
Relationship between risk perception and lifestyle in ischemic stroke patients with H-type hypertension
Introduction
Ischemic stroke, which is also referred to as brain or cerebral ischemia, affects more people in China than any other type of stroke (1). Globally, stroke accounts for the highest proportion of all neurological diseases (47.3%) and the highest proportion of deaths (67.3%) (2). Risk factors of stroke include hypertension, diabetes, hyperlipidemia, smoking, alcoholism and so on (3). Hypertension is the most important risk factor for stroke (4). High plasma homocysteine (Hcy) is also an important risk factor for stroke. For patients with stroke combined high Hcy levels, the risk of stroke is at least 12 times higher than those with normal Hcy levels (5). When patients with hypertension are complicated with high Hcy, it is called H-type hypertension. The Chinese guidelines for the management of hypertension (2018 revision) (6) have listed H-type (with Hcy ≥10 µmol/L) hypertension as a critical risk factor for stroke.
Therefore, the recurrence risk of stroke patients with H-type hypertension is higher than that of patients with simple stroke, which is worthy of attention. Lack of studies to discuss whether the health behaviors of H-type hypertension patients with stroke were different from that of normal Hcy patients. The occurrence and recurrence of stroke can be prevented by adopting a healthy lifestyle and controlling risk factors (4,7). However, the lifestyle behaviors of stroke patients are still inferior (8). A study found that the health behavior of Chinese patients with hypertension and stroke was at a lower level, especially in the dimension of exercise (9).
Risk perception refers to an individual’s awareness of the risk factors associated with their disease. Proper risk perception helps to increase the risk awareness of patients and supports them to actively control the relevant risk factor(s) (10). However, stroke patients in China generally have a low level of knowledge regarding the risk factors for stroke (11), and few studies have described stroke patients’ perceptions of the risk factors of their disease.
Studies have shown that proper risk perception was accompanied by good lifestyle. However, there is a lack of studies to explore the relationship between patients' lifestyle and risk perception at different Hcy levels. In this study, we investigated and explored the relationship between risk perception and lifestyle in ischemic stroke patients with H-type hypertension, so as to provide reference for tailored stroke prevention interventions. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2012).
Methods
Subjects
From Sept. 2018 to Sept. 2019, the convenience sampling method was used to enroll newly admitted patients from the neurology departments of three large-scale general hospitals in Guangzhou. A total of 314 stroke patients were enrolled, and 71 patients in normal Hcy group, 243 patients in high Hcy group. The inclusion criteria were as follows: (I) diagnosed by a specialist as ischemic stroke and confirmed by brain computed tomography (CT) or magnetic resonance imaging (MRI); (II) complicated by essential hypertension; (III) ischemic stroke occurred within the past month; and (IV) the patient could take care of themselves before disease onset. The exclusion criteria were: (I) aphasia; and (II) with heart, liver and kidney dysfunction, respiratory failure, malignant tumor, and/or mental illness.
Blood sampling and laboratory tests
Three mL of plasma were drawn by venipuncture into 5-mL plain evacuated tubes when the patient is fasting in the early morning. Blood samples were collected and analyzed within 1 h. The concentration of Hcy was determined by chemiluminescence. According to Chinese guidelines for the management of hypertension (2018 revision) (6), Hcy ≥10 µmol/L were considered high Hcy.
Measurements
General data survey forms
A self-designed questionnaire was used to collect patient information including sex, age, educational background, family history of stroke, whether or not it was their first-ever stroke, accompanying stroke risk factors, and serum Hcy level. According to the Hcy level, the patients were divided into the high Hcy group (Hcy ≥10 µmol/L) and the normal Hcy group.
Essen stroke risk score (ESRS)
The ESRS is used to predict the risk of stroke recurrence after an initial episode of ischemic stroke (3). The ESRA takes eight risk factors into account including age, hypertension, diabetes, previous myocardial infarction (MI), other cardiovascular disease (except MI and atrial fibrillation), peripheral arterial disease, smoking, and previous transient ischemic attack (TIA), and has a total score of 9 points. Accordingly, patients are classified as having low [0–2], intermediate [3–6], or high [7–9] risk. Our investigators scored the patients according to their responses on the questionnaire form.
Questionnaire on knowledge of stroke risk factors
The Questionnaire on Knowledge of Stroke Risk Factors, which was developed by Wan et al. (12), was used to measure patients’ perceptions of stroke risk factors. In addition to the risk factors assessed by the ESRS, this questionnaire also covered factors including hyperlipidemia, obesity, alcoholism, and family history of stroke. Risk perception was self-reported by patients according to questionnaire questions. The patients were asked, “Which of the following factors increase the risk of stroke?” Multiple questions were given, each containing a different risk factor, and might answer “Yes”, “Uncertain”, or “No”. A correct answer scored 1 point and a wrong answer scored 0 points. If a patient had an accompanying risk factor and correctly answered that it was a stroke risk factor, then the patient’s risk factor was judged to be “perceived”; otherwise, it was regarded as “unperceived”. The following formulas were applied:
Perception rate of a risk factor = the number of patients who have perceived the risk factor/the total number of patients with the risk factor ×100%.
Awareness rate of a risk factor: the number of patients who correctly identified the risk factor/the number of subjects (including patients with/without this risk factor) ×100%. The scale had a Cronbach’s α coefficient of 0.86 (12). In the current study, the Cronbach’s α coefficient was 0.82.
Health behavior scale for stroke patients
Patients’ lifestyle behaviors were assessed using the health behavior scale for stroke patients, which was adapted by Wan et al. This scale has seven dimensions [i.e., exercise, nutrition (including low-fat diet and low-sugar diet), low-salt diet, smoking cessation, alcohol restriction, medication, and blood pressure monitoring] and 25 items. The health behavior scale applies the Likert scale (rated as 1= never, 2= sometimes, 3= usually, and 4= always), with a higher score indicating a better lifestyle. The scale had a Cronbach’s α coefficient of 0.88 (12). In the current study, the Cronbach’s α coefficient was 0.83.
Ethical consideration
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethical committee of the Third Affiliated Hospital of Sun Yat-sen University [approval number: EC-TAHSYU (2018)02-421-01]. Signed informed consent was obtained from each participant after they had been given a brief explanation of the purpose of this study.
Data collection
Newly admitted patients completed a questionnaire-based survey before they received their health education. The objectives and methods of the survey were explained to the patients by trained staff. Then, the participants completed the questionnaire forms on the spot, which were collected immediately. All of the 340 questionnaires that were distributed were recovered. Among them, 314 forms (92.4%) included the results of Hcy measurement.
Statistical analysis
Statistical analysis was performed using the SPSS 25.0 software package. Statistical analysis methods included descriptive analysis, chi-square test, and t-test. Descriptive analysis was used to describe general information, ESRS factors, perception rate of risk factors and HBS-SP score. Chi-square test was used to compare general information, risk factors and perception rate of risk factors between normal Hcy group and high Hcy group. T-test was used to compare HBS-SP score between normal Hcy group and high Hcy group, as well as HBS-SP score between perceived group and non-perceived group.
Results
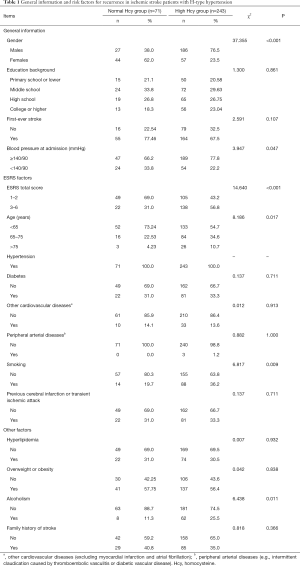
General information and risk factors for recurrence in ischemic stroke patients with H-type hypertension
In total, 314 ischemic stroke patients were found to have hypertension. As shown in Table 1, patients in the high Hcy group had significantly higher ESRS scores (3–6 points) than patients in the normal Hcy group, and were more likely to be older, to smoke, and to have alcoholism (all P<0.05).
Full table
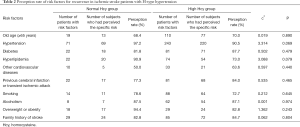
Perception rate of risk factors for recurrence in ischemic stroke patients with H-type hypertension
As shown in Table 2, the perception rates of existing risk factors among patients in the high Hcy group ranged from 63.6–90.5%, which showed no statistically significant difference from those in the normal Hcy group.
Full table
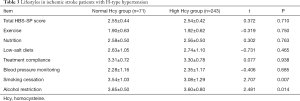
Lifestyles in ischemic stroke patients with H-type hypertension
Table 3 shows that the total lifestyle score of ischemic stroke patients with H-type hypertension was (2.54±0.42) points (range, 1–4 points), with the exercise dimension having the lowest score. The high Hcy group had inferior scores for smoking cessation and alcohol restriction compared to the normal Hcy group (both P<0.05).
Full table
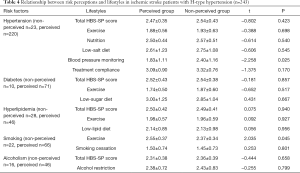
Relationship between risk perception and lifestyle in ischemic stroke patients with H-type hypertension
In the high Hcy group (Table 4), the perceived group had a better lifestyle compared to the non-perceived group; however, the only significant difference between the groups was found in blood pressure monitoring compliance (P<0.05). Among smokers, the overall lifestyle behaviors of the non-perceived group were superior to those of the perceived group (P<0.05); however, no statistical differences were observed between groups with regard to the other dimensions.
Full table
Discussion
Risk factors for recurrence in ischemic stroke patients with H-type hypertension
In our current study, the high Hcy group had a significantly higher proportion of patients with a high-risk ESRS score than the normal Hcy group. Possible explanations for this may be that the incidence of modifiable risk factors for stroke is increasing with China’s rising socioeconomic status. Hypertension is the leading cause of stroke (4), and in China, 75% of hypertensive patients are accompanied by high homocysteine (HHcy) levels (13). Synergistically, hypertension and high Hcy increase the risk of stroke 12-fold (5,14). A cohort study found when Hcy levels increased to 10 to 15 µmol/L, the risk of stroke and hypertension was significantly increased (15). The results of an 18-month follow-up study showed that the rate of stroke recurrence in patients with high levels of Hcy was 21%, while the recurrence of stroke in the normal Hcy group was only 6.8% (16). Furthermore, possible explanations for Hcy increase may be that the elevated plasma Hcy level is related to (I) excessive methionine intake; (II) dietary folic acid, vitamin B6, or B12 deficiency; and/or (III) genetic factors. Compared with those in Western countries, Chinese populations tend to stir-fry vegetables and eat fewer fruits and vegetables, which can easily lead to folic acid deficiency and cause high levels of Hcy in the plasma (17). Moreover, dyslipidemia, smoking, and alcohol consumption can also increase the concentration of plasma Hcy (17).
In our current study, 77.4% of ischemic stroke patients with hypertension had a high Hcy level, which was close to the proportion of 75% in the literature (17), suggesting that the measurement of Hcy level is essential in patients with stroke and hypertension. Routine Hcy measurement in patients with hypertension and stroke is crucial for secondary stroke prevention (17). Approximately 70% of patients with ischemic stroke have elevated blood pressure, and 40% of patients with ischemic stroke have hyperglycemia, which is associated with a poor prognosis (1). Among the ischemic stroke patients with H-type hypertension in the current study, the prevalence rates of diabetes and hyperlipidemia were 33.3% and 30.5%, respectively, which were remarkably higher than those for diabetes (10.9%) (18) and hyperlipidemia (19) in the general population. Therefore, ischemic stroke patients with H-type hypertension have a high risk of stroke recurrence and should be the top priority population for secondary prevention of stroke.
Perception of risk factors for recurrence in ischemic stroke patients with H-type hypertension
The awareness rates of the risk factors among the newly admitted ischemic stroke patients with hypertension prior to receiving health education were as follows: hypertension (92.0%), alcohol consumption (84.4%), hyperlipidemia (75.5%), previous cerebral infarction (75.5%), smoking (72.3%), diabetes (69.1%), old age (66.6%), family history of stroke (61.8%), heart disease (58.3%) and peripheral arterial disease (48.7%). These awareness rates were similar to those reported by Soomann et al. (20), but far higher than those described by Wang et al. (21) (obtained before the discharge of stroke patients) and slightly higher than those of Faiz et al. (22) (obtained 12 months after the discharge of stroke patients). Therefore, health education on the risk factors of stroke has been successful in China, which may be attributed to the strengthening of health education in hospitals and efficient efforts to raise awareness in the media, including through radio, television, and the Internet. Notably, in 20.9% of our ischemic stroke patients, hypertension was discovered after disease onset, which is similar to the results reported in the literature (20,23). Together, these findings suggest that screening for hypertension is critical for the primary prevention of stroke.
Risk perception, which refers to the cognitive evaluation of the accompanying risk factors by an individual with a disease, is different from risk awareness. Patients who are aware of a particular risk factor may not necessarily perceive it as a risk factor for their own disease. Many studies have been conducted on the rate of risk awareness in stroke patients; however, few studies have investigated whether stroke patients perceive their accompanying risk factors to be risk factors for stroke recurrence. In our current study, ischemic stroke patients with H-type hypertension had a perception rate of 63.6–90.5% for their existing risk factors, which showed no statistical difference from the rate in the normal Hcy group. This suggests that the perception of risk factors in ischemic stroke patients with H-type hypertension needs to be improved.
Lifestyle in ischemic stroke patients with H-type hypertension
Stroke can be prevented through a healthy lifestyle (24). However, stroke patients often have unhealthy lifestyle habits (8,25). In our current study, the total score of the lifestyle of ischemic stroke patients with H-type hypertension was (2.54±0.42) points; however, the exercise dimension had the lowest score, ranging between “never” and “sometimes”, which was consistent with the literature (8,26,27). An appropriate amount of exercise can reduce the risk of stroke (28). The smoking rate in our high Hcy group was 36.2%, which was higher than that (19.7%) in the normal Hcy group (P<0.05) and higher than those (23–24%) reported in stroke patients in international studies (20,29). The alcohol consumption rate in our high Hcy group was 25.5%, which was significantly higher than that (11.3%) in the normal Hcy group (P<0.05), close to those (27%) reported in stroke patients in international studies (20,29), and lower than those (30.11–42.11%) in ischemic stroke patients in a Chinese study (30). The risk of stroke is almost doubled by smoking, and it can also be increased by excessive drinking (28). Therefore, health education on smoking cessation and alcohol restriction must be strengthened for ischemic stroke patients with H-type hypertension.
The relationship between risk perception and lifestyle in ischemic stroke patients with H-type hypertension
Disease perception is a patient’s cognitive evaluation of a specific disease from which they suffer, and it can affect the patient’s adherence to treatment and lifestyle behaviors (10). Correct evaluation of the accompanying risk factors as the risk factors of the disease can help to improve the patient’s risk awareness and thus motivate them to actively cooperate with efforts to control such risk factors (10). In our current study, the perceived group had a superior lifestyle than the non-perceived group; however, the only significant difference between the groups was found in compliance with blood pressure monitoring (P<0.05). Thus, patients in perceived group have improved their lifestyles to a certain extent through the perception of risk factors, although further improvements still need to be made. However, the lifestyles of subjects who perceived diabetes, hyperlipidemia, smoking, and alcohol consumption to be risk factors did not differ significantly from those of patients in the unperceived group.
For patients with high Hcy level, healthy lifestyles are vital for controlling hypertension. In the current study, the proportion of patients with abnormal blood pressure was higher in the high Hcy group than in the normal Hcy group, which might be explained by a lower level of risk awareness. Possible explanations for this are as follows: (I) although Hcy is routinely measured in the neurology departments in almost all hospitals, the majority of patients neither understand nor care about the result of Hcy measurement; (II) awareness of this indicator is also low among medical staff and, consequently, its clinical significance is generally not explained to patients. Therefore, the lifestyle behaviors of ischemic stroke patients with H-type hypertension need to be improved. Although risk perception has not yet been shown to exert a significant impact on lifestyle. Health education strategies should focus more on the risk factors of stroke to improve patients’ risk perception. Finally, multidisciplinary management should be adopted to improve patients’ lifestyles and thus prevent stroke recurrence.
Acknowledgments
We thank all the patients who participated in this study. Thank you to Miao-Miao Mo, Ying-Mei Zhang, Cui-Ling Ou, Zhou-Yuan Peng, Wei-Jing Sui, and Ying Liu for assisting with data collection. Thank you to Meng-Yao Wang, Min-Jie Chen, and Susan H. Neidlinger for their editorial assistance.
Funding: This study was funded by Guangdong Science and Technology Department, the Guangdong Special Program for Scientific Development (No. 2016A020215039, Li-Hong Wan, PI) and Guangzhou Special Program for Scientific Knowledge (No. 201609010050, Li-Hong Wan, PI).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2012
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2012
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2012). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was obtained from the ethical committee of the Third Affiliated Hospital of Sun Yat-sen University [approval number: EC-TAHSYU (2018)02-421-01]. All participants were given a brief explanation of the purpose of this study, and signed informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chen Z, Jiang B, Ru X, et al. Mortality of Stroke and Its Subtypes in China: Results from a Nationwide Population-Based Survey. Neuroepidemiology 2017;48:95-102. [Crossref] [PubMed]
- GBD 2015 Neurological Disorders Collaborator Group. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol 2017;16:877-97. [PubMed]
- Weimar C, Diener HC, Alberts MJ, et al. The Essen stroke risk score predicts recurrent cardiovascular events: a validation within the REduction of Atherothrombosis for Continued Health (REACH) registry. Stroke 2009;40:350-4. [Crossref] [PubMed]
- Wang W, Jiang B, Sun H, et al. Prevalence, Incidence, and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480 687 Adults. Circulation 2017;135:759-71. [Crossref] [PubMed]
- Kwon HM, Lee YS, Bae HJ, et al. Homocysteine as a predictor of early neurological deterioration in acute ischemic stroke. Stroke 2014;45:871-3. [Crossref] [PubMed]
- Chinese committee of hypertension prevention and control guidelines, hypertension alliance (China), Chinese society of cardiovascular medicine, et al. Chinese guidelines for hypertension prevention and control (2018 revision). Chinese Journal of Cardiovascular Medicine 2019;24:24-56.
- Algra A, Wermer MJ. Stroke in 2016: Stroke is treatable, but prevention is the key. Nat Rev Neurol 2017;13:78-9. [Crossref] [PubMed]
- Wan LH, Zhang XP, You LM, et al. The Efficacy of a Comprehensive Reminder System to Improve Health Behaviors and Blood Pressure Control in Hypertensive Ischemic Stroke Patients: A Randomized Controlled Trial. J Cardiovasc Nurs 2018;33:509-17. [Crossref] [PubMed]
- Wu Y, Gao B, Zhong S, et al. Analysis on the status quo and influencing factors of healthy lifestyle of stroke rehospitalized patients. J of Nursing Science 2018;14:29-31.
- Mosleh SM, Almalik MM. Illness perception and adherence to healthy behaviour in Jordanian coronary heart disease patients. Eur J Cardiovasc Nurs 2016;15:223-30. [Crossref] [PubMed]
- Yang J, Zheng M, Chen S, et al. A survey of the perceived risk for stroke among community residents in western urban China. PLoS One 2013;8:e73578. [Crossref] [PubMed]
- Wan LH, Zhao J, Zhang XP, et al. Stroke prevention knowledge and prestroke health behaviors among hypertensive stroke patients in mainland china. J Cardiovasc Nurs 2014;29:E1-9. [Crossref] [PubMed]
- Zhong C, Lv L, Liu C, et al. High homocysteine and blood pressure related to poor outcome of acute ischemia stroke in Chinese population. PLoS One 2014;9:e107498. [Crossref] [PubMed]
- Wang HL, Tan S, Song B, et al. Correction of H-type Hypertension and Prognosis of Ischemic Stroke. Chinese Journal of Zhonghua Yi Xue Za Zhi 2012;92:1183-6. [PubMed]
- Feng Y, Kang K, Xue Q, et al. Value of plasma homocysteine to predict stroke, cardiovascular diseases, and new-onset hypertension: A retrospective cohort study. Medicine 2020;99:e21541. [Crossref] [PubMed]
- Wu XQ, Ding J, Ge AY, et al. Acute phase homocysteine related to severity and outcome of atherothrombotic stroke - reply. Eur J Intern Med 2014;25:e15. [Crossref] [PubMed]
- Zeng R, Xu CH, Xu YN. The effect of folate fortification on folic acid-based homocysteine-lowering intervention and stroke risk: a meta-analysis. Public Health Nutr 2015;18:1514-21. [Crossref] [PubMed]
- Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017;317:2515-23. [Crossref] [PubMed]
- Huang Y, Gao L, Xie X, et al. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr 2014;12:28. [Crossref] [PubMed]
- Soomann M, Vibo R, Korv J. Do Stroke Patients Know Their Risk Factors? J Stroke Cerebrovasc Dis 2016;25:523-6. [Crossref] [PubMed]
- Wang MD, Wang Y, Mao L, et al. Acute stroke patients' knowledge of stroke at discharge in China: a cross-sectional study. Trop Med Int Health 2018;23:1200-6. [Crossref] [PubMed]
- Faiz KW, Labberton AS, Thommessen B, et al. Stroke-Related Knowledge and Lifestyle Behavior among Stroke Survivors. J Stroke Cerebrovasc Dis 2019;28:104359. [Crossref] [PubMed]
- Chen MJ, Wu CC, Wan LH, et al. Association Between Medication Adherence and Admission Blood Pressure Among Patients With Ischemic Stroke. J Cardiovasc Nurs 2019;34:E1-8. [Crossref] [PubMed]
- Brenner DA, Zweifler RM, Gomez CR, et al. Awareness, treatment, and control of vascular risk factors among stroke survivors. J Stroke Cerebrovasc Dis 2010;19:311-20. [Crossref] [PubMed]
- Wan LH, Zhang XP, Mo MM, et al. Effectiveness of Goal-Setting Telephone Follow-Up on Health Behaviors of Patients with Ischemic Stroke: A Randomized Controlled Trial. J Stroke Cerebrovasc Dis 2016;25:2259-70. [Crossref] [PubMed]
- Wang MY, Shen MJ, Wan LH, et al. Effects of a Comprehensive Reminder System Based on the Health Belief Model for Patients Who Have Had a Stroke on Health Behaviors, Blood Pressure, Disability, and Recurrence From Baseline to 6 Months: A Randomized Controlled Trial. J Cardiovasc Nurs 2020;35:156-64. [Crossref] [PubMed]
- Ihle-Hansen H, Langhammer B, Lydersen S, et al. A physical activity intervention to prevent cognitive decline after stroke: Secondary results from the Life After STroke study, an 18-month randomized controlled trial. J Rehabil Med 2019;51:646-51. [Crossref] [PubMed]
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-492. [Crossref] [PubMed]
- Shravani K, Parmar MY, Macharla R, et al. Risk factor assessment of stroke and its awareness among stroke survivors: A prospective study. Adv Biomed Res 2015;4:187. [PubMed]
- Xia X, Yue W, Chao B, et al. Prevalence and risk factors of stroke in the elderly in Northern China: data from the National Stroke Screening Survey. J Neurol 2019;266:1449-58. [Crossref] [PubMed]
(English Language Editors: J. Chapnick and J. Reynolds)


