
Effect of combined treatment with pulsed electromagnetic field stimulation and sclerostin monoclonal antibody on changes in bone metabolism and pedicle screw augmentation in rabbits with ovariectomy-induced osteoporosis
Introduction
Orthopedic surgeons extensively use pedicle screws in the treatment of spinal diseases because of their three-column fixation and maintenance of reconstructed spine sequences (1-3). The low bone density and deterioration of the bone microarchitecture in osteoporotic patients often lead to bone fragility and a high risk of instrumentation failures, such as proximal kyphosis, screw loosening, pseudarthrosis formation and other osteoporosis-related complications (1). Osteoporosis-related complications can have a devastating effect on the quality of life because of temporary or permanent loss of function and other difficulties. Therefore, there is a strong demand for the improvement of internal fixation in osteoporotic bones. In the past few decades, there has been considerable progress in improving the stability of internal fixation, mainly in the optimization of materials, bone and screw interface enhancement, and the improvement of surgical techniques (4-8). However, the ideal measure is to enhance the quality and quantity of osteoporotic bones, that is, to improve bone density, increase the volume of cortical bone and cancellous bone, increase bone strength, and reduce the rate of osteoporotic fractures and internal fixation failures.
Sclerostin inhibits osteoblast differentiation and proliferation by inhibiting the Wnt/β-catenin signaling pathway (9). Antagonizing sclerostin by the use of a sclerostin monoclonal antibody has become a potential method for the treatment of osteoporosis (10,11). Pulsed electromagnetic field (PEMF) therapy is currently the most commonly used physical therapy for osteoporosis (12). The principle of the PEMF for treating osteoporosis is to use a low-frequency PEMF to change human bioelectricity, improve the biological field, promote osteoblast proliferation, enhance bone formation ability, and improve bone density (13).
However, the synergy between the two therapies has not been reported so far. In this study, we provide a reference for evaluating the therapeutic value of PEMF stimulation combined with the sclerostin monoclonal antibody for postmenopausal osteoporosis. We present the following article in accordance with the ARRIVE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-473).
Methods
Ovariectomy surgery
Experiments were performed under a project license (No. 2019 Wuyuan JS-042) granted by the Department of Laboratory Animal Science of Fudan University, in compliance with national guidelines for the care and use of animals. Forty 6-month-old healthy female New Zealand rabbits weighing 2.50±0.10 kg were housed and paired under strict supervision in the Fudan University Experimental Animal Center. Animals received standard food and water and were kept under climate-controlled conditions (21 °C, 12 h light/12 h darkness). One week after adaptive feeding, rabbits received bilateral ovariectomy under anesthesia to create an animal model of osteoporosis. The bone density of the middle femur region was measured regularly until six months after ovariectomy using dual-energy X-ray absorptiometry (DXA; PIXImus II; GE, USA) to observe changes in bone density.
Pedicle screw implantation
After the osteoporosis model was successfully established, all rabbits received pedicle screw implantation. Surgical procedures were performed aseptically under general anesthesia. Before surgery, rabbits received a single dose of antibiotics (enrofloxacin; 5 mg/kg body weight, Bayer, the Netherlands). The L4 vertebral body was selected as the pedicle screw fixation site. We chose the junction point between the transverse process of the vertebral body as a marker of the entry point. All pedicle screws were titanium alloy screws (WEGO Company, Shandong, China). All screws were 20 mm long and 2.0 mm in diameter. Fascia and skin were sutured in layers.
Experimental design
Ovariectomized rabbits were randomly divided into four groups, ten rabbits in each group, namely, the PEMF group, Scl-Ab group, PEMF+Scl-Ab group, and OVX control group. From the first day after surgery, rabbits in the PEMF group were treated with PEMF (TY-PEMF-B, Tianjin Tongye Technology, CHN, parameter: 15 Hz, 40 min/day, 5 days/week for 8 weeks); rabbits in the Scl-Ab group received subcutaneous injection of Scl-Ab (Amgen Inc., Thousand Oaks, CA, USA, dose 25 mg/kg, twice a week for 8 weeks); PEMF+Scl-Ab group rabbits received PEMF and Scl-Ab treatment at the same time for 8 weeks; OVX control group rabbits received the same dose of isotonic sodium chloride solution for 8 weeks. After eight weeks of intervention, all experimental animals were weighed and used DXA at the middle femur region to determine the areal bone mineral density (BMD).
Harvest of tissues
After eight weeks of treatment, all rabbits were euthanized by intraperitoneal injection of sodium pentobarbital. Rabbit blood samples were collected for testing bone metabolism indicators. The muscle tissue around the L3–5 vertebral bodies was removed; the L3–5 vertebral bodies were dissected, wrapped in wet gauze with saline, sealed, and stored in a −20 °C refrigerator for biological and biomechanical testing. L3 vertebral bodies were used to analyze bone microstructural parameters, L4 vertebral body screws were tested for biomechanical properties, and L5 vertebral bodies were tested for biological characteristics. All rabbits were intraperitoneally injected with tetracycline hydrochloride and calcein solution at a dose of 30 mg/kg and 15 mg/kg two days before sacrifice.
Micro-computed tomographic (microCT) scanning
The L3 vertebral body total 36 specimens were scanned using a desktop microcomputed tomographic system (GE Healthcare, London, Ontario, Canada), and the scanning parameter settings were as follows: voltage 50 kV, current 500 µA, scanning mode 360° rotation, exposure time 250 ms, and image plane resolution 1,024×1,024. Three-dimensional images of the bone tissue were obtained, and a quantitative analysis was performed using microCT built-in software to get the following bone microstructural parameters: bone volume fraction (bone volume total volume, BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), and trabecular spacing (Tb.Sp).
Biomechanical testing
The maximum screw pulling-out force was determined using the materials testing system 850 (MTS, Minneapolis, MN, USA) machine. The L4 vertebral bodies total of 36 specimens were embedded exposing only the screw head. A custom-made jig was used to grasp the screw head, and the specimen was held rigidly at the other end of the jig. Screws inside the specimens were pulled until the occurrence of failure at a constant speed of 10 mm/min. Strength and displacement were obtained in real-time using a computerized data acquisition system with a sampling rate of 10 Hz. The maximum screw pulling-out force was determined as the maximum point on the strength-displacement curve where failures occurred.
The maximum failure power consumption was first analyzed by implementing a sinusoidal, cyclic (1.0 Hz) compressive force to the screw head. A rotation axis at the screw head allowed free rotation orthogonal to the screw axis with all other degrees of freedom between the loading piston and screw being fixed. Testing was stopped when the displacement of the screw head reached 2.0 mm.
Histological analysis
The L5 vertebral bodies total of 36 specimens were placed in 10% formalin for 24 h, fixed in 70% ethanol, dehydrated with gradient ethanol, and degreased with xylene. They were then embedded in methyl methacrylate without decalcification and cut into 30 µm sections in the longitudinal direction of the screws. Static and dynamic histomorphometry measurements were performed using a semiautomated digital image analysis system (Osteometrics, Decatur, GA, USA). Static histomorphology was measured using Masson-Goldner staining. The osteoid surface is the proportion of the periplasmic circumference to that of the entire trabecular bone around the screws (×100%). Bone-screw contact is the ratio of the direct contact part of the whole thread length (×100%). Bone ingrowth is the ratio of all new cancellous bone areas to the total thread area (×100%). Mineral deposition rate (MAR) (µm/day) was defined as follows: on the new bone generated near the screws, the average spacing of two adjacent fluorescent double scales divided by the interval number of days (10 days).
Statistical analysis
All data are expressed as mean ± SD deviation. One-way ANOVA test analyzes the results of multiple groups. Statistical comparisons were made with SPSS 18.0 statistical software for Windows. A P value <0.05 was considered significant.
Results
Osteoporosis animal model production
At the beginning of the study, the BMD of the forty rabbits was 0.243±0.021 g/cm2, but at six months after ovariectomy, it was 0.156±0.035 g/cm2, which was 35.8% lower than the BMD before the operation. This difference was statistically significant. (P=0.003, <0.05), suggesting the successful establishment of the osteoporosis model. There was no wound infection or animal death after surgery. During the operation of pedicle screw implantation, four rabbits died of massive hemorrhage due to excessive anesthesia and improper operation. These animals belonged to the PEMF group, Scl-Ab group, PEMF+Scl-Ab group, and OVX control group, and thus, 36 rabbits entered the trial evaluation, with nine rabbits in each group.
Serum BALP and TRACP5b
Figure 1 reveals that the serum BALP level was lower in the OVX group than in the respective treatment groups (P<0.05). The serum BALP level was statistically similar in the PEMF, Scl-Ab, and PEMF+Scl-Ab groups (P>0.05). The serum TRACP5b level in the OVX group was significantly higher than that in all treatment groups (P<0.05). The level of serum TRACP5b in the PEMF+Scl-Ab group was considerably lower than that in the Scl-Ab group and the PEMF group (P<0.05).

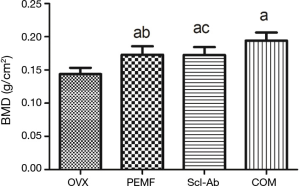
BMD
As shown in Figure 2, at eight weeks postoperatively, the mean BMD of the middle femur region in the OVX group was 0.14±0.02 g/cm2, which was not significantly different from that before treatment (P>0.05). However, the BMD of the PEMF group, Scl-Ab group, and PEMF+Scl-Ab group increased by 20.3%, 19.9%, and 35.0%, respectively. Besides, the BMD of the PEMF+Scl-Ab group was significantly higher than that in the PEMF group and the Scl-Ab group (P<0.05).
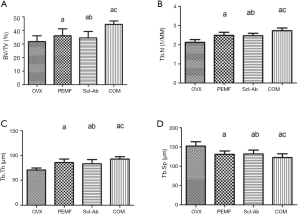
MicroCT scan results and analysis
MicroCT images and microstructure parameters of the L3 are presented in Figures 3 and 4. In the OVX group, the BV/TV, Tb.N, and Tb.Th indicators were significantly lower than those in the treatment groups, while Tb.Sp was significantly increased. Compared with BV/TV in the OVX group, BV/TV increased by 13.6%, 8.4% and 39.8% in the PEMF group, Scl-Ab group and PEMF+Scl-Ab group, respectively. Tb.N was 17.3%, 16.3% and 28.5% increased, respectively; Tb.Th was 21.1%, 17.5%, and 30.8% increased, respectively; and Tb.Sp was 14.0%, 13.5%, and 19.6% decreased, respectively.
Biomechanical testing
As shown in Figure 5, the maximum pulling force of the L4 vertebral pedicle screws in the OVX group was 17.21±5.12 N, and the maximum failure power consumption was 1.42±0.45 J. The maximum pulling force of the PEMF group, Scl-Ab group, and PEMF+Scl-Ab group was higher than that of the OVX group, increasing by 14.0%, 15.0% and 19.1%, respectively. This difference was statistically significant (P<0.05), but the differences among the three treatment groups were not statistically significant (P>0.05). The maximum failure power consumption of the PEMF group, Scl-Ab group, and PEMF+Scl-Ab group was higher than that of the OVX group, increasing by 27.9%, 27.2% and 33.6%, respectively. This difference was statistically significant (P<0.05), but the differences among the three treatment groups were not statistically significant (P>0.05).

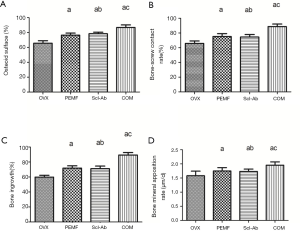
Histological analysis
From Figure 6, compared with the OVX group, the osteoid surface, bone-screw contact rate, bone ingrowth, and bone mineral apposition rate of the L5 vertebral pedicle screw in the treatment groups were significantly increased (P<0.05). The osteoid surface, bone-screw contact rate, bone ingrowth, and bone mineral apposition rate of the PEMF+Scl-Ab group were significantly higher than those of the PEMF group and Scl-Ab group, and the difference was statistically significant (P<0.05), suggesting that the osteogenesis activity of the PEMF+Scl-Ab group was significantly better than that of the single measure group.
Discussion
In this study, ovariectomized New Zealand white rabbits that underwent pedicle screw fixation were selected as the study subjects. The treatment groups received PEMF magnetic therapy, subcutaneous Scl-Ab injection, PEMF+Scl-Ab treatment together, and the OVX control group received subcutaneous injection of saline. Bone turnover index detection, bone density measurement, bone microstructure parameters and biomechanical properties around the screws showed that Scl-Ab+PEMF combined therapy enhanced the bone density and screw fixation strength, which were superior to those with a single treatment.
To avoid the failure of internal fixation, patients with osteoporosis need to extend the recuperative time after surgery, but such sedentary periods may lead to further loss of bone mass (14). Long-term unloaded patients, such as patients with spinal cord injury, have elevated serum SOST levels that are positively associated with the progression of osteoporosis (15). Inhibiting SOST function can increase bone formation and reduce bone loss. Mice knocked out the SOST gene show progressive bone mass and increased bone strength, while SOST gene-overexpressing mice have a low bone mass (16). What is more, increasing SOST levels secreted by bone cells are important factors in the pathogenesis of postmenopausal osteoporosis. Xu et al. (17) reported that the serum SOST content of Chinese women after menopause was higher than that of premenopausal women, and the SOST content was negatively correlated with lumbar spine BMD. Subcutaneous use of estrogen can reduce serum SOST levels in postmenopausal women. The world’s first sclerostin monoclonal antibody (AMG785, romosozumab) phase I clinical randomized controlled double-blind study was released in 2011. In this clinical study, 72 healthy postmenopausal women were selected as subjects and received a single romosozumab injection for a maximum of 85 days. The results showed that as the intervention dose increased, romosozumab increased the content of PINP, BALP, and osteocalcin in the serum of the subjects in a dose-dependent manner and decreased the content of β-CTX. Meanwhile, at the end of the intervention, the lumbar spine bone density increased by 5.3%, and the hip bone density increased by 2.8% (18). In our study, Scl-Ab was injected subcutaneously for eight weeks. Compared with the OVX group, BMD, bone metabolic markers, and bone microstructural parameters were significantly improved.
Researchers used zoledronate in combination with a PEMF to treat postmenopausal osteoporosis. The results showed that zoledronate combined with the PEMF could effectively improve BMD, reduce bone turnover biomarker levels, and inhibit bone loss in postmenopausal osteoporosis patients (19). Referring to previous studies, we set the parameters of PEMF to a magnetic strength of 3.8 mT, a field frequency of 15 Hz, lasting 40 min/day for eight weeks. Our results indicated that PEMF could improve BMD, bone microstructural parameters and biomechanical properties, similarly to previous studies (20). Most detailed findings about PEMF treatment, such as duration, intensity and frequency of exposure have been reported. Generally in animal fracture models, the initial repair speed was significantly accelerated in the early stage of fracture repair, however, prolonged exposure in the late stage of fracture repair did not improve bone healing, in fact, was detrimental to the process (21-23). Meanwhile, PEMF treatment in the active proliferation stage accelerated cellular proliferation. In the differentiation stage (based on alkaline phosphatase activity), treatment enhanced cellular differentiation and increases tissue-like formation. In the mineralization stage, there was a decrease in bone tissue like formation, and a stoppage of proliferation. Refer to the above research results, we set the duration of PEMF treatment to 8 weeks after pedicle screw implantation. Given the different pathological states of osteoporosis and local bone mechanics, interfering with bone turnover, especially promoting bone formation, directly enhancing the quality and quantity of bone at the fixed site is an ideal treatment for osteoporosis and prevention of internal fixation failure. The dynamic balance of bone turnover is the basis for maintaining bone density (24). The metabolic index of bone turnover can be used to assess changes in bone resorption and bone formation. In our study, the ELISA results indicated that all of the treatments inhibited bone resorption and promoted bone formation. Besides, the PEMF+Scl-Ab combination therapy inhibited bone resorption more efficiently than any of the single treatment did. We conclude that combination therapy may inhibit bone resorption through the additive effects of different treatments.
Biological and biomechanical parameters can also be used to assess osteoporosis status. In this study, compared with the corresponding settings in the OVX group, the osteoid surface, bone-screw contact rate, bone ingrowth and bone mineral apposition rate of the treatment groups increased at different levels eight weeks after surgery. There was a large amount of new trabecular bone around the screws in the treatment groups. The amount and spatial structure of the trabecular bone around the screws were significantly better than those of the OVX group, forming a better screw-bone interface. Through the mechanical test, the maximum pulling force and maximum failure power consumption of the pedicle screws in the treatment groups were significantly enhanced.
In conclusion, PEMF+Scl-Ab combination therapy can improve the osteoporotic bone microstructure and enhance bone mechanical strength by inhibiting bone resorption and promoting bone formation. This topic deserves further study to enhance the stability of internal fixation under osteoporotic conditions.
Conclusions
The present investigation confirmed that (I) combination therapy of Scl-Ab and PEMF can improve BMD and the mechanical strength of pedicle screws in osteoporotic vertebral bodies in rabbits with postmenopausal osteoporosis and that (II) PEMF+Scl-Ab combination therapy can enhance the osteoporotic bone microstructure and bone mechanical strength, which may be attributed to the inhibition of bone resorption and promotion of bone formation. Thus, we conclude that combination therapy may inhibit bone resorption through the additive effects of different treatments.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the ARRIVE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-473
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-473
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-473). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Experiments were performed under a project license (No. 2019 Wuyuan JS-042) granted by the Department of Laboratory Animal Science of Fudan University, in compliance with national guidelines for the care and use of animals.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bjerke BT, Zarrabian M, Aleem IS, et al. Incidence of Osteoporosis-Related Complications Following Posterior Lumbar Fusion. Global Spine J 2018;8:563-9. [Crossref] [PubMed]
- Lehman RA Jr, Kang DG, Wagner SC. Management of osteoporosis in spine surgery. J Am Acad Orthop Surg 2015;23:253-63. [Crossref] [PubMed]
- Rong Z, Zhang F, Xiao J, et al. Application of Cement-Injectable Cannulated Pedicle Screw in Treatment of Osteoporotic Thoracolumbar Vertebral Compression Fracture (AO Type A): A Retrospective Study of 28 Cases. World Neurosurg 2018;120:e247-58. [Crossref] [PubMed]
- Jia C, Zhang R, Xing T, et al. Biomechanical properties of pedicle screw fixation augmented with allograft bone particles in osteoporotic vertebrae: different sizes and amounts. Spine J 2019;19:1443-52. [Crossref] [PubMed]
- Kiner DW, Wybo CD, Sterba W, et al. Biomechanical analysis of different techniques in revision spinal instrumentation: larger diameter screws versus cement augmentation. Spine (Phila Pa 1976) 2008;33:2618-22. [Crossref] [PubMed]
- Li HM, Zhang RJ, Gao H, et al. Biomechanical Fixation Properties of the Cortical Bone Trajectory in the Osteoporotic Lumbar Spine. World Neurosurg 2018;119:e717-27. [Crossref] [PubMed]
- Yazu M, Kin A, Kosaka R, et al. Efficacy of novel-concept pedicle screw fixation augmented with calcium phosphate cement in the osteoporotic spine. J Orthop Sci 2005;10:56-61. [Crossref] [PubMed]
- Taniwaki Y, Takemasa R, Tani T, et al. Enhancement of pedicle screw stability using calcium phosphate cement in osteoporotic vertebrae: in vivo biomechanical study. J Orthop Sci 2003;8:408-14. [Crossref] [PubMed]
- Ke HZ, Richards WG, Li X, et al. Sclerostin and Dickkopf-1 as therapeutic targets in bone diseases. Endocr Rev 2012;33:747-83. [Crossref] [PubMed]
- Hay E, Bouaziz W, Funck-Brentano T, et al. Sclerostin and Bone Aging: A Mini-Review. Gerontology 2016;62:618-23. [Crossref] [PubMed]
- Minisola S, Cipriani C, Occhiuto M, et al. New anabolic therapies for osteoporosis. Intern Emerg Med 2017;12:915-21. [Crossref] [PubMed]
- Waldorff EI, Zhang N, Ryaby JT. Pulsed electromagnetic field applications: A corporate perspective. J Orthop Translat 2017;9:60-8. [Crossref] [PubMed]
- Catalano A, Loddo S, Bellone F, et al. Pulsed electromagnetic fields modulate bone metabolism via RANKL/OPG and Wnt/beta-catenin pathways in women with postmenopausal osteoporosis: A pilot study. Bone 2018;116:42-6. [Crossref] [PubMed]
- Szollar SM, Martin EM, Sartoris DJ, et al. Bone mineral density and indexes of bone metabolism in spinal cord injury. Am J Phys Med Rehabil 1998;77:28-35. [Crossref] [PubMed]
- Li D, Lin Z, Meng Q, et al. Cannabidiol administration reduces sublesional cancellous bone loss in rats with severe spinal cord injury. Eur J Pharmacol 2017;809:13-9. [Crossref] [PubMed]
- Spatz JM, Wein MN, Gooi JH, et al. The Wnt Inhibitor Sclerostin Is Up-regulated by Mechanical Unloading in Osteocytes in Vitro. J Biol Chem 2015;290:16744-58. [Crossref] [PubMed]
- Xu XJ, Shen L, Yang YP, et al. Serum sclerostin levels associated with lumbar spine bone mineral density and bone turnover markers in patients with postmenopausal osteoporosis. Chin Med J (Engl) 2013;126:2480-4. [PubMed]
- McColm J, Hu L, Womack T, et al. Single- and multiple-dose randomized studies of blosozumab, a monoclonal antibody against sclerostin, in healthy postmenopausal women. J Bone Miner Res 2014;29:935-43. [Crossref] [PubMed]
- Qin Y, Qiu B, Zhu S, et al. Clinical efficacy of zoledronic acid combined with pulsed electromagnetic field therapy on postmenopausal osteoporosis. Chinese Journal of Osteoporosis 2015;21:945-8.
- Zhou J, Liao Y, Xie H, et al. Effects of combined treatment with ibandronate and pulsed electromagnetic field on ovariectomy-induced osteoporosis in rats. Bioelectromagnetics 2017;38:31-40. [Crossref] [PubMed]
- Ibiwoye MO, Powell KA, Grabiner MD, et al. Bone mass is preserved in a critical-sized osteotomy by low energy pulsed electromagnetic fields as quantitated by in vivo micro-computed tomography. J Orthop Res 2004;22:1086-93. [Crossref] [PubMed]
- Midura RJ, Ibiwoye MO, Powell KA, et al. Pulsed electromagnetic field treatments enhance the healing of fibular osteotomies. J Orthop Res 2005;23:1035-46. [Crossref] [PubMed]
- Haddad JB, Obolensky AG, Shinnick P. The biologic effects and the therapeutic mechanism of action of electric and electromagnetic field stimulation on bone and cartilage: new findings and a review of earlier work. J Altern Complement Med 2007;13:485-90. [Crossref] [PubMed]
- Ikeda K, Takeshita S. The role of osteoclast differentiation and function in skeletal homeostasis. J Biochem 2016;159:1-8. [Crossref] [PubMed]



