3D printing technology applied to orthosis manufacturing: narrative review
Introduction
An orthosis is a device used to assist the functions of the human body. They usually have the following purposes: body protection, restricting motion, weight-bearing assistance, movement assistance, and deformity prevention or correction. Thus, orthoses are widely applied to patients with physical dysfunction and disability due to muscular dysfunctions, such as fractures, sprains, arthropathy and tendinopathy, and neurological disorders in the brain, spinal cord, and peripheral nerves (1,2).
The conventional method for manufacturing orthoses is relatively time-consuming. Further, it is necessary to manually correct the shape and dimensions of the orthosis according to the patient’s body. In addition, it is challenging to produce multiple customized orthoses with the same quality, and complex designs sometimes can be implemented. However, using recently developed three-dimensional (3D) printing technology, orthoses can be designed with exact dimensions through a computer graphic program, and the aforementioned disadvantages of the conventional method can be sufficiently addressed because 3D printers are highly accurate. Thus, using 3D printing technology, it is possible to design an orthosis with accurate numerical values of the dimensions through a design program and create structures that are difficult to implement manually (3-5). Additionally, while a manually produced orthosis requires approximately 1 week to produce, a 3D printer can perform this task in a day (6,7). Therefore, in the field of orthoses, significant attention is being paid to orthoses manufactured with 3D printing technologies.
In this study, we investigate the recent advancements in 3D printed orthoses by reviewing prior studies. We present this article in accordance with the narrative review reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1185).
Methods
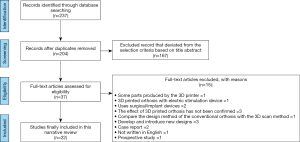
We set “3D printed orthosis”, “3D printed orthoses”, “3D printed braces”, “3D printed splints”, “3D printing orthosis”, “3D printed orthoses”, “3D printing braces” and “3D printing splints” as keywords in PubMed, CINAHL Complete & MEDLINE Complete, Cochrane, Embase, and Scopus to search for articles published up to July 27, 2020. The criteria for article inclusion are as follows: (I) 3D printed orthosis applied to a patient or a healthy subject, (II) area of application should be an upper limb, lower limb, or spine, (III) prospective study, and (IV) the availability of a full-text. The criteria for article exclusion are as follows: (I) object of comparison is a surgical treatment, or a conservative treatment other than orthosis, (II) orthosis manufactured by adding electrical stimulation device or robotic device, (III) replacement product for human body structure made for surgery or implant, (IV) some parts produced by a 3D printer, and (V) case reports, conference abstracts or presentations, review articles, and non-English publications.
The level of evidence was defined using the Research Pyramid model. The evaluation criteria are as follows: (I) level 1: systematic reviews and meta-analysis of randomized controlled trials (RCTs), (II) level 2: one or more RCTs, (III) level 3: controlled trials without randomization (at least two groups), (IV) level 4: case-control or cohort study, (V) level 5: systematic review of descriptive and qualitative study, (VI) level 6: single descriptive or qualitative study, and (VII) level 7: expert opinion. The results of the level of evidence evaluation of the papers included in this review were level 2 in six papers (6-11), level 3 in six papers (4,5,12-15), and level 4 in ten papers (3,16-24).
Results
We identified 237 relevant articles. Among them, a total of 22 were selected (3-24), excluding articles that did not match the inclusion criteria (Figure 1). Of the 22 studies, there were 8 studies related to the upper limbs (6,11,16-19,21,24), 13 related to the lower limbs (3-5,7-10,12,14,15,20,22,23), and 1 related to the spine (13). The characteristics of each study are summarized in Table 1. The following subsection explains how orthoses are made for each study.

Full table
Upper limb orthosis
Of the eight articles, two were randomized trials (6,11), and six were prospective observational studies (16-19,21,24).
In 2018, Kim et al. (6) manufactured a 3D printed orthosis in which the wrist joint was slightly dorsiflexed and free finger movements were possible, and the length was to the center of the forearm. The control group used ready-made cock-up splint. In 2020, Zheng et al. (11) manufactured the 3D printed orthosis in shape of a functional hand position (10°–15° extension of the wrist, 40°–45° flexion of the metacarpophalangeal (MP) and proximal interphalangeal, and thumb abduction). The control group used a low-temperature thermoplastic plate orthosis. In 2017, Chen et al. (16) 3D printed an orthosis designed to wrap around from the center of mid-forearm to the MP except for the thumb. In addition, the forearm part had several small holes for ventilation and wearer-friendliness, and the shells surrounding the upper and lower parts of the forearm-wrist-hand were sectioned and could be fixed using a Velcro strap. The 3D printed orthosis used by Portnova et al. (21) in 2018 was a wrist-driven orthosis, and each component of the orthosis was manufactured in various sizes to suit different users. The orthosis was designed with the feedback from three users and six orthotists. In 2018, Wang et al. (24) 3D printed the orthosis in the form of a fingerboard that straightens five fingers and maintains an abduction position. Small holes were drilled into the palmar side to make it breathable and comfortable for the user when wearing the orthosis. Only the base plate was produced using a 3D printer, and a Velcro strap was used for fixing it to the hand and finger. The 3D printed orthosis used by Guida et al. (18) had a design in which the wrists and hands were almost horizontally aligned, and the thumb was fixed at a slight abduction. The length of the body ranged from approximately proximal two-third of the forearm to a little above the MP. The shell was made in a double-shell design, and a hole was created on the entire shell for ventilation and lightness. In 2019, Lee et al. (19) 3D printed an orthosis designed to support from approximately the mid-forearm area to the MP and wrap only the MP area. The back of the hand and forearm were fixed with Velcro straps. As the patient wanted to perform daily life activities such as typing, eating, and writing. The hypothenar eminence area has a connector to fix a typing device or spoon, and a small ring was included between the thumb and index finger of the orthosis such that a pencil could be used. Furthermore, several small holes were made for breathability. In 2020, Chu et al. (17) measured the hands of 120 subjects and created a 3D parametric hand model. When manufacturing the orthosis, an offset of 1–2 mm was applied to the interphalangeal joint of the thumb and MP, and another offset of 2–3 mm was applied between the fifth metacarpal bone and the carpometacarpal joint. Thus, a suitable space was created on the inner surface between the thumb and the orthosis. This orthosis was designed to wrap under the MP, back of the hand, under the interphalangeal of thumb, and palm. There were no holes for ventilation, and because it consisted of one shell, a separate strap was not required.
Lower limb orthosis
Of the 13 related articles, there were four randomized trials (7-10) and 10 prospective observational studies (3-5,12,14,15,20,22,23).
In 2017, Telfer et al. (7) designed a 3D printed insole using foam-box foot impressions that were 3D scanned. The metatarsal area of the insole was layered, and the pressure was distributed when a vertical load was applied. The shape of the insole was similar to that of a ready-made insole. In 2019, Mo et al. (8) produced a 3D printed foot orthosis, with the subtalar joint positioned neutrally. A 3-mm PORON cover was added to the foot orthosis. Two studies were conducted in 2019 by Xu et al. (9,10). One of them was targeted at patients with plantar fasciitis (9). The pressure distribution was eased using lateral wedges in the heel of the insole and metatarsal pad. In a study involving patients with bilateral flat foot (10), a customized 3D printed insole was constructed that firmly supported the medial arch of the foot such that it did not collapse. In this 3D printed insole, the part surrounding the heel was deeper than in ready-made or normally customized insole, which increased the contact area where the foot touches the insole, thereby distributing the pressure. The 3D printed foot orthosis produced in two studies conducted by Telfer et al. in 2013 (22,23) were semi-rigid devices and three-fourth of the total foot length. The 3D printed orthosis used by Dombroski et al. (4) was designed through a 3D scan. Although the shape was not specifically mentioned, it had a feature that resulted in a higher arch height index than the control group. Allan et al. (12) evaluated the effect using eight types of 3D printed insole, including three-fourth of the length or full length with (I) 0° rearfoot, (II) 5° rearfoot, (III) 10° rearfoot and 5° forefoot, and (IV) 10° rearfoot. All individuals’ foot were scanned, and the insoles were made according to the shape of each foot. The orthosis used by Cha et al. (3) was an open type of heel and malleolus. Similar to the conventional orthosis, the front side was open with a shape that wrapped more to the front of the lower limb. The calf shell and plantar foot-plate length were approximately half of the conventional orthosis. In 2019, Jin et al. (5) produced the basic 3D printed insole in the form of a raised heel structure and an arched arch lift. The experimental group was divided into two groups; Group A had modified insoles such that the lateral-longitudinal portion was completely in contact with the bottom. The insoles of Group B were not applied with an arch lift. Liu et al. (20) produced 3D printed ankle-foot orthosis similar to posterior leaf spring orthosis. The ankle trim line passed behind the malleolus, and the foot plate fitted the entire length of the plantar of the foot. The sole and calf shells had several holes for comfort, ease of ventilation, weight reduction, and material cost savings. The 3D printed insole used by Mannisi et al. (14) was produced by adding lateral wedges of 0°, 5°, and 10° to the insoles manufactured by 3D scanning the knees and ankles at a 90°-bend with no load applied. Tarrade et al. (15) scanned each patient’s foot through a 3D footprint scanner and made customized orthoses. Subsequently, neutral insole was attached to the foot orthosis and applied to the subjects. Foot orthoses had an arch shape to support the arch.
Spinal orthosis
One prospective observational study was conducted to evaluate the effectiveness of 3D printed spinal orthosis (13).
The 3D printed orthosis used by Kuo et al. (13) was applied to the cervical vertebrae. Typical cervical orthosis wraps around the entire neck, whereas the 3D printed orthosis used in that study had support only in the front side. There were mandibular and lateral supports that descended to the clavicle at both ends of the mandibular support. In addition, the 3D printed orthosis had venting holes and strap holes on the mandibular support. The user could be fixed using the strap to prevent the orthosis from falling off the body.
Discussion
In the current review, we found that 3D printed orthoses can effectively improve biomechanical and kinematic parameters, and their effectiveness is similar to that of conventional orthoses. Additionally, study participants felt comfortable wearing 3D printed orthoses. Furthermore, in some studies, the effectiveness of 3D printed orthoses and the comfort when wearing them were better than those of conventional orthoses. Of the 22 studies included in our review, 10 of them (3-5,7-11,13,19) compared the effectiveness of 3D printed orthoses with that of conventionally produced orthoses. In all those studies, 3D printed orthoses showed superior or similar results in the evaluation parameters (satisfaction, wrist spasticity, wrist-hand function, gait parameter, arch height index, and plantar foot pressure and joint range of motion (ROM) compared to conventional orthoses, and patient satisfaction with 3D printed orthoses was also comparable with that of conventional orthoses. The reasons why 3D printed orthoses were more satisfactory and some explanations are as follows:
The effects and satisfaction of 3D printed orthosis were also evaluated in studies not mentioned previously (6,12,14-18,20-24). The results of stability, pain, pressure, function of the affected area, and satisfaction were generally excellent (Table 1). In aggregate, the pain was reduced, joint ROM was improved, and satisfaction was high because it was light and comfortable to wear. Given the advantages of 3D printed orthoses, this technology is expected to be used more widely in clinical practice in the near future. However, 3D printed orthosis is not excellent in all aspects. When performing a 3D scan, difficulty may arise owing to the patient being in an incorrect posture or continuously moving. In this case, a posture correction device should be used or an expert should set the optimal posture. There are limitations of the 3D printer as well. It is difficult to manufacture an orthosis with an exceptionally large circumference or height. In addition, although the price range varies, a printer with excellent quality and high production speed is expensive; therefore, it may be difficult to obtain a machine without basic funds. The use of unwarranted, low-cost printer and materials requires caution as it can cause secondary damage to users. In addition, for 3D printing technology to be actively used in the manufacturing of orthoses, we expect that practitioners in related fields, such as clinicians, prosthetists, orthotists, and occupational therapists, will have to acquire CAD utilization skills and increase their understanding of 3D printing technology.
Among the 22 studies included in our review, in 15 of them (3-8,12-15,18-20,22,23), the subjects’ bodies were scanned using a 3D scanner and later a CAD program was used to handle the data and design the orthosis. In five studies (9-11,17,21), a CAD program was directly used to design the orthosis, which was then self-produced. CAD files obtained through a 3D scanner can be modified using a CAD program, which is a design program that is used to create and edit drawings. Because CAD files can be stored for a long time, it is easy to manufacture an orthosis of the same design using a saved file when the orthosis is damaged or lost (3,11). It is also easy to modify it according to the patient’s desired shape (9,19). Open-source design is a free design source. It is free to use and accessible by anyone, and a wider variety of designs can be created in a short period of time based on open-source data (21).
The materials usually used for 3D printed orthoses include PLA, ABS, and TPU. PLA is an environmentally friendly material that has no environmental hormones or heavy metals. Additionally, PLA is a material with excellent renewability and biocompatibility (25). ABS is a type of styrene resin composed of three components (acrylonitrile, butadiene, and styrene). ABS has high impact resistance and ease of processability (26). TPU has mechanical properties, such as the highest tensile strength, tearing strength, and abrasion resistance among thermoplastic elastomers (26). Therefore, these materials are being widely used when manufacturing objects with high durability.
In this review, we investigated the effects of 3D printed orthoses. In all reviewed studies, 3D printed orthoses were durable and showed similar or superior results in biomechanical parameters, kinematic parameters, and comfort evaluation compared to conventional orthoses. Based on these results, 3D printed orthoses appear to be of sufficient value to replace conventional orthoses in clinical practice. However, previous studies had a small percentage of randomized trials and fewer results comparing conventional and 3D printed orthoses. In particular, for a spinal orthosis, there is only one prospective observational study. In addition, some studies only confirmed satisfaction, which is an individual’s subjective indicator. Therefore, for 3D printed orthoses to be more actively utilized in clinical practice, more randomized trials should be conducted to minimize the risk of bias and ensure the validity of the study. Moreover, it is necessary to compare the effects of conventional orthosis and 3D printed orthosis and evaluate objective indicators such as joint ROM, pressure distribution, and kinematic data.
Acknowledgments
Funding: The present study was supported by a National Research Foundation of Korea Grant funded by the Korean government (grant number NRF-2019M3E5D1A02068106).
Footnote
Reporting Checklist: the authors have completed the NARRATIVE REVIEW reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1185
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1185). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chae DS, Kim DH, Kang KY, et al. The functional effect of 3D-printing individualized orthosis for patients with peripheral nerve injuries: three case reports. Medicine (Baltimore) 2020;99:e19791. [Crossref] [PubMed]
- Weinstein SL, Dolan LA, Wright JG, et al. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512-21. [Crossref] [PubMed]
- Cha YH, Lee KH, Ryu HJ, et al. Ankle-foot orthosis made by 3d printing technique and automated design software. Appl Bionics Biomech 2017;2017:9610468. [Crossref] [PubMed]
- Dombroski CE, Balsdon ME, Froats A. The use of a low cost 3D scanning and printing tool in the manufacture of custom-made foot orthoses: a preliminary study. BMC Res Notes 2014;7:443. [Crossref] [PubMed]
- Jin H, Xu R, Wang S, et al. Use of 3D-printed heel support insoles based on arch lift improves foot pressure distribution in healthy people. Med Sci Monit 2019;25:7175-81. [Crossref] [PubMed]
- Kim SJ, Kim SJ, Cha YH, et al. Effect of personalized wrist orthosis for wrist pain with three-dimensional scanning and printing technique: a preliminary, randomized, controlled, open-label study. Prosthet Orthot Int 2018;42:636-43. [Crossref] [PubMed]
- Telfer S, Woodburn J, Collier A, et al. Virtually optimized insoles for offloading the diabetic foot: A randomized crossover study. J Biomech 2017;60:157-61. [Crossref] [PubMed]
- Mo S, Leung SHS, Chan ZYS, et al. The biomechanical difference between running with traditional and 3D printed orthoses. J Sports Sci 2019;37:2191-7. [Crossref] [PubMed]
- Xu R, Wang Z, Ma T, et al. Effect of 3D printing individualized ankle-foot orthosis on plantar biomechanics and pain in patients with plantar fasciitis: A randomized controlled trial. Med Sci Monit 2019;25:1392-400. [Crossref] [PubMed]
- Xu R, Wang Z, Ren Z, et al. Comparative study of the effects of customized 3d printed insole and prefabricated insole on plantar pressure and comfort in patients with symptomatic flatfoot. Med Sci Monit 2019;25:3510-9. [Crossref] [PubMed]
- Zheng Y, Liu G, Yu L, et al. Effects of a 3D-printed orthosis compared to a low-temperature thermoplastic plate orthosis on wrist flexor spasticity in chronic hemiparetic stroke patients: a randomized controlled trial. Clin Rehabil 2020;34:194-204. [Crossref] [PubMed]
- Allan R, Woodburn J, Telfer S, et al. Knee joint kinetics in response to multiple three-dimensional printed, customised foot orthoses for the treatment of medial compartment knee osteoarthritis. Proc Inst Mech Eng H 2017;231:487-98. [Crossref] [PubMed]
- Kuo YR, Fang JJ, Wu CT, et al. Analysis of a customized cervical collar to improve neck posture during smartphone usage: a comparative study in healthy subjects. Eur Spine J 2019;28:1793-803. [Crossref] [PubMed]
- Mannisi M, Dell'Isola A, Andersen MS, et al. Effect of lateral wedged insoles on the knee internal contact forces in medial knee osteoarthritis. Gait Posture 2019;68:443-8. [Crossref] [PubMed]
- Tarrade T, Doucet F, Saint-Lô N, et al. Are custom-made foot orthoses of any interest on the treatment of foot pain for prolonged standing workers? Appl Ergon 2019;80:130-5. [Crossref] [PubMed]
- Chen YJ, Lin H, Zhang X, et al. Application of 3D-printed and patient-specific cast for the treatment of distal radius fractures: initial experience. 3D Print Med 2017;3:11.
- Chu CH, Wang IJ, Sun JR, et al. Customized designs of short thumb orthoses using 3D hand parametric models. Assist Technol 2020. [Epub ahead of print]. [Crossref] [PubMed]
- Guida P, Casaburi A, Busiello T, et al. An alternative to plaster cast treatment in a pediatric trauma center using the CAD/CAM technology to manufacture customized three-dimensional-printed orthoses in a totally hospital context: a feasibility study. J Pediatr Orthop B 2019;28:248-55. [Crossref] [PubMed]
- Lee KH, Kim DK, Cha YH, et al. Personalized assistive device manufactured by 3D modelling and printing techniques. Disabil Rehabil Assist Technol 2019;14:526-31. [Crossref] [PubMed]
- Liu Z, Zhang P, Yan M, et al. Additive manufacturing of specific ankle-foot orthoses for persons after stroke: a preliminary study based on gait analysis data. Math Biosci Eng 2019;16:8134-43. [Crossref] [PubMed]
- Portnova AA, Mukherjee G, Peters KM, et al. Design of a 3D-printed, open-source wrist-driven orthosis for individuals with spinal cord injury. PLoS One 2018;13:e0193106. [Crossref] [PubMed]
- Telfer S, Abbott M, Steultjens M, et al. Dose-response effects of customised foot orthoses on lower limb muscle activity and plantar pressures in pronated foot type. Gait Posture 2013;38:443-9. [Crossref] [PubMed]
- Telfer S, Abbott M, Steultjens MP, et al. Dose-response effects of customised foot orthoses on lower limb kinematics and kinetics in pronated foot type. J Biomech 2013;46:1489-95. [Crossref] [PubMed]
- Wang K, Shi Y, He W, et al. The research on 3D printing fingerboard and the initial application on cerebral stroke patient's hand spasm. BioMed Eng OnLine 2018;17:92. [Crossref] [PubMed]
- Bai H, Deng S, Bai D, et al. Recent advances in processing of stereocomplex-type polylactide. Macromol Rapid Commun 2017. [Crossref] [PubMed]
- Memarian F, Fereidoon A, Ahangari MG. Effect of acrylonitrile butadiene styrene on the shape memory, mechanical, and thermal properties of thermoplastic polyurethane. J Vinyl Addit Techn 2018;24:E96-104. [Crossref]