The effect of Xiaobi decoction on minimal erythema dose of irradiation with 308 nm excimer lamp in guinea pigs
Introduction
Psoriasis is a chronic, autoimmune-mediated inflammatory skin disease (1), with a pathogenesis that is predominantly related to genetic, environmental, and immune factors. Clinically, psoriasis mainly manifests as scaly erythema, and can be divided according to clinical characteristics into common type (95% of cases), pustular type, erythroderma type, and arthropathy type.
Systemic, physical, and drug therapies are frequently used in the treatment of psoriasis. Systemic therapy includes tretinoin drugs, immunosuppressants, cytotoxic drugs, and biological agents. Short-term use of these drugs can significantly relieve psoriasis patients’ lesions of this; however, their long-term use is associated with significant side effects, and patients with psoriasis often suffer relapse after stopping these drugs. In terms of drug therapy, glucocorticoids, vitamin D derivatives, tar preparations, calcineurin inhibitors, and tretinoin are commonly used to treat psoriasis. These drugs have definite clinical efficacy for treating patients with mild disease or early disease, but their long-term clinical use is limited due to the adverse reactions associated with the increase in transdermal absorption at the skin lesions.
Physiotherapy mainly includes broad-spectrum ultraviolet (UV), narrow-band UVB (NB-UVB), photodynamic therapy, photochemotherapy, and 308-nm excimer phototherapy. Excimer 308-nm light can specifically act on the lesions and has a high safety profile. It has been widely used to treat clinical psoriasis, vitiligo, and other diseases. The local radiation dose of 308-nm excimer light is high, and phototoxic reactions are a common side effect, which can cause pain in the irradiated area, local reversible edematous erythema, blistering, and pigmentation. The clinical effect of 308-nm excimer light is beneficial in psoriasis patients with a skin lesion area less than 10% of the body surface area. The main therapeutic mechanism of 308-nm excimer light is the inhibition of T lymphocyte proliferation and the induction of T cell apoptosis (2). With 308-nm excimer light, the energy delivered to the irradiated area of skin is 5–10 times higher than that delivered with NB-UVB, and the skin lesions can also reduce the risk of skin photoaging and carcinogenesis while receiving high-energy treatment (3). Some scholars have concluded through clinical comparative studies that while there is no statistical difference in efficacy or safety between 308-nm excimer light and 308-nm excimer laser, 308-nm excimer light offers a bettermore effectiveness treatment than 308-nm excimer laser at a lower cost (4,5).
Because the specific pathogenesis of psoriasis is still unclear, a significant improvement ofin a patient’s condition cannot be easily achieved with traditional Chinese medicine or Western medicine alone. Combinations of traditional Chinese medicine and western medicine and combinations of internal and external treatment have gradually become treatment options for patients with psoriasis. Professor Jia Min, a well-known Chinese medicine doctor, has been engaged in the treatment of skin diseases for decades, and has unique insights into the treatment of psoriasis. According to the theory of traditional Chinese medicine, Xiaopi decoction is an empirical prescription for treating psoriasis vulgaris of “blood heat and wind-drying” type in its clinical stage. The prescription primarily focuses on clearing “heat” and removing “wind”, cooling “blood”, and stopping itching. In clinical practice, Xiaobi Decoction combined with 308-nm excimer light has been found to achieve a good effect for patients with advanced psoriasis vulgaris, with a low recurrence rate (6-9). In preliminary experiments, our research team found that Xiaobi decoction can affect the minimal erythema dose (MED) in experimental mice. To date, there has been no similar report on the mechanism of the effect of drugs combined with 308-nm excimer light in the treatment of psoriasis. Whether Xiaobi decoction improves the therapeutic effect of 308-nm excimer light by influencing the sensitivity of psoriasis patients to light is worth investigating. Therefore, this study aimed to observe the effect of Xiaobi decoction on the minimal erythema dose (MED) value in guinea pigs. We present the following article in accordance with the ARRIVE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2181).
Methods
Experimental animals
Eighty ordinary healthy guinea pigs (1:1 sex ratio; weight 324.7±16.3 g) were purchased from Chongqing Tengxin Biotechnology Co., Ltd. (animal license number: SCXK-Chongqing-2017-0010; animal certificate number: 0005242). The guinea pigs were raised in separate cages in the Animal Laboratory of Guizhou University of Traditional Chinese Medicine. This study was approved by the Animal Experiment Ethics Committee of the First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine and complied with Guidelines for the Ethical Review of Laboratory Animal Welfare (GB/ T35892-2018).
Herbs and agents
Xiaobi decoction composition: Rehmannia glutinosa 20 g, Scutellaria baicalensis 15 g, Honeysuckle 15 g, Forsythia 15 g, Viola dianthus 15 g, Faxia 15 g, Dandelion 15 g, Black Snake 15 g, Peach kernel 15 g, Safflower 15 g, Hive 10 g, Leech 10 g, Guizhi 8 g (total of 183 g) were supplied by our pharmacy.
Xiaobi decoction preparation method: All ingredients were soaked in cold water for 20 minutes. Then, 500 mL of water was added for each dosage of medicine, and the ingredients were boiled together and decocted on a tiny fire for 30 minutes. The decoction was poured out, and the process was repeated 2twice more. The decoctions were mixed, and then heated and condensed into 100 mL of decoction. After cooling, the decoction was stored at 4 °C in the refrigerator at the Animal Institute of Guizhou University of Traditional Chinese Medicine. Sodium sulfide depilatory was purchased from Guizhou Biotech Trading Co., Ltd.
Apparatus
Xilan 308 nm Excimer Light Therapy Apparatus was purchased from Oxtail Motor (Suzhou) Co., Ltd.; Model number: ADM002. Guinea pig vascular endothelial growth factor (VEGF) and interleukin-23 (IL-23) enzyme-linked immunosorbent assay (ELISA) kits were purchased from Shanghai Xitang Biotechnology Co., Ltd. Mouse anti-human CD34 monoclonal antibody was purchased from Bio-Worlde, USA, and a mouse SP-kit immunohistochemistry kit was purchased from Beijing Zhongshan Biotech Co., Ltd. [including biotin-labeled secondary antibody, peroxidase-labeled streptavidin, and 3,3’-diaminobenzidine (DAB) developer].
Animal grouping
The guinea pigs were randomly divided into a Xiaobi decoction group and a control group according to serial number; guinea pigs with odd numbers were assigned into the Xiaobi decoction group (n=40), and those with even numbers were assigned into the control group (n=40). The average body weight of the guinea pigs in the Xiaobi decoction group was (327.33±10.09) g, compared with (322.13±20.24) g in the control group; the difference was not statistically significant (P>0.05). The guinea pigs in the Xiaobi decoction group were administrated Xiaobi decoction by gavaging, and the guinea pigs in the control group were administrated distilled water.
Treatment
The minimum dose administered to the two groups of guinea pigs by gavaging was calculated using a method described in the “Methodology of Traditional Chinese Medicine Pharmacology” (10). The cCalculation tTable in this book shows that the conversion coefficient of the standard body weight for adult human beings with guinea pigs is 4.63: if the daily dose for adult human beings is 100 mL/60 kg = 1.67 g/kg, then the daily dose for guinea pigs should be 1.67 g/kg × 4.63 = 7.73 mL/kg.
Hair removal
First, the long hair on the back of the guinea pigs was cut with scissors. Then, a cotton swab was dipped in sodium sulfide depilatory and applied to the target area. After the short hair was soaked and left for 2–3 minutes, the depilated area was washed with warm water, and the back skin of the guinea pigs was dried with disinfected medical gauze.
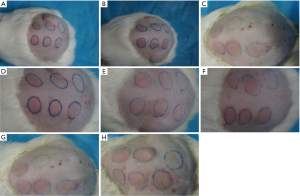
Pre-gavage measurement of MED
The first 10 guinea pigs according to number were taken, and their back hair was removed. Six points were selected and marked with a marker, with each point measuring approximately 1 cm2. Each point was irradiated once with a single dose of 308-nm excimer light. The dose of irradiation delivered to the first point was 200 mJ/cm2, and the energy was increased by 200 mJ/cm2 for each point after that; therefore, the irradiation doses for the 6 points were 200, 400, 600, 800, 1,000, and 1,200 mJ/cm2. After 24 hours, the MED of the guinea pigs was observed before gavaging.
Post-gavage measurement of MED
The MED value of the ten10 guinea pigs was measured before gavaging. The guinea pigs were gavaged daily, and back hair removal was performed on the 10th, 20th, and 30th days of gavaging. Six points were marked and irradiated with 308-nm excimer light. The guinea pigs were observed and the MED value for each erythema that occurred was recorded. The irradiation dose with the most significant MED was taken as the upper limit dose for the next irradiation after gavaging. Based on the upper limit dose, six points were selected and treated with successive doses of irradiation, which decreased by 50 mJ/cm2 each time. MED values were measured after 20 days and 30 days of gavaging. The MED value was measured in the irradiated area 24 hours after irradiation. The MED value was interpreted by three observers with rich experience simultaneously. At least two of the observers needed to agree for the energy to be regarded as the MED. Erythema or light erythema after 24 hours was considered positive. No erythema was considered negative.
Detection of VEGF and IL-23
After the experiment, the animals were anesthetized with 10% chloral hydrate, and blood from the abdominal aorta was collected into a centrifuge tube. The centrifuge tube was stood for 3 hours, before the serum was collected for later use through centrifugation at 4 °C at 3,000 r/min for 10 minutes. The levels of VEGF and IL-23 were detected using ELISA kits according to the manufacturer’s instructions.
Statistical analysis
The statistical data were processed with SPSS 23.0 statistical software (IBM, Illinois, USA.). Category variables were expressed as percentages and compared between groups using the chi-square test. Continuous variables were expressed as means ± standard deviations; comparisons between groups were made using Student’s t-test if the data followed a normal distribution, while non-parametric tests were used for data with non-normal distribution. P>0.05 was considered to be statistically significant.
Results
Comparison of MED between the two groups
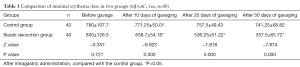
Before the administration of the drugs, the MED value in the Xiaobi decoction group was (800±126.5) mJ/cm2, compared with (780±107.7) mJ/cm2 in the control group; the difference was not statistically significant (P >0.05). However, after 10 days of intragastric administration, the MED value of the Xiaobi decoction group (638.75±54.18 mJ/cm2) was statistically significantly lower than that of the control group (771.25±50.01 mJ/cm2) (P<0.05). After 20 days of intragastric administration, the MED value of the Xiaobi decoction group was (536.25±51.22) mJ/cm2 compared with (757.5±49.43) mJ/cm2 in the control group, and the difference was statistically significant (P<0.05). After 30 days of gastric administration, the MED value of the Xiaobi decoction group was (357.5±65.72) mJ/cm2, which was significantly lower than that of the control group was (741.25±68.82) mJ/cm2 (P<0.05). These results are described in Table 1 and Figure 1.
Comparison of VEGF levels and IL-23 levels in two groups
The two groups of guinea pigs were sacrificed after MED measurement at the end of 30 days of gavaging. Abdominal aortic blood was taken, and the serum levels of VEGF and IL-23 were detected. The results are shown in Table 2. The serum VEGF and IL-23 levels of the guinea pigs in the Xiaobi decoction group were lower than those of the control group animals. This result suggests that Xiaobi decoction can reduce the serum expression levels of these two cytokines.

Full table
Discussion
The MED refers to the minimum radiation dose that will cause visible erythema or light erythema on an area of skin 24–48 hours after exposure to irradiation of a specific light source or wavelength. The measurement of MED value can help to gain a better understanding of the sensitivity of the patient’s skin to a phototherapy instrument. However, it is influenced by factors such as the location of the light, skin type, stratum corneum thickness, and sex. Clinically, the MED value determines the initial dose of local light irradiation, which is usually 50–70% of the MED value. If the initial dose is too low, the clinical efficacy will be poor or the therapeutic effect may even be lost. However, if the initial dose is too high, the risk of adverse reactions will increase.
The treatment and prognosis of skin diseases are of great significance (11). In recent years, phototherapy has become a popular method for the treatment of psoriasis. The advantage of performing MED measurement before phototherapy is that it allows doctors to understand the patient’s sensitivity to light in advance and to choose the best treatment dose in order to avoid serious side effects. Some scholars (12) have found that a faster clinical curative effect can be obtained when the irradiation dose is greater than or equal to the MED, which is beneficial in reducing the number of phototherapies and the cumulative dose. Rodríguez-Granados (13) used NB-UVB to perform MED measurement on 302 patients with various skin diseases and found that the skin lesions of psoriasis patients were resistant to lower radiation doses, which further confirmed that patients with psoriasis should receive a dose of no less than the MED. In 2014, Han et al. (14) determined that the MED of psoriasis model mice treated with NB-UVB was 350 mJ/cm2. The irradiation dose was set to 100 mJ/cm2 and 400 mJ/cm2 once a day for the low-dose and high-dose groups, respectively. After 5 days of continuous irradiation, pathological examination was conducted, the results of the disease examination showed that the expression levels of keratinocytes and keratin K17 in the low-dose group model mice were increased compared to those before irradiation, while in the high-dose group, the levels of keratinocytes and keratin K17 were significantly inhibited. Yue and Wang (15) confirmed through in vivo experiments that erythema under the guidance of MED is safe and reversible. In summary, the measurement of MED is helpful for doctors in choosing the appropriate initial dose for a patient; thereby, it increases the therapeutic efficacy and reduces the incidence of adverse reactions.
In traditional Chinese medicine, psoriasis is known as “cowhide ringworm” (niupi xian). Ancient physicians believed that psoriasis was a chronic disease induced by a combination of internal and external factors. In the theory of traditional Chinese medicine, these external factors were mainly “wind”, “dampness”, and “heat”, which attack the body and cause blood pulsation, qi imbalance, and blood stasis, leading to muscle loss of qi and blood nourishment, long-term skin dryness, desquamation, internal causes of blood heat, deficiency, dryness and stasis. and“Blood heat” is the fundamental cause of disease and runs through the entire pathogenesis of psoriasis, and the treatment should be based on “blood theory” (16).
Xiaobi decoction is a clinically proven prescription developed by Professor Jia Min for the treatment of advanced-stage psoriasis vulgaris and dialectical psoriasis of blood-heat and wind-dryness in traditional Chinese medicine. The prescription has the effects of clearing “heat” and removing “wind”, cooling the blood, and stopping itching. Previous studies have confirmed that patients with psoriasis have a good prognosis and a low incidence of adverse reactions after taking Xiaobi decoction (6). He et al. (9) randomly divided 60 patients into a Xiaobi decoction group and an Acitretin capsule group. After 3 months of treatment, they found that the peripheral serum soluble intercellular adhesion molecule (sICAM-1), tumor necrosis factor-α (TNF-α), and monocyte chemoattractant protein-1 (MCP-1) levels of patients in the Xiaobi decoction group were decreased and significantly lower than those of the patients treated with Acitretin capsules. Wu et al. (7,8) found that Xiaobi decoction can reduce the proportion of pro-inflammatory cytokine T-helper (Th)17 cells and interferon gamma (IFN-γ), IL-8, IL-17, IL-18, IL-22, IL-23. in the serum of patients with psoriasis, while increasing the proportion of serum Treg cells and the expression levels of IL-10, TGF-β1 and other anti-inflammatory cytokines. They also observed that Xiaobi decoction could help to balance Th17/Treg levels, thereby controlling the inflammatory response of psoriasis and exerting an immunomodulatory effect. The above-mentioned clinical studies have demonstrated that Xiaobi decoction can increase the expression of anti-inflammatory factors while reducing the levels of pro-inflammatory cytokines in the serum to achieve the effect of treating psoriasis. Hu et al. (17) treated propranolol model rats with Xiaobi decoction. After 2 weeks, skin pathology was performed, and the results showed that Xiaobi decoction had inhibited keratinocytes in the psoriasis model group and reduced the infiltration of inflammatory cells in the skin lesions. Its curative effect is equivalent to that of Acitretin capsules.
Scutellaria baicalensis Georgi in Xiaobian Decoction has the effects of clearing away “heat”, “fire”, and “dampness”. Honeysuckle and forsythia have the effects of clearing “heat”, cooling “blood”, and dispelling “knots” and “carbuncle”. Sheng Dihuang is an important medicine for clearing “heat”, cooling “blood”, and promoting body fluid. The combination of these four drugs constitutes a “master drug” that can achieve the effects of dispelling “blood, heat and toxins”, and cooling the “blood”. Hive, black snake, and leech are all medicines obtained from animals. The combination of these three medicines is a minister medicine that enhances the effects of dispelling “wind”, relieving itching, promoting blood circulation, and removing blood stasis. Its usage is also consistent with the theory of “to treat wind, firstly treat blood, and the wind will disappear when the blood flows”. The combination of peach kernel and safflower promotes blood circulation, removes blood stasis, and thus has the effect of cooling blood without leaving blood stasis, promoting blood circulation without injuring the blood. The combined use of dandelion and purple ditin can enhance the power of the monarch medicine to clear heat and cool blood. The sweetness of cinnamon sticks can warm and regulate the meridians, and some scholars (18) have concluded through in vivo experiments that cassia sticks can promote the recovery of psoriasis model mice. To prevent the large doses of cold and cool products from negatively affecting the “spleen and stomach”, we added Pinellia to moderate the yin and yang in order to relieve any gastric discomfort caused by the above-mentioned drugs. The important pathological changes of psoriasis include abnormal microcirculation in the skin lesion area and impaired vascular endothelial function. Therefore, psoriasis can be relieved by treatment with drugs that improve vascular endothelial function and regulate microcirculation (19,20). The main treatment of this disease emphasizes “treatment based on blood”. These drugs have anti-inflammatory, antibacterial, and vasodilating effects, and can improve blood circulation. They are all drugs that have the effect of improving psoriasis skin lesions, which is enhanced by combining the monarch and the minister medicines.
This study found that Xiaobi decoction could reduce the MED value in guinea pigs and that a treatment effect could be achieved using a lower light energy. Therefore, it is speculated that another mechanism of Xiaobi decoction in the treatment of psoriasis is to increase the absorption of 308-nm excimer light in patients with psoriasis. Sensitivity is related to the absorption of skin lesions. At the same time, Xiaobi decoction was found to reduce the levels of serum VEGF and IL-23 in guinea pigs. In conclusion, the combination of Xiaobi decoction with 308-nm excimer light phototherapy may reduce the total number of phototherapies and the cumulative radiation dose and related serum factors, thereby reducing the incidence of potential side effects of phototherapy while improving erythema.
Acknowledgments
Funding: Guiyang Science and Technology Project {[2019]9-2-37}.
Footnote
Reporting Checklist: The authors have completed the ARRIVE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2181
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2181
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2181). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Animal Experiment Ethics Committee of the First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine and complied with Guidelines for the Ethical Review of Laboratory Animal Welfare (GB/ T35892-2018).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Golbari NM, Porter ML, Kimball AB. Current guidelines for psoriasis treatment: a work in progress. Cutis 2018;101:10-2. [PubMed]
- Bulat V, Situm M, Dediol I, et al. The mechanisms of action of phototherapy in the treatment of the most common dermatoses. Coll Antropol 2011;35 Suppl 2:147-51. [PubMed]
- Beggs S, Short J, Rengifo-Pardo M, et al. Applications of the Excimer Laser: A Review. Dermatol Surg 2015;41:1201-11. [Crossref] [PubMed]
- Shi Q, Li K, Fu J, et al. Comparison of the 308-nm excimer laser with the 308-nm excimer lamp in the treatment of vitiligo--a randomized bilateral comparison study. Photodermatol Photoimmunol Photomed 2013;29:27-33. [Crossref] [PubMed]
- Rattanakaemakorn P, Phusuphitchayanan P, Pakornphadungsit K, et al. Efficacy and safety of 308-nm excimer lamp in the treatment of scalp psoriasis: a retrospective study. Photodermatol Photoimmunol Photomed 2019;35:172-7. [Crossref] [PubMed]
- Xia HL, Jai M. Effects of Xiaobi Decoction on Psoriasis and serum expression level of TGF-β1 and SOD. Guiyang: Guiyang Traditional Chinese Medicine College 2010:23-5.
- Wen CH, Jia M, Zhang S, et al. Clinical study of Xiaobi decoction (empirical Min) in the treatment of psoriasis vulgaris. China Modern Medicine 2016;23:28-31.
- Wu R, Tang T, He AJ, et al. Effect of Qingre Liangxue Xiaopi Decoction on Regulatory T Cells and Cytokines in Patients with Psoriasis Vulgaris (Blood Heat Syndrome). Journal of Chinese Medicinal Materials 2017;40:2977-80.
- He AJ. Effects of Xiaobi Decoction on Psoriasis and serum expression level of TNF-α, sICAM-1, MCP-1. Guiyang: Guiyang Traditional Chinese Medicine College, 2010:20-30.
- Chen Q. Research Methodology of Chinese Medicine Pharmacology. Beijing: People’s Medical Publishing House, 2011:1262.
- Heckman CJ, Chandler R, Kloss JD, et al. Minimal Erythema Dose (MED) testing. J Vis Exp 2013.e50175. [PubMed]
- de Gálvez MV. Psoriasis Protects Against a Low Minimal Erythema Dose. Actas Dermosifiliogr 2017;108:798-9. [PubMed]
- Rodríguez-Granados MT, Estany-Gestal A, Pousa-Martínez M, et al. Is it Useful to Calculate Minimal Erythema Dose Before Narrowband UV-B Phototherapy? Actas Dermosifiliogr 2017;108:852-8. [PubMed]
- Han CX, Dang EL, Jin L, et al. Effects of narrow-band ultraviolet B on the expression of keratin 17 in keratinocytes. Chin J Dermatol 2014;47:271-4.
- Yue XP, Wang HW. Determination of minimum erythema dose on rabbit ear irradiated by 308 nm excimer laser. Chin J Lepr Skin Dis 2016;32:464-7.
- Zhang S, Liu HX, Ou Y. Research Progress on etiology and pathogenesis of psoriasis. J Dermatology and Venereology 2017;39:27-30.
- Hu WT, Jia M, Shi H. The Effect of Xiaobi Decoction on Pathologic Changes of Rat Psoriasis-like Skin Lesions Expression. Prac Integr Chin and Western Med 2017;17:1-4.
- Guo S, Shi L, Yan XB, et al. Study of Magui Decoction on Imiquimod-induced Psoriasis-like Lesions in Mice by Gavage J Chin Med Mater 2014;37:1049-52.
- Fei WM, Tang HY, Yang S, et al. Changes of Cutaneous Microcirculatory in Psoriasis. Chin J Derm Venereol 2018;06:714-7.
- Sharma A, Reddy MH, Sharma K, et al. Study of endothelial dysfunction in patients of psoriatic arthritis by flow mediated and nitroglycerine mediated dilatation of brachial artery. Int J Rheum Dis 2016;19:300-4. [Crossref] [PubMed]
(English Language Editor: J. Reynolds)