Surgery, palliative care, and the American College of Surgeons
Since the late 1990s, the American College of Surgeons (ACS) has increasingly recognized and advocated palliative care for patients and their families with serious, critical, and terminal illness under surgical care. The college has been the primary catalyst for the recognition of palliative care in the field of surgery in the U.S. and abroad, primarily through educational efforts directed at practicing surgeons and surgeons in training. Roughly 15 years ago a group of surgeons of different specialties from the fellowship of the college coalesced and then spearheaded these initiatives with invaluable support and advice from leading non-surgeon pioneers of palliative care. The subsequent growth and evolution of this group reflected the same pattern observable in the non-surgical medical specialties: it commenced its activities as a “grass roots” movement representing a wide spectrum of specialties with an even wider spectrum of abilities and experience and evolved into a sophisticated and experienced core of board-certified specialists in Hospice and Palliative Medicine in addition to a primary surgical specialty.
The ACS was uniquely advantaged in becoming an effective advocate for palliative care education for its membership because of its historic significance, scientific and educational reputation, and ethical credibility. Before palliative care was widely known and available and few surgeons had had direct experience with hospice in the late 1990s, the college had begun to wrestle with end of life issues but only through the narrow lens of ethical debates about the limits of individual autonomy and paternalism best exemplified by a major symposium on physician assisted suicide held in 1997. Regardless of the position taken about the legitimacy of physician assisted suicide, it was evident to most surgeons at that time that surgeons were ill equipped to address the most elementary problems encountered in end-of-life care such as communication, pain control, and the scope of appropriate medical interventions. Despite a rich history of contributions that would ultimately prove invaluable in the conduct of palliative care, including several striking examples of individual accomplishment in hospice care, surgery appeared to be absent from the table in the early days of specialty practice of hospice and palliative care. That status quo was capsulized in an article published in the Bulletin of the American College of Surgeons in April 1997 (1).
Another promising note during this era was the college’s release of its “Statement of Principles Guiding Care at the End of Life” (2) a few months after its symposium on physician-assisted suicide. This document, however, was written by the college’s committee on ethics that had neither members nor input from individuals with formal hospice or palliative care training or practice experience. The 1998 “Statement” was superseded in 2005 when the college issued its “Statement on Principles of Palliative Care” (3) (Table 1), which was jointly written by the Committee on Ethics and the Surgical Palliative Care Task Force that included surgeons certified in Hospice and Palliative Medicine.
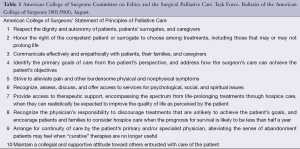
Full table
By the time of the Annual Clinical Congress held in 2000, there was enough interest in palliative care among the college leadership to present a symposium titled, “Palliative Care by the Surgeon: Patient Selection and Management” (4). This symposium’s significance was the public discourse of two highly esteemed surgeons with reputations for ethical probity, the late C. James Carrico and Thomas J. Krizek, and one of the most recognizable names in palliative medicine at that time, Kathleen Foley. The success of this symposium provided the needed momentum for the continued attention of the college’s leadership. Much credit is due to the late Olga Jonasson, then Director of the Division of Education, for her personal interest in raising the visibility of palliative care within the educational activities of the college. Her intellectual and personal stature as a surgeon and scientist was enough to brush off any serious challenges to the legitimacy of the concept. Several years later [2006], she would strongly support the American Board of Surgery’s joining other specialty boards in their sponsorship of certification in hospice and palliative medicine through the American Board of Medical Specialties (ABMS).
During this formative period of the creation of a comprehensive framework of surgical palliative care, critical guidance and mentoring was freely and graciously given by a triumvirate of individuals, David Weissman, Ira Byock, and Charles Von Gunten, all of whom possessed qualities welcomed by surgeons—dry humor, rigorous intellect, and effectiveness in their undertakings. All of them were well known palliative care clinicians, researchers, and educators who had demonstrated an interest in surgery and surgeons. Through their network of connections surgeons found a seat at the table with the non-surgical disciplines in the final years of the Robert Wood Johnson Foundation’s (RWJF’s) funding for end-of-life care initiatives.
In 2001, the RWJF funded a Surgeons Workgroup to survey the state of end-of-life care in the field of surgery with the expectation of issuing a report as the end product. The grant was administered through the Division of Education of the ACS. Because of the assets and interest of the college, however, far more was accomplished with the impetus and prestige of the RWJF grant. A Surgeons Palliative Care Workgroup was organized and met for the first time, auspiciously, on September 10, 2001. By this time several symposia had been planned for future Annual Clinical Congresses and the Workgroup had sponsored a series of monthly articles that were to appear in the Journal of the American College of Surgeons (JACS) over the next 3 years. The JACS series was approved by Seymour Schwartz, the Editor in Chief of JACS, and passionately supported and skillfully edited by its Executive Editor, Wendy Husser. In addition to her contributions to the JACS palliative care series, she navigated surgeons belonging to the Workgroup through the structure of the college’s committees and social network that afforded opportunities later for the Workgroup’s transition from a temporary, externally grant-funded entity to a permanent part of the college structure. This transition occurred the same year [2003] as the Workgroup’s publication of its “Report from the Field”. The new college supported entity was named the ACS Palliative Care Task Force. The Task Force became part of the Division of Education, which at that point and now is under the consistently supportive leadership of surgical educator, Ajit Sachdeva. In 2013, the Task Force assumed its current designation, the Committee on Surgical Palliative Care (CSPC).
Over the past decade (refer to Table 2 for chronology), the CSPC has sponsored symposia at every Annual Clinical Congress of the ACS, has participated in proceedings of other college sponsored programs and committees including the Commission on Cancer, the Committee on Trauma, and the widely used self-education program, Surgical Education and Self-Assessment Program (SESAP®). In 2009, the CSPC contributed to the publication of “Surgical Palliative Care: A Resident’s Guide” (5). This project was administered by the ACS and funded by the Cunniff-Dixon Foundation, a philanthropic organization whose original mission was to enrich the physician-patient relationship near the end of life by the education and inspiration of individual physicians to inspire them to provide the kind of care near the end of life wished by all. The work of the CSPC and its preceding groups has enjoyed the enthusiastic support of the late Thomas R. Russell, formerly Executive Director of the college, and his successor, David B. Hoyt. Linn Meyer, formerly Director of Member Services for the college, should be recognized for securing frequent opportunities for the Task Force to publish its work and experience in the college’s bulletin in addition to serving as the coordinator for the Resident’s Guide project. It is noteworthy that much of the work of the CSPC would have not been accomplished without the passionate interest of the college staff most of whom were not physicians. However, at the highest level of surgical leadership, the College’s Board of Regents, support for developing the concept of palliative care by surgeons was evident even before the Task Force was organized. One of its members, John L. Cameron, is editor of the first widely read surgical textbook to recognize surgical palliative care as a distinct entity. In it surgical palliative care is defined: “…the treatment of suffering and the promotion of quality of life for seriously or terminally ill patients under surgical care.” (6). Another member of the board of regents, Mary H. McGrath, oversaw the release of the college’s “Statement of Principles of Palliative Care” in her capacity as Chair of the College’s Committee on Ethics, edited a text book on ethics for surgeons (7) in addition to frequently moderating well attended symposia and debates addressing palliative care ethical and practice issues.
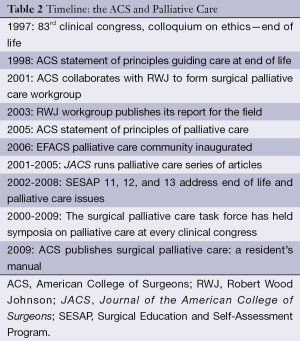
Full table
In 2012, the Commission on Cancer, an ACS sponsored program, first required in its Cancer Program Standards (8) that palliative care services be available to patients either on site or by referral. This requirement was a significant contribution from a surgical organization to the conduct of palliative care for cancer patients under the care of all medical specialists. It would have been far less likely to occur without the personal interest and leadership of surgeons, Stephen B. Edge, Frederick L. Greene, and Philip Y. Roland.
The ACS CSPC (Table 3) accepts members from the Fellowship of the ACS, which represents all specialties of surgery. A formal meeting of the core committee occurs annually at the ACS headquarters in Chicago. The CSPC’s mission is to incorporate the precepts and techniques of palliative care into surgical clinical practice, education, research, and advocacy. The current committee structure now includes an executive committee and sub-committees on education, research, patient quality outcomes, and advocacy. The current membership includes surgeons specializing in trauma and critical care, general surgery, oncologic surgery, and gynecologic oncology. Almost all members are now ABMS certified in Hospice and Palliative Medicine in addition to their primary surgical certification. Several are triple-boarded.
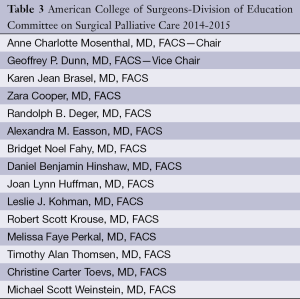
Full table
Some of the current initiatives by the CSPC include preparing a more readily available pathway for surgeons to pursue fellowship training in hospice and palliative medicine, identification of quality indicators of surgical palliative care, and revision of the current 30-day mortality and morbidity surgical outcome measure to better accommodate palliative surgical interventions.
The CSPC contributes regularly to the palliative care series published in the ACS’ Surgery News. Several of these articles (9,10) have provided opportunities for recently trained surgeons and surgeons-in-training to address some of the salient themes of surgical palliative care, auguring well for the future of this concept.
To summarize the ACS’ contribution to the evolution of surgical palliative care, it started the search for an effective strategy for the care of surgical patients at the very end of life following the recently established ethical and legal pathway to freedom from futile or undesired treatments as laid out in the landmark cases of Quinlan (11) (ruling allowed withdrawal of ventilator support from patient in permanent vegetative state), Cruzan (12) (ruling affirmed that patients who could not make decisions still retained a right to refuse medical treatment) and its acknowledgement of end-of-life issues within the limited scope of the physician assisted suicide debate. This commenced with highly intellectualized discourse by ethicists that left surgeons with the practical challenges about how surgeons should communicate with seriously ill patients, how they should manage their most troubling symptoms, and how they should contribute to the restoration of hope using their own and their patients’ personal, socioeconomic, and spiritual assets. Since the late 1990s much evidence based information about daily palliative care practice has accumulated of which surgeons and surgical organizations are now prepared to assimilate much in part because of the endorsement and ground work laid by the ACS.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Milch RA, Dunn GP. The surgeon and palliative care. Bull Am Coll Surg 1997;82:15-18.
- Statement on principles guiding care at the end of life. American College of Surgeons' Committee on Ethics. Bull Am Coll Surg 1998;83:46. [PubMed]
- Task Force on Surgical Palliative care; Committee on Ethics. Statement of principles of palliative care. Bull Am Coll Surg 2005;90:34-5.
- The American College of Surgeons 86th Annual Clinical Congress. Chicago, Illinois, USA, 2000.
- Dunn GP, Martensen R, Weissman D. eds. Surgical Palliative Care: A Resident’s Guide. Chicago: American College of Surgeons, Cunniff-Dixon Foundation, 2009.
- Cameron JL, Cameron AM. eds. Current Surgical Therapy 9th edition. Philadelphia: Mosby Inc., 2007.
- McGrath MH, Risucci DA, Schwab AP. eds. Ethical issues in clinical surgery. Chicago: American College of Surgeons, 2007.
- Commission on Cancer. eds. Cancer Program Standards 2012: Ensuring Patient-Centered Care v1.0. Chicago: American College of Surgeons, 2011.
- Johnston FM. Commentary: Preemptive planning is key to palliative care. Available online: http://www.acssurgerynews.com/opinions/palliative-care/blog/commentary-preemptive-planning-is-key-to-palliative-care/afb635e9df0ba6df5864ba8155432cfa.html?tx_ttnews[sViewPointer]=2
- Kayssi A, Easson AM. No heroic measures. Available online: http://www.acssurgerynews.com/index.php?id=14883&cHash=071010&tx_ttnews[tt_news]=139969
- In re Quinlan, 70 N.J. 10 (1976), 355 A.2d 647. In the matter of Karen Quinlan, an alleged incompetent. Available online: https://www.uta.edu/philosophy/faculty/burgess-jackson/In%20re%20Quinlan,%2070%20N.J.%2010,%20355%20A.2d%20647%20%281976%29.pdf
- Cruzan V. Director, Missouri Department of Health, (88-1503), 497 U.S. 261 (1990). Available online: http://www.law.cornell.edu/supct/html/88-1503.ZS.html


