
Effect of continuous nursing based on the Omaha System on cancer-related fatigue in patients with lung cancer undergoing chemotherapy: a randomized controlled trial
Introduction
According to global cancer statistics (1), there were approximately 2.09 million new cases of lung cancer in 2018, comprising 11.6% of all new cases of cancer, and around 1.76 million deaths, accounting for 18.4% of all cancer deaths. There are significant regional differences in the incidence and mortality of lung cancer, and China is a high-incidence country. According to the 2015 China Cancer Data Report (2), lung cancer was ranked the most common malignant tumor in China, with approximately 787,000 new cases, an incidence rate of 57.26 per 100,000, and a treatment success rate of 28.16 per 100,000.
As an important treatment approach for lung cancer, chemotherapy not only brings hope for patient survival, but also impacts the physical and mental health of individuals receiving it, with 19–96% of patients reporting varying degrees of fatigue during and after chemotherapy (3). Such fatigue impacts negatively on the body, mind, and mood, diminishing physicality and quality of life (4). In severe cases, chemotherapy may not farewell, and may even shorten survival and increase disease recurrence (5). Further, the occurrence and exacerbation of fatigue do not necessarily occur during hospitalization; there is a lag, with the majority occurring in the interval following chemotherapy (6,7). Therefore, the demands of patients with lung cancer for medical services, disease treatment information, symptom control, and psychological support are significantly greater during the interval following chemotherapy (8).
In the 1970s, the Visiting Nurse Association of Omaha began developing the Omaha System for community-based nursing practices; after 5 revisions and refinements, a research-based, comprehensive, standardized nursing classification system was developed (9). The Omaha System comprises 3 parts: problem classification, intervention, and problem outcome evaluation (10). The problem classification system covers 42 questions in 4 fields: environment, psychology, physiology, and health-related behavior. The intervention system divides nursing interventions into 4 categories: health education, guidance and consultation, treatment and procedure, and case management and monitoring. The outcome evaluation system uses a Likert 5-grade scoring method to evaluate patient problems based on 3 aspects: cognition, behavior, and condition. This system is a fundamental tool for assessing patient health problems from a holistic perspective and providing care interventions and outcome evaluation. With the improvement and maturity of the Omaha System, its application has been extended from its initial practice in community nursing to other fields, spanning the boundaries of the hospital, clinic, community, and family.
In 2003, the Omaha System was recognized by the American Nurses Association (ANA) as a supporting terminology standard for nursing practice in the United States, and is widely used in home care, clinical care, public health clinics, schools, and other mobile health care organizations (11). In 2010, the Omaha System was included as part of the training of community nurses in the “Training manual for Chinese mainland community care”, prepared by the World Health Organization (WHO) Collaborating Centre for Community Health Services.
In this study, the Omaha System was used as a framework to establish a model of continuous care for patients with lung cancer after chemotherapy, and the model used to implement the continuous care for patients with lung cancer after chemotherapy. Fatigue outcomes were compared between patients receiving standard care and those cared for using the Omaha System-based model. Further, common nursing problems and intervention measures were summarized, to provide scientific theory and practical guidance for improving cancer-related fatigue after chemotherapy for lung cancer.
We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2542).
Methods
Ethical approval
All participants provided oral and written informed consent before undertaking the study. The design of this study conformed to the Declaration of Helsinki (as revised in 2013), and the study was approved by the Ethics Committee of Hangzhou Cancer Hospital [Scientific Research Medical Ethics (035)-01].
Participants
A total of 102 patients with lung cancer who received chemotherapy at the Hangzhou Cancer Hospital from April 2018 to May 2019 were selected using a convenience sampling method. All patients were randomly divided into experimental group and control group according to random number table. The criteria for inclusion in this study were as follows: (I) patients with pathologically confirmed primary stage III and IV bronchopulmonary cancer who were treated with chemotherapy, as recommended by the International Union Against Cancer; (II) patients who received regular first-line platinum-containing double-drug or single-drug chemotherapy, including the following chemotherapy regimens: pemetrexed + platinum (PP), gemcitabine+ platinum (GP), docetaxel + platinum (DP), paclitaxel + platinum (TP), etoposide + platinum (EP), and single-drug chemotherapy; (III) age, ≥18 years; physical condition score, 0–2; cognition, normal; ability to read, write, and understand Chinese; (IV) patient provided informed consent, signed an informed consent form, participated voluntarily, and completed the study; (V) no contraindications to chemotherapy. Exclusion criteria were: (I) patients with lung cancer undergoing concurrent radiotherapy, immunotherapy, or targeted therapy; (II) patients with consciousness disturbance or mental disorders, or with poor compliance and unwillingness to cooperate with the investigation; (III) patients who stopped chemotherapy midway.
Intervention
Patients in the control group received routine continuous nursing care after discharge; that is, patients were contacted by the responsible nurse by telephone once within a week following discharge.
The observation group received continuous nursing based on Omaha System theory (12). The specific measures are described below.
- Basic information files were established for patients and the main problems to be addressed by continuous nursing were comprehensively analyzed using an intervention record sheet. The researchers, or trained nurses, evaluated the continuous care problems of participants by means of interview, examination, and consulting the nursing data.
- A health guidance manual for patients with lung cancer was issued. The manual was compiled with reference to the intervention categories in the Omaha intervention system and Maslow’s hierarchy of needs, and through literature review, evaluation of disease characteristics, expert panel discussions and consultation, and previous use by patients. The final revised form of the manual was entitled “Lung Cancer Patient Health Instruction Manual” and contained the following sections: A. Self-management of Adverse Reactions to Chemotherapy; B. Diet Management During Chemotherapy; C. Guidance on Sleep Disorders; D. Pain Management; E. Exercise Guidance; F. Catheter Maintenance; G. Reexamination Guidance and Disease Management; H. Psychological Rehabilitation; I. Related Guidance for Family Members.
- Problem-based continuity of care. The continuity of care team conducted a comprehensive analysis of continuity of care issues, to determine whether such issues were current or potential for patients with lung cancer undergoing chemotherapy, and whether they were personal or family-related. When patients had multiple problems in continuing nursing care, we applied Maslow’s hierarchy of basic human needs theory to the individual situations of patients to prioritize nursing problems. Continuity of care was maintained using a combination of online follow-up and on-site guidance. The specific intervention times and contents are detailed in Table 1, and intervention measures are described in Table 2. Continuous nursing intervention was evaluated during the second, third, and fourth cycles of chemotherapy in the same way as it was during the first cycle.

Full table

Full table
Evaluation tool
There are many assessment tools for cancer-related fatigue, such as Brief Fatigue Inventory (BFI), MD Anderson Symptom Inventory (MDASI), Cancer Line Analogy Scale (CLAS) and so on. Cancer Fatigue Scale (CFS), Schwartz Cancer Fatigue Scale (SCFS), Piper Fatigue Scale (PFS) and others can be used as multi-dimensional fatigue scale to measure the intensity, duration and impact of fatigue on daily life. Considering the specificity of the subjects and the feasibility of filling in the questionnaire, the CFS was chosen as the research tool in this study.
Before the first chemotherapy, at the end of the second cycle, and at the end of the fourth cycle, the study team used the Cancer Fatigue Scale (CFS), which was developed by Okuyama et al. (13), and includes 15 items categorized in 3dimensions: body, emotion, and cognition, with 7, 4, and 4 items in the physical, emotional, and cognitive fatigue dimensions, respectively. Each item was rated from 1(no fatigue) to 5(severe fatigue), with a total score of 15–75. The higher the score, the more severe the fatigue. Cronbach’s coefficient values for all dimensions of the scale and the total scale were 0.63–0.86. Retest reliability was 0.55–0.77.
Statistical methods
Data were entered in Microsoft Excel and then analyzed using SPSS statistical software (SPSS version 25.0; IBM, Armonk, NY, USA). Categorical data are described as numbers and percentages, and comparisons between groups were conducted using a t-test. Continuous data are described as means and standard deviation (SD), and comparisons between 2 groups were made by ANOVA of repeated measures data. A P value <0.05 was considered statistically significant.
Results
Participants
A total of 102 participants were included in this study; 7 were lost to follow-up, 4 in the experimental group and 3 in the control group, giving a loss to follow-up rate of 6.9%. Reasons for loss to follow up were that 4 participants were unable to continue due to sudden deterioration of their condition, 1 was unable to continue due to transfer to another hospital for treatment, 1 was unable to continue chemotherapy for financial reasons, and 1 participant was lost because of a change in the method of contact. In total, 46 and 49 patients in the experimental and control groups completed follow-up, respectively. Basic data for the 2 groups of patients are presented in Table 3. There were no significant differences in baseline characteristics between the 2 groups (P>0.05).
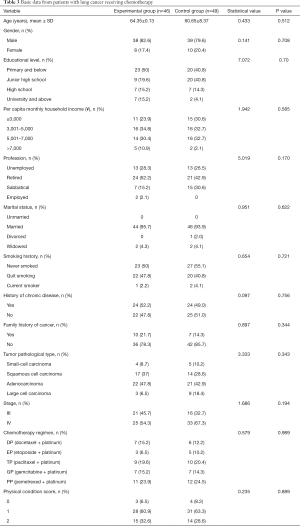
Full table
Comparison of the scores of cancer-related fatigue before and after intervention between groups
Cancer-related fatigue scores before intervention, after the second round of chemotherapy, and after the fourth round of chemotherapy were compared between the 2 groups (Table 4). After the fourth cycle of chemotherapy, fatigue scores were significantly lower for patients in the intervention group compared to those in the control group (P<0.05). However, there were no significant differences between the groups at the other time points.
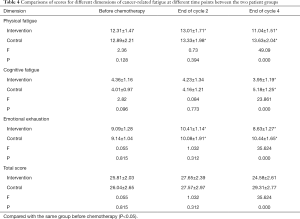
Full table
Changes in cancer-related fatigue over time in the two patient groups
Total cancer-related fatigue scores before and after intervention were assessed by repeated ANOVA measures, and effects were evaluated according to time, intervention, and interaction between time and intervention, to determine the influence of the intervention on comparative observation indices. The results showed that there were significant time- and intervention-dependent differences in fatigue scores (both P<0.001). Further, there was a significant interaction between time and intervention factors (P<0.001) (Table 5 and Figure 1), where total cancer-related fatigue score after the intervention was significantly lower than that of the control group.
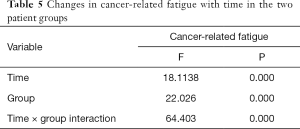
Full table
Discussion
Carcinogenic fatigue is a persistent subjective feeling of physical, emotional, or cognitive fatigue associated with cancer or cancer treatment (14). Compared with general fatigue, cancer-related fatigue is characterized by rapid onset, high severity, lasting duration, unpredictability, inability to relax through rest or sleep, and serious impacts on daily life, rehabilitation, and long-term quality of life (15).
The pathogenesis of cancer-related fatigue has not been completely determined, but its influencing factors are relatively clear, in addition to cancer itself, treatment methods and complications, the negative psychological factors, the bad life style and the negative family social function of the patients with lung cancer will aggravate the cancer-related fatigue. With effective control measures already existing for nausea, vomiting, pain, and other symptoms, for inpatients with cancer, cancer-related fatigue has become a primary concern, and is one of the most common and important reasons that patients cease treatment. Proper assessment, treatment, and care of fatigue symptoms are increasingly recognized as important aspects of cancer follow-up. The incidence of cancer-related fatigue during chemotherapy in cancer patients was 51% (16) in Germany, compared with 76.35–87% in China (17).
As the specific cause of cancer-related fatigue is unclear, there is no uniform international standard for drug treatment of this condition. Maintaining specified activity, avoiding sedentary behavior, and changing poor eating habits can help patients with cancer to recover from fatigue (18). Further, some forms of aerobic exercise can be effective in reducing fatigue (19). In 2007, a team of evidence-based medicine researchers at the American Society of Oncology highlighted that exercise has been confirmed by first-level evidence as an effective intervention measure for cancer-related fatigue. Health care workers tend to encourage patients to rest to ease their fatigue, while studies have shown that not exercising can lead to undesirable consequences, such as muscle atrophy and decreased cardiorespiratory fitness, as well as lower self-confidence and reduced social interaction (20).
The health instruction manual for patients with lung cancer developed in this study provides 3 exercise principles including the principle of quantitative and quantitative exercise, the principle of exercise and gradual progress, the principle of whole body exercise and local supplement, 4 modes of exercise, and a set of breathing exercises for patients with lung cancer, to allow patients to choose the mode of exercise that suits them, and instruct them to exercise optimally for relief of fatigue. And patients only need to guarantee the movement frequency three times a week, therefore, the movement time can be adjusted by the patients according to their physical condition.
Lung cancer and lung cancer treatment can lead to patients with nausea, vomiting and diarrhea and other gastrointestinal symptoms, these symptoms can be accompanied by anemia, weight loss, water and electrolyte disorders. All of these symptoms can lead to fatigue. Therefore, in this study, scientific guidance of patients with reasonable diet and nutrition, so that patients in good nutritional status is conducive to reduce the occurrence of cancer-related fatigue. During follow-up, patients were repeatedly instructed to follow a scientific diet and exercise regimen, assisted to correct bad habits in their daily diet, and urged to eat according to a scientific plan to the best of their ability. These encouragements were made to reduce patient morbidity due to improper diet, such as constipation, diarrhea, and malnutrition, as well as other adverse reactions. Further, functional exercise guidance was provided to help patients restore physiological function as soon as possible. The continuity of care model developed in this study, based on Omaha System theory, can be of more rapid assistance to patients, help them better adapt to lifestyle changes, and assist in functional recovery, while simultaneously ameliorating the fatigue caused by chemotherapy and changes in living habits to some extent, as well as reducing the duration of fatigue.
Conclusions
To summarize, continuous nursing based on Omaha System theory is helpful for improving cancer-related fatigue in patients with lung cancer undergoing chemotherapy. The model developed in this study facilitated identification of existing or potential nursing problems during rehabilitation in a timely and accurate manner. Further, the system enabled development of individualized continuous nursing intervention measures, based on specific problems, which improves patient compliance with self-care, and greatly ameliorates cancer-related fatigue. To improve fatigue and quality of life efficiently and systematically, the Omaha System of continuity of care should be recommended for patients with lung cancer, and potentially also other types of cancer. The intervention and evaluation of this study lasted only 4 cycles of chemotherapy. The long-term effect of the Omaha-based continuum of care needs to be further explored. In the future, the effect of the intervention can be maintained by prolonging the intervention cycle, and whether the extension of the intervention will further reduce the degree of cancer-related fatigue.
Acknowledgments
Funding: This work was supported by the 2017 Hangzhou Health Science and Family Planning Science and Technology Program, Key Projects (2017Z02).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2542
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2542
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2542). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The design of this study conformed to the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Hangzhou Cancer Hospital [Scientific Research Medical Ethics (035)-01] and written informed consent was provided by participants for the publication of this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mauguen A, Pignon JP, Burdett S, et al. Surrogate endpoints for overall survival in chemotherapy and radiotherapy trials in operable and locally advanced lung cancer: A re-analysis of meta-analyses of individual patients’ data. Lancet Oncol 2013;14:619-26. [Crossref] [PubMed]
- Brown Johnson CG, Brodsky JL, Cataldo JK. Lung cancer stigma, anxiety, depression, and quality of life. J Psychosoc Oncol 2014;32:59-73. [Crossref] [PubMed]
- Manir KS, Bhadra K, Kumar G, et al. Fatigue in breast cancer patients on adjuvant treatment: course and prevalence. Indian J Palliat Care 2012;18:109-16. [Crossref] [PubMed]
- Lin C, Diao Y, Dong Z, et al. The effect of attention and interpretation therapy on psychological resilience, cancer-related fatigue, and negative emotions of patients after colon cancer surgery. Ann Palliat Med 2020;9:3261-70. [Crossref] [PubMed]
- Groenvold M, Petersen MA, Idler E, et al. Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat 2007;105:209-19. [Crossref] [PubMed]
- Kim DI, Choi MS. Guidance for prospective acupuncture treatment on cancer-related fatigue (CRF). Ann Palliat Med 2013;2:7-10. [PubMed]
- Asawari LR, Palak P, Chintan P, et al. Preventability, predictability and seriousness of adverse drug reactions amongst medicine in patients in a teaching hospital: A prospective observational study. Int J Pharm Chem Sci 2012;1:1293-9.
- Maguire R, Papadopoulou C, Kotronoulas G, et al. A systematic review of supportive care needs of people living with lung cancer. Eur J Oncol Nurs 2013;17:449-64. [Crossref] [PubMed]
- Martin KS. The Omaha System: Past, present, and future. Online J Nurs Infor 1999;3:1-6.
- Martin KS. The Omaha System: A key to practice, documentation and information management. St Louis Mo: Elsevier Saunders, 2005:11-12.
- Simpson RL. What's in a name? The taxonomy and nomenclature puzzle, part 1. Nurs Manage 2003;34:14-8. [PubMed]
- Lin L, Li Y, Wang L, et al. Construction of transitional care evaluation system for lung cancer patients with chemotherapy based on Omaha system. Chin J Mod Nurs 2020;26:2550-6.
- Okuyama T, Akechi T, Kugaya A, et al. Development and validation of the cancer fatigue scale: A brief, three-dimensional, self-rating scale for assessment of fatigue in cancer patients. J Pain Symptom Manage 2000;19:5-14. [Crossref] [PubMed]
- National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Cancer-Related Fatigue (01.2014). Available online: ; accessed Nov 28, 2016.www.nccn.org
- Ebede CC, Jang YC, Escalante CP. Cancer-related fatigue in cancer survivorship. Med Clin North Am 2017;101:1085-97. [Crossref] [PubMed]
- Kuhnt S, Szalai C, Erdmann-Reusch B, et al. Cancer related fatigue in rehabilitation care. Rehabilitation (Stuttg) 2017;56:337-43. [PubMed]
- Xu H, Jiang L, Yin Z, et al. Investigation on cancer-related fatigue of lung cancer patients receiving chemotherapy. Chin J Nurs 2010;45:332-5.
- Brown JC, Huedo-Medina TB, Pescatello LS. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: A meta-analysis. Cancer Epidemiol Biomarkers Prev 2011;20:123-33. [Crossref] [PubMed]
- Zou LY, Yang L, He XL. Effects of aerobic exercise on cancer-related fatigue in breast cancer patients receiving chemotherapy: A meta-analysis. Tumour Biol 2014;35:5659-67. [Crossref] [PubMed]
- Tomlinson D, Diorio C, Beyene J. Effect of exercise on cancer-related fatigue: A meta-analysis. Am J Phys Med Rehabil 2014;93:675-86. [Crossref] [PubMed]
(English Language Editor: J. Jones)



