
Morphological changes of lymphocytes in peripheral blood smears of patients with COVID-19
Clinical laboratory has played an important role in the diagnosis, treatment and prognosis of coronavirus disease 2019 (COVID-19) patients. A notable laboratory finding was that the absolute value of lymphocyte in most confirmed cases was reduced, which suggests that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) might mainly act on lymphocytes (1). Previous published studies mainly focused on epidemiological, radiological, and clinical characteristics of COVID-19 patients. Little attention has been paid to the morphological changes of peripheral white blood cell. Hence, this pilot study was to investigate whether SARS-CoV-2 infection causes morphological changes in peripheral lymphocytes.
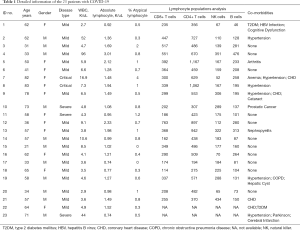
A total of 23 most recently hospitalized patients from 25 February to 01 March, including 12 females, were enrolled in this study, with age ranging from 31 to 83 years old. All of the 23 inpatients denied histories of leukemia (Table 1). According to Novel Coronavirus Pneumonia Prevention and Control Program (5th edition) published by the National Health Commission of China, COVID-19 patients were categorized into four types: mild type, moderate type, severe type and critical type (2). The disease categories were as follows: 18 mild cases, 3 severe case and 2 critical case. All the blood samples were obtained on the admission day of each patient. Morphological changes, compared with normal lymphocyte, in peripheral lymphocytes were defined as atypical lymphocyte. Blood five differential counts were determined by Mindray automated hematology analyzer. Lymphocyte population analysis was performed via flow cytometry. Peripheral blood smears, obtained by use of the wedge-pull smear technique and stained by means of Wright-Giemsa method, were visually examined by two independent experienced clinical technicians by use of light microscopy. In order to calculate the atypical lymphocytes ratios, 200 white blood cells were counted.
Full table
Our results showed that the highest percentage of atypical lymphocytes was just 4%, while the second highest in our cohort was 2%. The rest were all around 1% (Table 1). This was much lower than that of another similar study, whose results demonstrated that highest percentage of atypical lymphocytes was up to 13.5% (6.90%±4.30%) (3). Most of the atypical lymphocytes observed in our cohort was just irregular shaped lymphocytes with excessive cytoplasm but normal nucleus (Figure S1). Plasmacytoid lymphocytes were also observed but with a low percentage, which was in agreement with other studies (4,5).
The atypical lymphocyte can be found in small numbers in normal human blood (6) and in increased numbers in a variety of clinical settings, especially infectious mononucleosis and many viral as well as non-viral illnesses, because atypical lymphocytes are generally lymphocytes that have been activated to respond to a viral infection or sometimes a bacterial or parasitic infection. From the results of some sporadic researches with very limited number of enrolled participants, it can be concluded that SARS-CoV-2 infection is a new aetiology for atypical lymphocytes, however, is the presence of atypical lymphocytes, especially plasmacytoid lymphocytes, a laboratory feature of SARS-CoV-2 infection still needs to be validated by future studies with larger populations.
Acknowledgments
We thanked Professor Li Ming from 991st Hospital of Joint Logistic Support Troop for his professional help during our revision.
Funding: None.
Footnote
Provenance and Peer Review: This article was a free submission to the journal. The article has undergone external peer review.
Peer Review File: Available at
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See:
References
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- Liu YP, Li GM, He J, et al. Combined use of the neutrophil-to-lymphocyte ratio and CRP to predict 7-day disease severity in 84 hospitalized patients with COVID-19 pneumonia: a retrospective cohort study. Ann Transl Med 2020;8:635. [Crossref] [PubMed]
- Weinberg SE, Behdad A, Ji P. Atypical lymphocytes in peripheral blood of patients with COVID-19. Br J Haematol 2020;190:36-9. [Crossref] [PubMed]
- Foldes D, Hinton R, Arami S, et al. Plasmacytoid lymphocytes in SARS-CoV-2 infection (Covid-19). Am J Hematol 2020;95:861-2. [Crossref] [PubMed]
- Gérard D, Henry S, Thomas B. SARS-CoV-2: a new aetiology for atypical lymphocytes. Br J Haematol 2020;189:845. [Crossref] [PubMed]
- Wood TA, Frenkel EP. The atypical lymphocyte. Am J Med 1967;42:923-36. [Crossref] [PubMed]


