negative MIP, and “exhalation hold” was then continuously selected and held for 15 seconds. At the same time, the patient was instructed to inhale hard and read the MIP value. The patient was monitored once every 15 seconds, the readings were taken three times in total, and the average value was calculated as the obtained MIP value.
The index of shallow and rapid respiration was also measured. After the above parameters of the ventilator were measured, the ventilator was disconnected and the patient entered into spontaneous breathing. After one minute of observation, Vt was measured with a tidal meter three times consecutively. The average value was calculated, and RR was recorded at the same time. The respiratory index was calculated using the following formula: RSBI = f/Vt.
After the above parameters were measured, a spontaneous breathing test was administered and the T-tube method was selected. Methods: The patient’s vital signs were recorded, the ventilator was disconnected, and the observation time was 30–120 minutes. Vt was measured by tidal meter at 1, 3 and 30 minutes, RR was recorded, and the RSBI was calculated.
During the spontaneous breathing test, when the patient’s condition exceeded the following indexes, the spontaneous breathing test was stopped and the patient was switched to mechanical ventilation: (I) an RR/Vt (L) (shallow fast index) of <105; (II) an RR of >8 or <35 beats/min; (III) spontaneous breathing Vt of >4 mL/kg; (IV) a heart rate of less than 140 beats/min or changed <20%, without new arrhythmia; and (V) oxygen saturation of more than 90%.
A spontaneous breathing test was administered if the patient’s condition did not exceed the above-mentioned indexes, the vital signs of the patient were closely observed, and the required measurement parameters were recorded. The objective indicators of spontaneous breathing test (SBT) success were as follows: arterial blood gas index (FiO2 <40%, SpO2 ≥85–90%, PaO2 ≥50–60 mmHg, pH ≥7.32, and PaCO2 increase ≤10 mmHg); hemodynamic stability (HR <120–140 beats/min; HR change <20%; systolic blood pressure <180–200 and >90 mmHg; blood pressure change <20%, no need to use vasoactive drugs); and respiration (e.g., RR ≤30–35 beats/min; RR change ≤50%). The subjective clinical evaluation indicators of SBT failure were as follows: changes in mental state (e.g., drowsiness, coma, excitement, or anxiety); sweating; increased respiratory work (e.g., the use of auxiliary respiratory muscles, and contradictory breathing).
Based on the above criteria, patients who did not require mechanical ventilation again within 48 hours were classified into the successful weaning group, while those who required mechanical ventilation again or died within 48 hours were classified into the weaning failure group. Patients were then evaluated to determine if the orotracheal intubation could be removed. The possibility of extubation was determined based on a patient’s consciousness, expectoration ability, and amount of airway secretions. If extubation was permissible, the orotracheal intubation was removed. It should be noted that the oral and airway secretions were cleaned before extubation
Statistical analysis
SPSS 21.0 software package was used to analyze the data, and medcalc11.4 software was used to analyze the receiver operating characteristic (ROC) curve. The data were expressed as mean ± standard deviation (SD). An independent t-test was conducted to compare the two groups. The area under curve (AUC) was used to compare the predictive role of the weaning parameters. A P<0.05 was considered statistically significant.
Results
Successful weaning rates of both groups
As Table 2 shows, a total of 40 patients (33 male and 7 female) participated in this study. Of these patients, 25 were weaned successfully and 15 were weaned unsuccessfully. Thus, there was a success rate of 62.5%. In the A/C group, there were 12 successful weaning cases and 7 failure cases, yielding a success rate of 63%. In the PSV group, there were 13 successful weaning cases and 8 failure cases, yielding a success rate of 62%. After 24 hours, 31 cases were successfully weaned and 9 cases failed, yielding a success rate of 77.5%. Among 19 patients in the A/C group, there were 16 successful cases, yielding a success rate of 84%. Of the 21 cases in the PSV group, 15 were successful, yielding a success rate of 71.42%. After 48 hours, 34 cases were successfully weaned and 6 cases failed, yielding a success rate was 85%. Among 19 patients in the A/C group, 16 were successful, yielding a success rate of 84%. In the PSV group, 18 were successful, yielding a success rate of 85%. After 72 hours, 36 cases were successfully weaned and 4 cases failed, yielding a success rate of 90%. In the A/C group, 16 cases were successful, yielding a success rate of 84%. In the PSV group, 20 cases were successful, yielding a success rate of 95%.
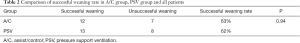
Full table
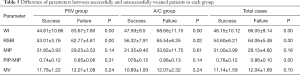
Case analyses of the successful and unsuccessful weaning groups
Patients were divided into the successful or unsuccessful weaning groups. There was no significant difference between the two groups in terms of age (67.87±9.78 vs. 67.28±10.34, P=0.86), gender (P=0.17), APACHE II score (15.47±3.76 vs. 13.76±4.12, P=0.15), height (168.71±7.39 vs. 165.04±10.18, P=0.92), ideal weight (64.4±7.23 vs. 62.94±9.77, P=0.61), ICU stay time (14.93±8.79 vs. 14.88±14.61, P=0.99), or hospitalization time (40.67±17.64 vs. 33.36±19.37, P=0.24). However, a significance difference between the two groups was found in relation to mechanical ventilation duration (8.53±5.09 vs. 5.44±4.12, P=0.04).
Case analyses of the A/C and PSV groups
Patients were divided into either the A/C group or the PSV group. There was no significant difference between the two groups in terms of age (67.19±9.78 vs. 67.84±10.52, P=0.84), gender (P=0.18), APACHE II score (14.14±4.58 vs. 13.58±4.47, P=0.69), height (170.71±6.51 vs. 165.32±10.18, P=0.05), ideal weight (65.94±6.77 vs. 60.78±10.17, P=0.07), mechanical ventilation duration (8.7±6.2 vs. 6.95±5.43, P=0.34), successful weaning rate (62% vs. 63%, P=0.94), inspiratory peak pressure (23±4.16 vs. 23.58±3.76, P=0.65), MV (11.61±1.19 vs. 11.28±2.02, P=0.52), MIP (28.9±4.42 vs. 27.42±5.02, P=0.33), RSBI 1 min (58.44±10.08 vs. 60.61±9.91, P=0.50), RSBI 3 min (62.37±12.46 vs. 65.47±10.98, P=0.41), RSBI 30 min (70.79±15.61 vs. 73.4±11.16, P=0.55), or WI (57.35±24.44 vs. 61.34±22.61, P=0.60) (Tables 3-5).

Full table

Full table
Full table
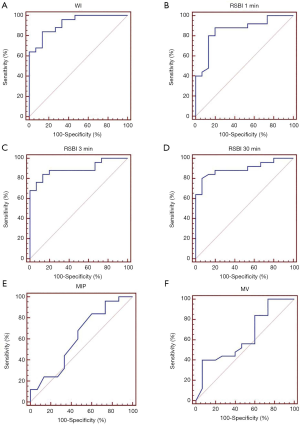
Predictive role of the WI in the A/C group
When the WI was less than 61.45 in the A/C group, the sensitivity and specificity were 98% and 72%, respectively. The area under the ROC curve was 0.917±0.068. There was no significant difference between the WI and RSBI, PIP/MIP (0.917±0.068 vs. 0.84±0.102, 0.917±0.068 vs. 0.673±0.132); however, there was a statistical difference between the WI and other parameters, such as MIP and MV (0.917±0.068 vs. 0.554±0.165, 0.917±0.068 vs. 0.66±0.148). There were significant differences in the WIs and RSBIs of the successful and unsuccessful weaning groups (68.66±11.15 vs. 47.59±9.5, P=0.00, RSBI 1 min 65.54±6.35 vs. 56.32±7.91, P=0.002, RSBI 3 min 69.58±6.01 vs. 61.48±8.66, P=0.04, RSBI 30 min 79.51±11.15 vs. 69.01±10.25, P=0.03). There was no significant difference in PIP, MIP, PIP/MIP and MV between the successful and unsuccessful weaning groups (25±2.24 vs. 523.33±1.97, P=0.1, 29±5.89 vs. 30.08±4.01, P=0.64, 0.88±0.13 vs. 0.79±0.12, P=0.14, 12, 07±2.32 vs. 10.89±1.93, P=0.24).
Predictive role of the WI in the PSV group
When the WI was less than 51.44 in the PSV group, the sensitivity and specificity were 76.9% and 100%, respectively. The area under the ROC curve was 0.923±0.05. There was no significant difference between the WI and RSBI (0.923±0.05 vs. 0.63±0.131); however, there was significant difference between the WI and other parameters (0.923±0.06 vs. 0.85±0.12, 0.923±0.04 vs. 0.615±0.09, 0.923±0.05 vs. 0.631±0.0131). There were significant differences in the WI and RSBI between the successful and failed weaning groups (63.67±7.81 vs. 44.81±10.86, P=0.00, RSBI 1 min 62.77±4.61 vs. 53.01±3.76, P=0.00, RSBI 3 min 73.05±5.71 vs. 58.01±5.35, P=0.00, RSBI 30 min 85.39±5.48 vs. 67.84±8.08, P=0.00). There was no significant difference in the mean of the MIP and MV between the successful and unsuccessful weaning groups (12.01±1.08 vs. 11.76±1.22, P=0.24, 29.25±3.53 vs. 31.85±3.93, P=0.16).
The total predictive role of the WI
When the WI was less than 50.44, the sensitivity and specificity of predicting weaning success were 84.6% and 100%, respectively. The area under the ROC curve was 0.933±0.05 (see Figure 1). There was no significant difference between the WI and RSBI (0.933±0.05 vs. 0.928±0.07); however, there was a statistical difference between the WI and other parameters (0.933±0.05 vs. 0.808±0.09, 0.933±0.05 vs. 0.692±0.133, 0.933±0.05 vs. 0.63±0.131). There were significant differences in the WI and RSBI between the successful and unsuccessful weaning groups (69.05±9.41 vs. 46.15±10.02, P=0.00, RSBI 1 min 64.06±5.48 vs. 54.6±6.21, P=0.00, RSBI 3 min 71.43±5.71 vs. 59.76±8.667.18, P=0.00, RSBI 30 min 82.65±6.67 vs. 68.4±9.01, P=0.00). There was no significant difference in the mean of the MIP and MV between the successful and unsuccessful weaning groups (29.13±4.59 vs. 31±3.99, P=0.18, 12.04±1.7 vs. 11.14±1.59, P=0.09).
Discussion
At present, ICU doctors will mainly judge whether patients can wean based on their own subjectivity, and lack scientific and effective data support. Although some doctors will try to wean based on the low-level pressure support model, the final decision is still mainly based on the clinical performance of the patient. There are differences in clinician experience, which may cause some patients to fail offline. Mechanical ventilation is associated with many complications; thus, it is important to confirm whether (and how soon) a patient can be removed from a ventilator. Additionally, it is clear that weaning can reduce respiratory muscle fatigue caused by weaning failure due to improper weaning, and prolonged mechanical ventilation duration (6-8). In recent decades, clinicians have made great efforts to make it scientific. Many WIs have been applied to clinical practice, such as the RSBI, MIP, P0.1/MIP, RR, Vt, MV, and CROP. Among them, the RSBI is the most widely used in clinical practice, as it is easy to obtain, does not require the cooperation of patients, and its predictive efficacy is better than other parameters. The results showed that when an RSBI was >105, the PPV was 78% and the NPV was 95%. Thus, it is necessary to improve the predictive efficacy of the RSBI to provide guidance as to when patients on mechanical ventilation can be weaned smoothly. The current study focused on parameters related to the RSBI to clarify a number of issues, including its clinical application feasibility, threshold, and predictive efficacy.
The phenomenon of shallow fast breathing was first discovered by Tobin and his colleagues. When there is an imbalance between the respiratory muscle strength and respiratory load, the phenomenon of shallow fast breathing occurs, and the shallow fast breathing index can be used to predict the failure of weaning (9). Yang and Tobin later conducted a study on this phenomenon, and found that the shallow and rapid breathing index of internal medicine patients under the air condition of spontaneous breathing with a T-piece was less than 105 times/min, and that this could be used as the offline prediction threshold. Subsequently, a study on the RSBI (10) showed that it had better predictive efficacy, was easy to obtain, did not require the cooperation of patients, and was easy to measure at bedside application.
All the predictive indexes of weaning were compared with the index of shallow rapid breathing. However, some studies have shown that (11-13) the RSBI has no advantage over other parameters, and may even prolong the offline time. Many factors affect the threshold value of the RSBI. Due to the different measuring time, measurement method, and application population, the RSBI threshold has not been the same in each study. In clinical practice, the RSBI is measured in PSV and CAPA mode, and the lower mechanical ventilation support condition (5–8 cmH2O) is often selected to reduce the increase in the respiratory load of patients due to an increase in additional airway resistance after mechanical ventilation.
Research (14) has shown that low-level support conditions can reduce respiratory work. Another study (15) showed that a threshold value in this mode was significantly lower than that of the conventional T-tube method. In theory, the condition of low-level respiratory support is closer to that without a catheter, which is more suitable for patients with poor cardiopulmonary function. However, at present, the rapid breathing index at 1 minute of spontaneous breathing under a T-tube is still used as the weaning standard, and the threshold value is 105. The results of this study showed that the optimal threshold value of the RSBI was 62, the area under the ROC curve was 0.885, the sensitivity was 88%, and the specificity was 80%. In relation to the T-tube oxygen inhalation, the RSBI of the failure group was 64.06±5.48, which was significantly higher than that of the successful weaning group; however, the threshold value was significantly lower than that of 105. For these reasons, Yang chose the T-tube method for autonomous air breathing. It should also be noted that the patients were medical patients. Conversely, in the present study, most of the selected patients were surgical patients, and the catheter oxygen inhalation method was used, which may have resulted in the lower threshold.
Different results have been suggested for the optimal threshold of RSBI. In 2012, Fadaii et al. (16) conducted a study with respiratory ICU patients (70 patients who had received mechanical ventilation for more than 48 hours participated in the study). The patients had a PSV of 0 and a PEEP of 0 in spontaneous breathing mode. After 1 minute, the RSBI was measured. The results showed that the RSBIs in the success and failure groups were 66±57.2 vs. 76.9±28.1; however, no statistical difference between the two groups was found. Huaringa et al. (4) showed that one third of patients failed to wean when their RSBIs were less than 105, their RSBIs were fell between 80 and 105, and the optimal threshold value of the RSBI was still uncertain. Thus, it is necessary to conduct research with different patients and across different conditions to determine whether 105 should continue to be used as the threshold value for the RSBI. It is suggested that a RSBI of less than 105 may not be a good threshold. Thus, further studies need to be conducted to determine the optimal threshold of the RSBI under different conditions.
RSBI dynamic change is an improved parameter for predicting weaning based on the RSBI. Krieger et al. (17) found that the specificity of RSBI increased from 57% to 89% and the area under the ROC increased from 0.81 to 0.93 after 3 hours of spontaneous breathing tests in elderly patients, and noted the importance of the dynamic observation of RSBI changes in predicting successful weaning. It may be that a patient’s respiratory load increases due to catheter resistance and complete spontaneous breathing after shutdown. Additionally, the positive chest pressure becomes negative, the amount of blood returned to the heart increases, and the cardiac preload also increases. If a patient cannot tolerate autonomous breathing with the extension of the shutdown time, the respiratory endurance will gradually decrease, the phenomenon of shallow and fast breathing will occur, and the possibility of weaning failure is greater. It is at this time that the RSBI is measured, if the measured value is significantly higher than before, the possibility of successful weaning is small and thus the predictive weaning ability increases.
Segal concluded that RSBI variability as a dynamic change marker can improve prediction offline ability (18). Furqan et al. found that a RSBI threshold of less than 105 can more accurately predict the successful weaning of patients in ICUs (19). However, the results of some related studies (20) did not support these findings. Notably, Teixeira et al. continuously measured the shallow and rapid respiratory index at 1, 30 and 120 minutes in a spontaneous breathing test, and found no statistical difference between the time points. Thus, the continuous monitoring of the RSBI cannot predict the weaning. In the present study, we measured the RSBI at 1, 3 and 30 minutes of a spontaneous breathing test, and compared the RSBI variability. The results showed that the RSBI of the unsuccessful weaning group was higher than that of the successful weaning group at each time point, and these differences were statistically significant. However, there was no significant difference in RSBI variability between the successful and unsuccessful weaning groups, which may be related to the small sample size of this study. Further research needs to be conducted to confirm this clinical finding.
RSBI has advantages over other parameters; however, its specificity is poor. In 2012, a new WI was proposed that included two correction parameters additional to the RSBI to improve its prediction efficacy. Under the WI, RSBI × EI × VDI (where EI = peak pressure/negative inspiratory force (NIF), and VDI = MV/10). The study showed that it was the most accurate offline predictive parameter. In the present study, the WI = RSBI × EI × VDI threshold value was 50, the AUC of area under curve was 0.981, sensitivity was 72%, specificity was 98%, while the AUC of the previous study was 0.959, sensitivity was 98%, and specificity was 89%. However, it should be noted that the previous study measured MV in the A/C mode to promote its application, while the present study measured MV in both the A/C mode and PSV mode. The results showed that compared with the PSV group, there were no significant differences in age, gender, ideal weight, success rate, APACHE II score, mechanical ventilation time, ICU stay time and hospitalization time between the two groups. There was no significant difference in the WI, RSBI, MIP, MV, ΔRSBI, and PIP/MIP between the two groups. When the WI of A/C group was less than 61.45, the sensitivity and specificity of predicting weaning success were 98% and 72%, respectively, and the area under the ROC curve was 0.917±0.068. When the WI of the PSV group was less than 51.45, the sensitivity and specificity of predicting weaning success were 76% and 100%, respectively, and the area under the ROC curve was 0.933±0.046. There was no significant difference in the predictive efficacy between the two groups. However, there were significant differences between the two groups in the threshold value, prediction sensitivity, and specificity. There was no statistical difference in each index between the two groups, which may be due to the small sample size, which in turn could have led to the large variability in the indicators measured in each group. There was no significant difference between the WI and RSBI. Further studies need to be conducted to confirm these results. The threshold value of the WI in this study was significantly lower than that in previous studies. The subjects selected in the previous study were mainly medical patients; however, the patients in in the present study were mainly surgical patients. Thus, more surgical patients were selected in the present study than the previous study. The cardiopulmonary function of the surgical patients was better than that of medical patients, their respiratory muscle strength was stronger, and their ability to tolerate spontaneous breathing was high, which may have led to the lower threshold value; however, further research needs to be conducted to confirm these findings.
The maximum inspiratory negative pressure reflects the maximum strength of the inspiratory muscle, which is widely used in clinical practice. The greater the negative pressure generated by the inspiratory muscle, the greater the possibility of successful weaning. The threshold value of the maximum inspiratory negative pressure was between –20 and –30 cmH2O. However, previous studies (21,22) have shown that this is not a good prediction parameter. The present study showed that the area under the MIP curve was 0.615, and the prediction ability was low. Notably, one of the reasons that a patient’s inspiratory capacity will be decreased with negative pressure machine withdrawal may also be one of the reasons that a patient's inspiratory capacity will be decreased when a ventilator is withdrawn. At present, single maximum inspiratory negative pressure as a prediction parameter is rarely used due to its low predictive ability. However, it is often combined with other parameters, such as P0.1*RSBI (23), CROP, and CROE, to improve its prediction ability. Conversely, the maximum inspiratory negative pressure only measured the inspiratory muscle strength, without considering the corresponding respiratory load, and whether it matched or not. Notably, the most common reason for weaning failure was the imbalance between the respiratory load and the respiratory muscle strength. The respiratory mechanics correction parameter in the WI proposed in the present study was EI = Peak Pleasure/NIF. If the EI is <1, then the patient’s respiratory muscle strength can overcome the maximum pressure required to reach the ideal Vt. An EI of <1 indicates that the inspiratory muscle strength is greater than the respiratory load, which in turn indicates that the possibility of successful weaning is high. Conversely, an EI of >1 indicates that the maximum inspiratory force of the patient is less than the respiratory load, that the patient is unable to achieve the ideal Vt by autonomous breathing, and that the possibility of successful weaning is small. The area under the EI = Peak Pressure/NIF curve was 0.727, the sensitivity was 48%, and the specificity was 93.3%. It has a certain predictive ability, which is better than the maximum inspiratory negative pressure prediction ability; however, further research needs to be conducted to verify these findings.
Teixeira and Sahn showed that (24,25) when MV was >10 L/min, patients displayed hyperventilation, the reaction center drive was enhanced, and thus the possibility of weaning failure was high and MV was not a good predictor of weaning. In the present study, VDI = MV/10. If VDI was <1, then patients did not show hyperventilation, which indicates that they may be weaned successfully. However, the question arises as to which ventilation mode should be used to measure ventilation. In the previous study, MVV was calculated under the support of quiet and full ventilation to reduce the effects of anxiety and other factors on the results of MV; however, this resulted in a large variation of MV. In the present study, patients were considered to be breathing spontaneously when they were offline; thus, the spontaneous breathing situation may better reflect the ventilation ability and central drive. This study suggested that the PSV mode be used to calculate the MV. The results showed that the MVV under the A/C mode was 29.68±4.63 vs. 30.86±3.92 under the PSV mode. Further, no statistical difference was found between the two modes. The results also showed that the area under the MV curve was 0.631 in the PSV mode, and 0.66 in the A/C mode. Further, there was no significant difference in MV under different modes in patients with quiet breathing. Thus, the measurement of MV in the PSV mode can replace that in the A/C mode. However, it should be noted the prediction capacity of weaning by MVV alone was low.
This study has a number of limitations. First, as patients in the A/C group needed a PB840 ventilator, the number of patients in the group was relatively small. This study needs to be conducted with a larger sample size to confirm these results. Second, in this study, we mainly focused on the WI related to the RSBI, and did not measure other indicators, such as comprehensive WI, CROP, or CROE. Further research needs to be conducted to compare the advantages and disadvantages of a comprehensive WI. Third, the first success rate of all patients was 62.5%, the 24-hour success rate was 77.5%, the 48-hour success rate was 85%, and the 72-hour success rate was 90%. However, in this study, no further follow-up study was conducted to measure the relevant indicators to indicate the reasons for the first weaning failure; thus, this issue requires further research.
Weaning parameters play an important role in mechanical ventilation evacuation, and there are many respiratory parameters. At present, composite parameters have gradually become a popular area of research because of their better predictive efficacy. However, in addition to its accurate predictive efficacy, a good weaning parameter also needs to be easily obtainable at the bedside. A repeatable measurement is an important prerequisite for its wide clinical promotion. The RSBI is undoubtedly the best choice. Thus, the question arises as to how the predictive ability of the RSBI can be improved without increasing the difficulty and complexity of clinical measurement. This study answers this question in part; however, further verification is needed.
To conclude, the WI predicts weaning results well, while the RSBI appears to have no advantage. When the WI is used, MV can be measured in the PSV mode rather than in the A/C mode.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at http://dx.doi.org/10.21037/apm-21-105
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-21-105
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-21-105). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by ethics committee of the Fourth Hospital of Hebei Medical University (No. 2020MEC106) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445-50. [Crossref] [PubMed]
- MacIntyre NR, Cook DJ, Ely EW Jr, et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College for Critical Care Medicine. Chest 2001;120:375S-395S. [Crossref] [PubMed]
- Huo Y, Guo S, Zhang K, et al. A clinical study on the ability of the integrative weaning index to predict weaning from mechanical ventilation. Ann Palliat Med 2020;9:3162-9. [Crossref] [PubMed]
- Huaringa AJ, Wang A, Haro MH, et al. The weaning index as predictor of weaning success. J Intensive Care Med 2013;28:369-74. [Crossref] [PubMed]
- Society of Critical Care Medicine, Chinese Medical Association. Practical guidelines for mechanical ventilation (2006). Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 2007;19:65-72. [PubMed]
- Eskandar N, Apostolakos MJ. Weaning from mechanical ventilation. Critical Care Clinics 2007;23:263-74. [Crossref] [PubMed]
- Hasani A., Grbolar A. Principles of weaning from the mechanical ventilation. Acta Informatica Medica 2008;16:83-5.
- chweickert W, Gehlbach B, Pohlman A, et al. Daily interruption of sedative infusions and complications of critical illness in mechanically ventilated patients. Critical Care Medicine 2004;32:1272-6.
- Yang KL, Tobin MJ. A prospective study of indexes predicting the outcome of trials of weaning from mechanical ventilation. N Engl J Med 1991;324:1445-50. [Crossref] [PubMed]
- Tobin MJ, Jubran A. Meta-analysis under the spotlight: focused on meta-analysis of ventilator weaning. Crit Care Med 2008;36:1-7. [Crossref] [PubMed]
- Boutou AK, Abatzidou F, Tryfon S, et al. Diagnostic accuracy of the rapid shallow breathing index to predict a successful spontaneous breathing trial outcome in mechanically ventilated patients with chronic obstructive pulmonary disease. Heart Lung 2011;40:105-10. [Crossref] [PubMed]
- Tanios MA, Nevins ML. A randomized controlled trial of the role of weaning predictors in clinical decision making. Crit Care Med 2006;34:2530-5. [Crossref] [PubMed]
- Fadaii A, Amini SS. Assessment of rapid shallow breathing index as a predictor for weaning in respiratory care unit. Tanaffos 2012;11:28-31. [PubMed]
- Pinsky MR. Cardiovascular issues in respiratory care. Chest 2005;128:592S-597S. [Crossref] [PubMed]
- Patel KN, Ganatra KD. Variation in the rapid shallow breathing index associated with common measurement techniques and conditions. Respir Care 2009;54:1462-6. [PubMed]
- Fadaii A, Amini SS, Bagheri B, et al. Assessment of rapid shallow breathing index as a predictor for weaning in respiratory care unit. Tanaffos 2012;11:28-31. [PubMed]
- Krieger BP, Isber J, Breitenbucher A, et al. Serial measurements of the rapid-shallow-breathing index as a predictor of weaning outcome in elderly medical patients. Chest 1997;112:1029-34. [Crossref] [PubMed]
- Segal LN, Oei E, Oppenheimer BW, et al. Evolution of pattern of breathing during a spontaneous breathing trial predicts successful extubation. Intensive Care Med 2010;36:487-95. [Crossref] [PubMed]
- Furqan A, Rai SA, Ali L, et al. Comparing the predicted accuracy of PO2\FIO2 ratio with rapid shallow breathing index for successful spontaneous breathing trial in Intensive Care Unit. Pak J Med Sci 2019;35:1605-10. [Crossref] [PubMed]
- Stetson JB. Introductory essay in prolonged tracheal intubation. Int Anaesthesiol Clin 1970;8:774-5. [Crossref]
- Nemer SN, Barbas CS, Caldeira JB, et al. Evaluation of maximal inspiratory pressure, tracheal airway occlusion pressure, and its ratio in the weaning outcome. J Crit Care 2009;24:441-6. [Crossref] [PubMed]
- Conti G, Montini L, Pennisi MA, et al. A prospective, blinded evaluation of indexes proposed to predict weaning from mechanical ventilation. Intensive Care Med 2004;30:830-6. [Crossref] [PubMed]
- Nemer SN, Barbas CS, Caldeira JB, et al. A new integrative weaning index of discontinuation from mechanical ventilation. Crit Care 2009;13:R152. [Crossref] [PubMed]
- Teixeira C, Zimmerman-Texeira PJ, Hoher JA, et al. Serial measurements of f/VT can predict extubation failure in patients with f/VT < or = 105? J Crit Care 2008;23:572-6. [Crossref] [PubMed]
- Sahn SA, Lakshminarayan S. Bedside criteria for discontinuation of mechanical ventilation. Chest 1973;63:1002-5. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


