
The upper eyelid levator weakening procedure for the correction of severe cicatricial entropion caused by trachoma
Introduction
Upper eyelid cicatricial entropion (UCE) is a common and challenging eyelid disease. In Western countries, UCE is usually caused by chronic blepharitis, previous surgery, trauma, chemical injuries, or Stevens-Johnson syndrome (1). In China, the leading cause of UCE in elderly patients is still trachoma (2-4).
Trachoma-induced UCE often shows conjunctival and tarsal scarring, which leads to contracture and shortening of the upper eyelid posterior lamella. Persistent entropion might lead to keratitis, corneal ulcers, severe corneal scarring, and even blindness (5).
The definitive treatment for trachoma-induced UCE is surgery. Surgeons have developed various surgical techniques to address UCE, including tarsotomy with margin rotation (6), posterior lamella lengthening using grafts (7), eyelash resection (8), and anterior lamella recession (9). But due to the special anatomical characteristics, the single surgery isn’t suitable for Chinese patients, and some other surgeries like using grafts increase the risks of infection and rejection. So far, there are few reports about surgery for Chinese trachomatous UCE patients. In this study, we described and assessed the results of our surgical technique for trachoma-induced UCE: upper eyelid levator weakening combined with tarsotomy and an anterior lamella recession procedure.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-2067).
Methods
Our study was retrospective and non-comparative. Fifty-six eyes from 36 patients suffering from severe trachomatous UCE with short tarsi (width <9 mm) and conjunctiva scarring were retrieved from the Ophthalmology Department of Second Affiliated Hospital of Guangzhou University of Chinese Medicine between January 2017 and December 2019. Patients with thick and long tarsi, and patients who had a history of surgery for UCE were excluded.
All patients were asked to stop systemic anticoagulants before surgery (for at least 1 week). We performed full preoperative ophthalmological examinations before surgery. Eyelid and tarsal conditions, corneal and conjunctival surface disorders, and the shape and position of the eyelashes were analyzed and recorded. All patients signed informed consent forms. A single surgeon performed all procedures. Written consent was retrieved for using clinical photographs and archived in the patient records. This study was adhered to the principles of the Declaration of Helsinki (as revised in 2013).
Surgical technique
Preoperative skin marking
The position of the trichiasis, the patient’s natural eyelid crease or the planned new crease, typically 5–6 mm superior to the upper eyelid margin, was marked first. Then, the patient was asked repeatedly to open and close her or his eyes when she or he sat, and the redundant tissue that was to be excised was marked.
Operative procedure
The procedures were performed under local anesthesia (2.5 mL, 2% lidocaine mixed with 2.5 mL, 0.75% ropivacaine with 1:100,000 epinephrine). We made an eyelid crease incision along the preoperatively marked line. Part of the orbicularis was removed. The orbital septum was opened, the levator aponeurosis was exposed, and the fat pad was judiciously excised. Then, depending on the position of the upper eyelid, 2–4 vertical incisions were made on both sides of the levator aponeurosis to achieve the optimal eyelid height (Figure 1A). Subsequently, a standard gray line incision was made 2 mm beyond the extent of the entropion with a No. 11 scalpel blade, and a pretarsal skin-muscle flap was created. Then, the horizontal line was marked on the tarsus 3–4 mm superior to the lid margin, and a full-thickness tarsal plate incision was made, forming a tarsal flap (Figure 1B). At this stage, if there were some inverted lashes left in the tarsus margin, a standard tarsus wedge resection was performed (Figure 1C). Three sets of sutures were created through the cutting edge of the tarsus to rotate the plate outward 45° with 6-0 vicryl sutures. Then, the skin-muscle flap was repositioned superiorly to leave 2 mm of bare tarsus at the lid margin and sutured to the partial tarsus with 3 to 4 interrupted horizontal mattress sutures (Figure 1D). Finally, the patient opened the eyes, and when the upper eyelid position was satisfactory, and the entropine was corrected, the eyelid skin was closed with 6-0 prolene interrupted sutures. Approximately five stitches were passed through the anterior tarsal surface. All patients wore a patch with antibiotic ointment for 24 hours.

Complete success was defined as no rubbing lashes being detected and no associated eyelid complications during the follow-up period. Failure was when the number of recurrent lashes was over six and required another surgical intervention.
Statistical analysis
Data were collected and analyzed. Descriptive statistics were calculated, and the numerical data were summarized as the mean and standard deviation (± SD). Categorical data were summarized as percentages (%).
Results
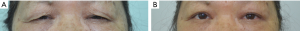
Fifty-six eyelids from 36 patients underwent upper eyelid levator weakening combined with tarsotomy and an anterior lamella recession procedure. The patients’ ages ranged from 64 to 87 years (mean 77.90±10.01 years). Nighteen (52.7%) patients were female, and seventeen (47.2%) patients were male. Bilateral surgery was performed in 20 (55.6%) patients (Figures 2,3). Eight patients (12 eyelids) diagnosed cicatricial trachomatous entropion with keratopathy, and three patients had corneal ulcers (Figure 2A,B). The tarsus width of patients ranged from 7.5 to 8.5 mm (mean 7.93±0.42 mm) by our measure. All patients were followed for 6 to 24 months after surgery (mean 11.61±2.71 months).

Forty-eight eyelids (85.7%) achieved complete success after surgery. A significant improvement in clinical symptoms, including irritation, watering, light sensitivity, and foreign body sensation, was observed in 51 eyes (91.1%). Four eyelids (7.1%) had a ≤5 recurrence of trichiasis, but the severity was milder than before. Among them, three eyelids were treated with electrolysis. One patient refused further treatment, so his eyelashes were pulled out regularly. Four eyelids (7.1%) had an over six recurrent lashes, which needed another surgery. All patients have postoperative eyelid ecchymosis and edema but complete lid closure. All patients also showed marginal thickening in the early stages after surgery, which disappeared by the 2nd month. All patients experienced early-stage ectropion, but it vanished by 2–3 months. Nine (16.1%) eyelids developed mild ptosis postoperatively, which recovered within 1–2 months. None of the patients experienced eyelid contour disorders or other severe complications.
Discussion
Trachoma is chronic infectious keratoconjunctivitis caused by Chlamydia trachomatis (2). Trachoma-induced UCE is the late stage of trachoma and is characterized by progressive conjunctival and tarsal scarring with misdirected lashes rubbing against the cornea (5). Although trachoma has almost disappeared in China, there are still many aged patients suffering from trachoma-induced UCE, and if not treated in time, it can lead to corneal ulcers and even vision loss (3,4). The World Health Organization (WHO) proposed the SAFE strategy to eliminate trachomatous blindness, and surgical treatment is a critical component of the SAFE strategy for managing trachoma-induced UCE (2,5).
In trachoma-induced UCE, the eyelid undergoes a complex anatomic and dynamic change. The scarring of the conjunctiva and tarsal plate leads to contracture and shortening of the posterior lamella, which produces a direct pull on the lid margin and results in an inward rotation of the margin. The anterior lamella and the lashes are turned toward the eyeball (9,10). Through the complex mechanism, the surgeon should balance the physiologic and anatomic damage to the anterior and posterior lamella, which presents a challenge to the surgeon.
The WHO recommends the bilamellar tarsal rotation (BLTR) procedure for treating trachoma-induced UCE (4). However, there are several surgical procedures available for correcting trachoma-induced UCE, depending on the experience of the surgeon and the severity of entropion. Aghai et al. performed an anterior lamella recession for the management of trachoma-induced UCE (9). Cruz et al. described a surgical technique involving a lid crease approach with internal absorbable sutures for upper lid margin rotation (10). Sadiq et al. reported bilamellar tarsal margin rotation with blepharoplasty to address the UCE (11). Osaki et al. combined labial mucous membrane grafts to lengthen the posterior lamella to treat severe UCE (7). Besides all of the above, there are some other new surgical method for Caucasian trachomatous UCE, such as anterior lamellar reposition and tarsal margin rotation with posterior lamella superadvancement (6,12).
The tarsotomy procedure is a conventional and classic surgery to treat trachoma-induced UCE in Asian countries (13-15). In that surgery, a horizontal tarsotomy is formed across the entire tarsus, and then the anterior lamella and lid margin is rotated with external sutures. However, there are some limitations to this surgery. First, it produces a new horizontal scar in the tarsal plate and conjunctiva, which will cause the posterior lamella shorter after surgery. Second, after removing the stitches, the traction of the tarsus is relieved, and lid rotation becomes downward because of gravity. Therefore, we found a high rate of entropion recurrence in our clinic.
The Asian eyelid has distinctive anatomical properties, including single eyelids, short tarsal plates, thick skin, weak levator function, and more fatty pads in the upper eyelid. Therefore, different and innovative surgical techniques are needed for Asian patients (16,17); however, few reports about the surgical methods are available for severe trachoma-induced UCE in Chinese patients.
We used upper eyelid levator weakening combined with tarsotomy and an anterior lamella recession procedure, i.e., a combination of several well-known techniques, to treat severe trachoma-induced UCE in Chinese patients. In this surgery, we performed the upper eyelid levator weakening procedure to lengthen the posterior lamella, which advanced the lamella inferiorly. We also performed a modified partial tarsotomy procedure to achieve lid rotation and gray line splitting with anterior lamella repositioning to prevent downward migration of the anterior lamella. Elderly patients often have other eyelid abnormalities, including dermatochalasis and brow ptosis. The redundancy of the upper eyelid skin, orbicularis oculi muscle, and fatty pads may mechanically slide toward the lid margin and result in the recurrence of the entropion (18,19), so we usually combine blepharoplasty or additional surgical techniques to remove the excess skin, muscle, and fat.
As we know, there are various techniques for lengthening the posterior lamella (20-23), but the upper eyelid levator weakening procedure that we have described was more straightforward to perform and associated with less morbidity than posterior lamella grafts, which require a donor site and have the risk of graft failure. Some authors have advised the levator recession to compensate for the degree of posterior lamella retraction (22,23). However, because Asians have weak levator function, we hypothesize the levator weakening procedure was better than the levator recession. The outcome of our technique was satisfactory. There were no severe complications, and all the patients were satisfied with their postoperative eyelid contour. During the follow-up period, the recurrence rate was low (7.1%), and the recurrence of trichiasis could be resolved by electrolysis, an economical and straightforward method. The results showed that our technique was effective in treating severe trachoma-induced UCE in Chinese patients.
Also, we have some other personal experience with this surgery. First, the height of the new eyelid crease should not be too high. Because the function of the levator was weakened and the gray line split was done, the postoperative eyelid crease could become wider, and the lid margin could become thicker than before, which would produce a poor cosmetic contour. Second, for Asian patients, the orbicularis and fat pad should be judiciously removed. If too much tissue is left, it increases the risk of recurrence. Third, upper eyelid retraction should not be overcorrected. Fourth, the patients could have mild or moderate ectropion in the early postoperative stage, but it was better by 1–3 months after surgery.
In conclusion, upper eyelid levator weakening combined with tarsotomy and an anterior lamella recession procedure effectively treated severe trachoma-induced UCE in Chinese patients with good functional results, relatively low recurrence rates, and satisfactory cosmetic results. However, the limitations of this study are the small sample size and the lack of a comparison group. However, our surgical method may give other surgeons new ideas for treating severe trachoma-induced UCE in Chinese patients.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-2067
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-2067
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-2067). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All patients signed informed consent forms. Written consent was retrieved for using clinical photographs and archived in the patient records. This study was adhered to the principles of the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Millman AL, Katzen LB, Putterman AM. Cicatricial entropion: An analysis of its treatment with transverse blepharotomy and marginal rotation. Ophthalmic Surg 1989;20:575-9. [PubMed]
- Flueckiger RM, Courtright P, Abdala M, et al. The global burden of trichiasis in 2016. PLoS Negl Trop Dis 2019;13:e0007835. [Crossref] [PubMed]
- Jie Y, Xu L, Ma K. Prevalence of trachoma in the adult Chinese population. The Beijing Eye Study. Eye 2008;22:790. [Crossref] [PubMed]
- El Toukhy E, Lewallen S, Courtright P. Routine bilamellar tarsal rotation surgery for trachomatous trichiasis: Short-term outcome and factors associated with surgical failure. Ophthal Plast Reconstr Surg 2006;22:109-12. [Crossref] [PubMed]
- Lavett DK, Lansingh VC, Carter MJ, et al. Will the SAFE strategy be sufficient to eliminate trachoma by 2020? Puzzlements and possible solutions. ScientificWorldJournal 2013;2013:648106. [Crossref] [PubMed]
- Russell DJ, Seiff SR. Long-term results for entropion repair by tarsal margin rotation with posterior lamella superadvancement. Ophthal Plast Reconstr Surg 2017;33:434-9. [Crossref] [PubMed]
- Osaki TH, Sant’Anna AE, Osaki MH, et al. Management of severe cicatricial entropion with labial mucous membrane graft in cicatricial ocular surface disorders. J Craniofac Surg 2018;29:1531-4. [Crossref] [PubMed]
- Wu AY, Thakker MM, Wladis EJ, et al. Eyelash resection procedure for severe, recurrent, or segmental cicatricial entropion. Ophthal Plast Reconstr Surg 2010;26:112-6. [Crossref] [PubMed]
- Aghai GH, Gordiz A, Falavarjani KG, et al. Anterior lamellar recession, blepharoplasty, and supratarsal fixation for cicatricial upper eyelid entropion without lagophthalmos. Eye 2016;30:627-31. [Crossref] [PubMed]
- Cruz AAV, Akaishi PMS, Al-Dufaileej M, et al. Upper lid crease approach for margin rotation in trachomatous cicatricial entropion without external sutures. Arq Bras Oftalmol 2015;78:367-70. [Crossref] [PubMed]
- Sadiq MN, Pai A. Management of trachomatous cicatricial entropion of the upper eye lid: our modified technique. J Ayub Med Coll Abbottabad 2005;17:1-4. [PubMed]
- Ahmed RA, Abdelbaky SH. Short term outcome of anterior lamellar reposition in treating trachomatous trichiasis. J Ophthalmol 2015;2015:568363. [Crossref] [PubMed]
- Chi M, Kim HJ, Vagefi R, et al. Modified tarsotomy for the treatment of severe cicatricial entropion. Eye 2016;30:992-7. [Crossref] [PubMed]
- Cornand G, Doury JC. Trachomatous tarsitis: its consequences and their surgical treatment (author’s transl). Med Trop (Mars) 1981;41:157-71. [PubMed]
- Thanh TTK, Khandekar R, Luang VQ, et al. One year recurrence of trachomatous trichiasis in routinely operated Cuenod Nataf procedures cases in Vietnam. Br J Ophthalmol 2004;88:1114-8. [Crossref] [PubMed]
- Bi YL, Zhou Q, Xu W, et al. Anterior lamellar repositioning with complete lid split: a modified method for treating upper eyelids trichiasis in Asian patients. J Plast Reconstr Aesthet Surg 2009;62:1395-402. [Crossref] [PubMed]
- Sun L, Chen X, Liu G, et al. Subcutaneous Fat in the Upper Eyelids of Asians: Application to Blepharoplasty. Clin Anat 2020;33:338-42. [Crossref] [PubMed]
- Kemp EG, Collin JR. Surgical management of upper lid entropion. Br J Ophthalmol 1986;70:575-9. [Crossref] [PubMed]
- Sodhi PK, Yadava U, Pandey RM, et al. Modified grey line split with anterior lamellar repositioning for treatment of cicatricial lid entropion. Ophthalmic Surg Lasers 2002;33:169-74. [PubMed]
- Fin A, De Biasio F, Lanzetta P, et al. Posterior lamellar reconstruction: a comprehensive review of the literature. Orbit 2019;38:51-66. [Crossref] [PubMed]
- Swamy BN, Benger R, Taylor S. Cicatricial entropion repair with hard palate mucous membrane graft: Surgical technique and outcomes. Clin Exp Ophthalmol 2008;36:348-52. [Crossref] [PubMed]
- Pandey N, Jayaprakasam A, Feldman I, et al. Upper eyelid levator-recession and anterior lamella repositioning through the grey-line: Avoiding a skin-crease incision. Indian J Ophthalmol 2018;66:273-7. [Crossref] [PubMed]
- Ross AH, Cannon PS, Selva D, et al. Management of upper eyelid cicatricial entropion. Clin Experiment Ophthalmol 2011;39:526-36. [Crossref] [PubMed]
(English Language Editor: J. Chapnick)


