
The mental health of Chinese healthcare staff in non-epicenter of COVID-19: a cross-sectional study
Introduction
Background
Medical staff, as the primary staff in a hospital, are responsible for providing health services to patients, and their health status provides a solid foundation for the medical system. Zou et al. (1) have argued that medical workers are under considerable work-related and psychological pressure because of the complexity of the Chinese medical system and environment. van Agteren et al. (2) explained that healthcare workers are at high risk for mental health problems, and the stressful environment can affect their wellbeing. Nevertheless, the professional knowledge of medical staff causes their mental health status to be more easily overlooked than that of the general public (3). As Hall et al. (4) pointed out, staff wellbeing is vital to patient safety interventions. If staff have mental health problems, it will affect the quality of medical service (5).
In January 2020, COVID-19 appeared in the city of Wuhan in central Hubei Province, China (6). Unfortunately, the virus appeared to spread by close person-to-person contact. More than 42,000 people in China had been infected by 11 February (7). The rapid spread of the virus sparked fears of a nationwide outbreak. An outpouring of information began. Dissemination of information about a disease and health advice may reduce the spread of a disease during a public crisis such as an epidemic. Nevertheless, Blakey and Abramowitz (8) and Shigemura et al. (9) found that excessive (or sensational) news reports can also exaggerate the threat of the disease and even trigger anxiety in the public, including healthcare workers. Medical staff were at high risk in the early stage because of the lack of forewarning that they might come into contact with someone with the virus. Over 1,700 medical staff were infected with the virus in several hospitals across the country (10). Until 12 February, the Chinese government also rushed relief supplies and more than 21,000 medical personnel to the area (11) where the virus outbreak was most severe (Hubei Province). Medical staff across China were on standby, ready to go to the epicenter of the outbreak to work on the frontline at a moment’s notice. They were also at serious risk of infection in local hospitals. Therefore, each medical worker during this time was under more pressure than workers during previous virus outbreaks. Subsequently, the Chinese authorities released a document (12) listing measures to care for medical staff, one of which was to provide mental health services for medical workers. The psychological effects during the pandemic such as fear, anxiety, depression, post-traumatic stress disorder (PTSD), a moral injury might occur. During the COVID-19, many medical workers show high levels of anxiety and worry as well. The mental health of healthcare workers is extremely important in the battle against the virus, and their psychological status will affect medical service delivery.
The idea of the study stem from two reasons. Firstly, China is a country with a large area, and there are great differences among different regions. There might be risks of underestimating and overestimating the prevalence of the mental health of medical staff. To allocate resources accurately and provide psychological support for employees promptly, the authors' conducted a baseline survey on the psychology of employees in a hospital. Secondly, an only child policy (birth control policy) exists since the 1980s in China. A family is permitted to have an only child according to the policy. The only child generation is quite spoiled by parents during their development. Now, they have already become the primary workforce in society, medical workers are not exceptionally to play an important role. It's hard to predict whether they will be psychologically resilient to emergencies. Hence, the authors' conducted a baseline survey on the psychology of employees in a hospital.
We present the following article in accordance with the SURGE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2041).
The objective of the study
There were several medical staff in the target hospital that were sent to Wuhan to treat patients. This study investigated the psychological health of medical staff in a special tertiary hospital, and analyzed their psychological status during the outbreak stage of the epidemic and the association with relevant factors. It is hoped that this study can provide a basis for the development of corresponding psychological intervention measures in the future.
Methods
Study design and participants
This study was a cross-sectional survey. It was approved by the Chengdu Women and Children’s Central Hospital Ethics Review Board. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the participants. Staff from the Women and Children’s Hospital were recruited in February 2020.
In Chengdu, a city with more than 14,000,000 people in Southwest China (13), the first COVID-19 case was reported on 21 January 2020 in another tertiary hospital (14). By 20 February, there were 11 suspected and probable cases, but none of the confirmed cases had occurred in the target hospital, which has 1,800 beds and 2,923 workers (including ancillary staff). All medical workers (2,439) at the tertiary hospital who were actually on service during the outbreak were invited to participate. This hospital has a small proportion of men. Three hundred men are working in the target group, only about 12.3%. The study covered a period of just over a week (from 10 February to 16 February), the time when it was declared that the hospital would officially accept suspected COVID-19 patients. The inclusion criteria were medical staff in the hospital without mental illness. The exclusion criteria were ancillary staff and people who left their position for a long period of time.
After providing voluntary written consent, participants completed an anonymous, self-rated questionnaire that took 10 to 20 minutes, and no compensation was offered. Each person could respond to the questionnaire only once. All participants were required to complete the survey within a week. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
There are three psychological counselors in the research group. They provide some psychological treatments for people who have severe anxiety symptoms, including telephone interviews and cognitive therapy.
Study measures
The questionnaire consisted of 3 parts: sociodemographic data, the Psychological Questionnaire on Emergency Events in Public Health (PQEEPH), and the Generalized Anxiety Disorder-7 (GAD-7) scale.
PQEEPH
The psychological response to COVID-19 was assessed using the PQEEPH. This instrument was developed by Gao et al. (15) in China during the severe acute respiratory syndrome (SARS) outbreak in 2003. It has 5 dimensions: depression, neurasthenia, fear, compulsion anxiety, and hypochondriasis. There are 27 items in total. The extent (none, mild, moderate, or severe) and frequency (occasionally, sometimes, regularly, or always) of the emotional reaction were scored on a 4-point scale from 0 to 3. The total score of each dimension divided by the number of items is the score for the dimension. Zhang et al. (16) also used this questionnaire to analyze the psychological status and coping style of nurses during the influenza A (H1N1) epidemic.
GAD-7
Mental health status was measured using the GAD-7. The 7 items of the GAD-7 were developed by Spitzer et al. (17) The questionnaire asks how often the respondent has suffered from the 7 core symptoms of GAD within the last 2 weeks. The items are (I) feeling nervous, anxious, or impatient, (II) not being able to control worry, (III) feeling fear and anxiety related to a series of events or activities, (IV) trouble relaxing, (V) difficulty concentrating, (VI) becoming easily annoyed or irritability, and (VII) feeling anxiety and worry that terrible things might happen. The response options include ‘not at all’, ‘on some days’, ‘on more than half of the days’, and ‘almost every day’ (scored 0–3, with a total score ranging from 0 to 21) (18). A threshold score of 10 is recommended in the GAD-7 (17).
Data collection
The questionnaire was distributed to a WeChat (a phone communication application widely used in China) group through a QR code created by an online survey website (Questionnaire Star) over the internet (to which all the medical staff in the hospital had free access). Data were collected and analyzed by 3 trained researchers.
Data analysis
The researchers screened the data and then input the valid data into the computer for analysis. SPSS version 23.0 was employed to analyze the data. A P value <0.05 was considered statistically significant. Descriptive statistics such as frequency, percentage, mean, and standard deviation were used to analyze sociodemographic characteristics and the PQEEPH and GAD-7 scores. Independent samples t-tests were conducted for gender and family members to examine the corresponding factors, and one-way analysis of variance (ANOVA) was conducted for the other indicators to compare the influencing factors. To explore the sources of differences in age, marital status, and educational background, a post hoc test was carried out using the least significant difference (LSD) test.
Results
The sociodemographic characteristics of the respondents
There were 2,439 medical staff in the target group, and 2,143 workers participated in the study. Twenty-four workers refused to respond to the questionnaire, 31 participants refused to allow the use of their information for research, and one of the questionnaires was not completed carefully. The final number of respondents was 2,087. Valid responses were obtained from 1,890 women and 197 men, whose mean age was 31.3 years (range, less than 21 to more than 60 years). Most of the respondents were nurses (1,070/2,087, 51.3%), doctors (339/2,087, 16.2%), or paramedical staff (678/2,087, 32.5%). Table 1 shows the sociodemographic characteristics of the respondents.

Full table
The psychological response of medical staff and results of the correlative factor analysis of the PQEEPH
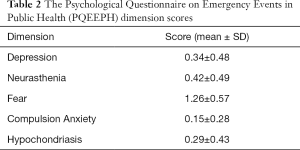
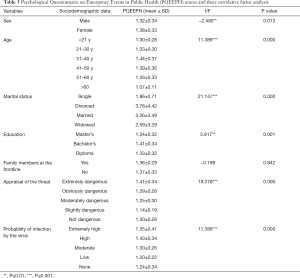
The PQEEPH scale investigates individuals’ emotional responses to public health emergencies. In this study, the Cronbach’s α coefficient of internal consistency for the PQEEPH was 0.881. The average score in this study was 0.49 (SD =0.36). Table 2 presents the average scores of the 5 dimensions. Of the participants, 89.7% had a PQEEPH score lower than 1 point, 10% scored 1 point to 2 points, and 0.3% scored higher than 2 points. There was a significant difference in PQEEPH scores by sociodemographic variables such as sex, age, marital status, and education. A significant difference in PQEEPH scores was found between females and males (t=−2.48, P value <0.01). Additionally, scores differed significantly by age (F =11.388, P value <0.001), and the 31–40 years old group of medical workers had the highest score. Marital status (F =21.147, P value <0.001) and educational background (F =3.817, P value <0.001) also led to significantly different PQEEPH scores. Widowed people had the highest scores, followed by divorced people. Medical staff with a bachelor’s degree had higher scores than those with a master’s degree or diploma. However, there was no significant difference in the scores based on whether family members were frontline workers in the fight against the epidemic. Finally, there were significant differences by appraisals of the threat (F =9.378, P value <0.001) and of the probability of infection by the virus (F =61.856, P value <0.001). The scores of workers who appraised the threat from the virus as high risk were significantly higher than those of workers who appraised the risk as lower. Additionally, a probably of infection appraisal of ‘extremely high’ was associated with the highest score, followed by ‘high’, ‘moderate’, and ‘low’. The details are shown in Table 2 and Table 3.
Full table
Full table
The psychological response of medical staff and the correlative factor analysis of the GAD-7
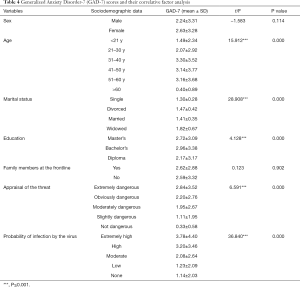
In this study, the Cronbach’s α coefficient of internal consistency of the GAD-7 was 0.917. The average score in this study was 2.59 (SD =3.29). A total of 4% of the respondents reported GAD-7 scores greater than or equal to 10 points. Table 4 presents the GAD-7 scores and the demographic variables. GAD-7 scores differed significantly by sociodemographic variables such as age (F =15.912, P value <0.001), marital status (F =8.908, P value <0.001), and education (F =4.128, P value <0.001). Those younger than 31 years had lower scores than those in other age groups. Widowed people had the highest scores, followed by divorced people. Medical staff with a bachelor’s degree had higher scores than those with a master’s degree or diploma. There were significant differences by appraisals of the threat (F =6.591, P value <0.001) and of the probability of infection by the virus (F =36.840, P value <0.001). The analysis showed that those who considered the threat ‘high risk’ had significantly higher scores than those who appraised the threat as lower. Rating the probably of infection ‘extremely high’ was associated with the highest score, followed by ‘high’, ‘moderate’, and ‘low’. However, there was no significant difference in the scores based on sex or whether the family members were at the frontline of the fight against the virus.
Full table
Discussion
Since COVID-19 emerged, it has rapidly spread in Hubei Province, China, and to other countries, leading to tens of thousands of cases and thousands of deaths, causing a certain level of public panic (19). Medical staff are not exceptionally terrified. However, the results of our study showed that 65.6% of medical professionals perceived the threat posed by the virus as extremely dangerous. This is the first study assessing the psychological status of all medical staff in a special hospital (providing services for women and children only) during the COVID-19 outbreak. The rapid and unexpected spread of COVID-19 could be regarded as an acute, traumatic public health event. Most of the existing literature on the mental health of Chinese medical staff focuses on peacetime or other natural disasters or catastrophic events (16,20-23). Furthermore, most of these studies were conducted in general hospitals, and few were conducted in specialized hospitals, especially women and children’s hospitals. There is a psychological out-patient department in the hospital. The Labor Union of the hospital invites the psychotherapists to conduct psychological counseling and support for medical staff each year. Those with severe mental problems have left their jobs, and the existing workers have not shown any psychological problems before the outbreak of the COVID-19.
The psychological status of tertiary hospital workers
The psychological status of the medical staff was relatively good in this study performed in a tertiary hospital. The results from several studies (1,16,23) in China reported that the mental health of medical staff was good. In contrast, some researchers (24-26) identified that medical staff had worse mental health compared to those in other occupations. The psychological status of medical staff might differ by specialty, location, level of hospital, and demographic characteristics (27,28). Moreover, the outbreak of the virus occurred during the Chinese Spring Festival holiday. During this time, family members could gather and support each other. Additionally, work pressure was lower than ordinary because the number of patients declined markedly during the outbreak of the virus. Individuals without serious diseases were advised not go to hospital to reduce potential virus spread. Additionally, according to the control policy of the government, more than half the medical staff of the hospital were required to stay at home. Therefore, the probability of infection by the virus was low when they participated in the survey. Moreover, residents in this region have experienced several large natural disasters in recent years, such as the Wenchuan earthquake and Yushu earthquake. Thus, the medical staff, and even the public, were better equipped mentally to cope as the situation unfolded.
The factors influencing the mental health of medical staff according to the PQEEPH results
Public health emergencies can cause fear, which is an instinctive response that helps individuals protect themselves. The average score of the fear dimension of the PQEEPH was 1.26 (SD =0.57). This is consistent with a study of COVID-19 conducted by Jin et al. (19) showing that the spread of the virus leads to a certain level of public panic. Similarly, other studies (20,22) showed that the most common reaction of medical staff to SARS in 2003 was fear and anxiety. The reaction of men was better than that of women, as women reported a higher score than men on the PQEEPH. This is consistent with other studies (1,21,23,29) indicating that women’s mental health is worse than men’s. Traditional Chinese values dictate that women must undertake more responsibility in the family, such as housework and raising children. Thus, they are at high risk of psychological problems. In addition, men are more likely to adopt a positive attitude toward emergencies than women (30). The 31–40 age group scored highest on the survey. This might be because people of this age usually have to take care of the elderly and children at home and face the pressure of promotion at work (23,31). Many issues need to be considered when emergencies arise. The staff reported high scores when they felt the virus was extremely dangerous or assessed the probability of infection as extremely high. This shows that cognition might affect people’s emotional reactions.
The factors influencing the mental health of medical staff according to the GAD-7 results
A total of 4% of participants reported high scores on the GAD-7 in this study. In a large-sample survey, Ouyang (28) also found that the incidence of severe anxiety in medical staff was 4.3%. The level of anxiety increased with age. However, the results differed from those of a study by Tu et al. (24) that showed that elderly staff had low anxiety levels because they were familiar with the culture and the environment, and had sufficient economic support. Nevertheless, the younger staff members belong to the ‘only child’ generation. They experience less pressure because they have more support from their parents, including economic and social support. They prefer to express their emotions rather than restrain themselves. The 31–40 years old group demonstrated a higher level of anxiety than the other age groups. This might be because people of this age face more pressure not only at home but also at work (23,31). Regarding education level, anxiety was highest among those with a bachelor’s degree, followed by those with a master’s degree and those with a diploma. Educational background influences the mental health of individuals by influencing their cognitive and coping styles. However, the insufficient sample size of master’s degree holders might affect the results. The staff reported a high level of anxiety when they felt the virus was extremely dangerous or assessed the probability of infection as extremely high. Therefore, individuals who think that they are in danger are more likely to develop anxiety.
Worry or anxiety about COVID-19 should not necessarily be regarded as pathological or in need of professional treatment. Anxiety will reduce over time as the COVID-19 is resolved in China. The results demonstrate that majority of medical professionals in the hospital are at good level of mental health. The authors summed up the invention and the hospital’s treatment for well-being of the healthcare workers during COVID-19. There are several practical measures to enhance the well-being of the staff during the pandemic. The most important is the hospital leaders always provide staff high-grade quality information and advice from experts and the government to avoid the crisis that fear and panic was spread by rumors, misinformation, and confusing information. Secondly, the hospital leaders provide adequate support to employees. For instance, feeling prepared, and properly instructed, having access to the relevant protecting equipment, and access to psychological support, all help to lighten fears and can help to decrease the impact of psychological suffering on healthcare workers. In addition to these practical measures, consideration should also be given to establishing an ongoing program of mental health monitoring in the hospital for impacted medical staff.
For those who are in a heightened state of anxiety or fear, it would typically alleviate once the virus is contained, and the majority did not require clinical treatment. They are not treated with drugs, and these staffs with severe psychological problems are relieved through the interview and cognitive therapy.
Strengths and limitations
The strength of this study was that the online questionnaire was easily accessed. However, nonprobability convenience sampling might have resulted in sampling bias, and the findings may not be representative of all medical staff across all levels of hospitals. In particular, there are fewer male staff than female staff in the hospital. Another important limitation of the study is that medical workers who suffer from severe symptoms of psychological disturbance are reluctant to participate or report because of Chinese culture. Hence, the true percentage of people with clinical anxiety and depressive symptoms may have been underestimated.
Conclusions
In summary, medical staff in the women and children’s hospital had a low rate of psychological distress compared to that of the general population. Female staff, those 31–40 years old, and those who are widowed were found to have a high level of anxiety and therefore need more support. The cognition of medical workers to perceived threat might affect their emotional reactions. Treatment to decrease their anxiety during emergency event outbreaks should include communication strategies. Ongoing efforts should be made to understand the associations reported here in order to assist leaders in developing policies to improve the mental health of medical staff in special hospitals during the COVID-19 outbreak and other emergency outbreaks.
Acknowledgments
We thank our team and colleagues at Chengdu Women and Children’s Central Hospital for their assistance.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2041
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2041
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2041). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Chengdu Women and Children’s Central Hospital Ethics Review Board. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zou Z, Huang Y, Wang J, et al. The mental health of medical staff in general hospital. Practical Journal of Clinical Medicine 2015;12:78-81.
- van Agteren J, Iasiello M, Lo L. Improving the wellbeing and resilience of health services staff via psychological skills training. BMC Res Notes 2018;11:924. [Crossref] [PubMed]
- Su C, Lin X, Lin S, et al. The mental health status of 546 medical staff. Hainan Medical Journal 2013;24:3094-5.
- Hall L, Johnson J, Watt I, et al. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PloS One 2016;11:e0159015. [Crossref] [PubMed]
- Hua R. A study on the mental health of medical staff. Preventive Medicine Tribune 2016;22:791-4.
- Health Ministry’ emergency services office, The report of Wuhan Health Committee on unknown virus pneumonia. 2020 Jan 11. Available online: http://www.nhc.gov.cn/xcs/yqtb/202001/1beb46f061704372b7ca41ef3e682229.shtml
- Health Ministry’ emergency services office, The epidemic situation of the novel coronavirus by 10th Feb. 2020 Feb 11. Available online: http://www.nhc.gov.cn/xcs/yqtb/202002/4a611bc7fa20411f8ba1c8084426c0d4.shtml
- Blakey SM, Abramowitz JS. Psychological Predictors of Health Anxiety in Response to the Zika Virus. J Clin Psychol Med Settings 2017;24:270-8. [Crossref] [PubMed]
- Shigemura J, Harada N, Tanichi M, et al. Rumor-Related and Exclusive Behavior Coverage in Internet News Reports Following the 2009 H1N1 Influenza Outbreak in Japan. Disaster Med Public Health Prep 2015;9:459-63. [Crossref] [PubMed]
- Ministry of propaganda. The authentic script records of the 2020 Feb 14th news conference about coping with the novel coronavirus conducted by the State Council. 2020 Feb 14. Available online: http://www.nhc.gov.cn/xcs/fkdt/202002/5329d7ab7af24690a1d5b66982333af3.shtml
- Medical Administration Bureau. The National Health Committee strongly supports the medical treatment in Hubei Province and the city of Wuhan. 2020 Feb 13. Available online: http://www.nhc.gov.cn/xcs/fkdt/202002/ad3af9295f5c4f11a779c02041a2c932.shtml
- Division for Personnel. The notice of the National Health Committee on the implementation of measures to improve the working conditions of front-line medical personnel and care for the physical and mental health of medical personnel [2020 No.61]. 2020 Feb 15. Available online: http://www.nhc.gov.cn/renshi/s3577/202002/85896fabe90747cba8b79beb4c57f202.shtml
- State Statistical Bureau. The main data bulletin of the sixth nationwide census of Sichuan Province in 2010. 2012 Feb 28. Available online: http://www.stats.gov.cn/tjsj/tjgb/rkpcgb/dfrkpcgb/201202/t20120228_30404.html
- Sichuan Health Committee. The first confirmed infected case of the novel coronavirus founded in Sichuan Province demonstrated by the National Health Committee in January 21st. 2020 Jan 21. Available online: http://wsjkw.sc.gov.cn/scwsjkw/gzbd01/2020/1/21/c5d37b61355348769e41f0e73b112c16.shtml
- Gao Y, Xu M, Yang Y, et al. A study on coping styles and related factors of college students during SARS. Chinese Medical Ethics 2004;17:60-3.
- Zhang J, Fu C, Wang F, et al. Analysis of psychological status and coping style of non-active civilian nurses during influenza A (H1N1) epidemic. Journal of Nursing 2010;17:74-6.
- Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006;166:1092-7. [Crossref] [PubMed]
- Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7). J Affect Disord 2020;265:395-401. [Crossref] [PubMed]
- Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version). Mil Med Res 2020;7:4. [Crossref] [PubMed]
- Sun H, Meng Q, Yang F, et al. The psychological analysis for the. medical staffs suffered with SARS. Chin J Behav Med Sc 2003;12:554-5.
- Zhang W, Gan J, Li X, et al. The investigation of. the psychological health of medical staff in SARS. Practical Journal of Medicine & Pharmacy 2003;12:919-21.
- Su L, Wei B. The psychological response of public and intervention in public health. emergency events. Chin J Behav Med Sci 2005;12:1139-41.
- Wang X, Hua L, Wang J. Analysis on mental health status of 2460 health care workers in Beijing. Chinese Journal of Health Education 2013;29:779-81.
- Tu L, Zhang X, Ren N, et al. Current Situation and Analysis of the Medical Staff’ s. Psychological Health in China. Medicine and Philosophy (Humanistic &Social Medicine Edition) 2009;07:44-6.
- Ji Y, Heng Z, Xiang Z, et al. Study on mental health status and its influencing factors among 551 medical staffs in Qingdao City. Chinese Journal of Health Education 2015;31:577-80.
- Li P, Xu Y, Li L, et al. Research on mental health status and. management measures of medical staff in Hainan province. Modern Preventive Medicine 2019;46:3764-7.
- Hu J. The study about medical personnel’ psychological status and related factors in. ‘influenza H1N1 flu’ outbreak. Central South University, 2010.
- Ouyang N. A study on the mental health status of 17170 medical staff and its determinate. factors. Central South University, 2012.
- Song G, Ying C, Liu B, et al. Investigation on psychology state of 180 medical. college students in emergent events of public health. Chin J School Doctor 2012;10:730-1.
- Bangasser DA, Eck SR, Sanchez EO. Sex differences in stress reactivity in arousal and attention systems. Neuropsychopharmacology 2019;44:129-39. [Crossref] [PubMed]
- Ding L, Hu D. Survey of the health status and its influencing factors among the medical staff of a top three hospital. Medical Education Management 2017;3:77-82.
(English Language Editor: C. Betlazar-Maseh)


