
Influence of transitional care on the self-care ability of kidney transplant recipients after discharge
Introduction
Chronic renal failure is a common clinical condition, and allogeneic kidney transplantation remains the preferred treatment. However, the success of kidney transplantation greatly depends on care, especially the transitional care after discharge. Poor adherence to follow-up and medication leads to many avoidable complications, which affect the quality of life and even lower the survival rates of both grafts and patients. Transitional care is defined as a set of actions designed to ensure the coordination and continuity of health care as patients transfer between different locations (e.g., from hospitals to home) or different levels of care within the same location (e.g., between different departments in the same hospital). The term usually refers to the continuum of care from hospital to home and includes the discharge plan made by the hospital, referral, and continuous follow-up visits, along with the health guidance and education received after the patient returns home or to their community (1-3). Transitional care is an extension of in-patient nursing and plays a key role in lowering rehospitalization rates, improving the quality of life after discharge, and reducing health-care costs.
Continuous care has been adopted as part of the treatment of many clinical diseases, with satisfactory results. For instance, some studies (4,5) used a concurrent control study to carry out continuous nursing intervention for patients after kidney transplantation. The results showed that the self-management ability of the intervention group after discharge was better than that of the conventional group. However, there might have been individual differences between the two groups of patients in the concurrent control study, which could be improved through a self-controlled design. Thus far, few researchers have employed their own before-and-after studies to better verify the effectiveness of continuing care. Therefore, with the aim of improving the self-care ability and quality of life of kidney transplantation patients, our hospital established a kidney transplantation transitional care group. This involved the evaluation of kidney transplant patients before and after the implementation of the continuous care nursing plan by assessing the disease knowledge and the effect of self-care ability in discharged patients. It is hope that the results of this study can provide a valuable reference for the continuous care of transplant patients discharged from hospitals.
We present the following article in accordance with the SURGE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1120).
Methods
Subjects
A total of 100 recipients who underwent kidney transplantation in the department of urology of our hospital from January 2015 to March 2018 were selected as study subjects using the convenience sampling method. The inclusion criteria were as follows: (I) the surgical operation was successful, and the postoperative recovery was smooth; (II) aged 18 years or older, without intellectual and cognitive impairments, and with the ability to speak and comprehend Chinese; (III) without serious diseases in other systems or organs; (IV) living or residing in the suburbs or downtown area of the city where our center is located; (V) voluntarily participated in the study and signed informed consent. The exclusion criteria were as follows: (I) unwilling to participate in this study; and (II) living or residing in remote areas with poor transportation or communication conditions. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013), and was approved by the Institutional Review Board of The First Affiliated Hospital of Soochow University [approval number: (2020)068].
Interventions
Establishment of a transitional care team
A transitional care team for kidney transplant recipients was established. The teams had 10 members including 2 kidney transplant surgeons, 2 attending physicians, and 6 kidney transplant specialist nurses. All members received 1 month of training on transitional care and passed the examinations. Among them, kidney transplant experts, attending physicians, and specialist nurses were mainly responsible for the care, evaluation, and education of patients during their hospital stay; the attending physicians and specialist nurses also regularly followed-up with and monitored the care, diet, exercise, and medication of patients after their discharge, so as to ensure the smooth implementation of the transitional care. In order to ensure the integrity and continuity of the patient data, one researcher was assigned to the registration and maintenance of the subject database, which contained the patient’s general data, findings during hospitalization and follow-up visits, telephone follow-up data, family visit data, and data collected during patient events.
Development and implementation of the transitional care program
One week before discharge, the primary nurse assessed the patient and recorded the patient’s diet, activities, medications, complications (if any), mental state, sleep, excretions, and psychological conditions; after obtaining consent from the patient, the nurse created the patient’s Individual File, in which the general data of the patient were entered. Health education was offered according to the specific conditions of the patient, and a discharge care plan was created accordingly. After the patient was discharged, members of the transitional care team offered transitional care to the patient. The content and frequency of transitional care were as follows:
- Telephone visits: the first telephone visit was conducted 72 hours after the patient was discharged and then on a monthly basis, and the “Record of Telephone Visit” form was filled out. The content of the telephone visits included the patient’s general condition, graft rejection and complications, psychological state, healthy behaviors, and environment. More specifically, it consisted of the following: (i) general conditions, including body temperature, pulse, blood pressure, body weight, 24-h urine volume, etc.; (ii) graft rejection and complications, including discomfort/pain at the transplanted kidney area, elevated body temperature, increased blood pressure, increased body weight, decreased urine output, infection, etc.; (iii) psychological state, including the assessment of patient participation in various social activities and the offer of psychological counseling if abnormal conditions were found; (iv) healthy behaviors, including the assessment of the patient’s compliance with the healthy behaviors/lifestyles; and (v) environment, including the evaluation of the patient’s home environment to improve any adverse factors.
- Outpatient visits: the patients were required to undergo outpatient visits on a weekly basis after discharge and every 2 weeks after 6 months. When the patient visited the outpatient department, the attending physician assessed the patient using content identical to that of the telephone visits; meanwhile, relevant laboratory examinations were performed. According to the assessment and examination results, health education was provided to improve the patient’s self-care ability.
- Family visits: after the patient was discharged, family visits were performed every month, and the follow-up record was filled out. The patient’s lifestyle, self-monitoring method, and home environment were evaluated and guided, with the content being consistent with that of the telephone visit.
- Patient events: patient events were held annually, which helped the patients to communicate with each other and relieve their psychological pressure.
Survey tools and methods
Questionnaire on disease knowledge
A self-designed questionnaire on disease knowledge was used to assess the patients’ knowledge on disease 1 week before discharge and 1 and 6 months after discharge. The questionnaire involved six dimensions: (I) self-monitoring, including the accurate measurement of body temperature, pulse, blood pressure, and body weight; (II) accurate recording of the 24-hour urine volume and fluid intake and output; (III) medications, including the immunosuppressants that were rationally administered as directed by the doctor; (IV) exercise, including the encouragement to perform appropriate aerobic exercises; (V) reasonable diet; and (VI) early recognition of rejection reactions, typically including symptoms of weight gain, increased blood pressure, increased body temperature, and decreased urine output. Each dimension had 5 single-answer questions worth 0–4 points each, and the total score was 120 points. A higher score indicated better disease knowledge. This questionnaire has been repeatedly revised with input from experts and has a Cronbach’s α coefficient of 0.81.
Exercise of self-care agency (ESCA) scale
The self-care ability of the patients was assessed by using the ESCA scale 1 week before discharge and 1 and 6 months after discharge. Based on Orem’s self-care theory, the scale has 43 items, which consist of four dimensions: self-concept (items 1–8), self-nursing responsibility (items 9–14), self-care skills (items 15–26), and health knowledge level (items 27–43). Each item is rated on a 5-point Likert scale. The total score of the ESCA ranges from 0 to 172, and a higher score represents a higher self-care ability (low, 0–57 points; moderate, 58–115 points; and high, 116–172 points) (6). The scale was translated into Chinese in the year 2000, and the Chinese version showed good validity and reliability in the Chinese populations in Taiwan Province of China (6). In our current study, the content validity index (CVI) of the scale was 1.00, and the Cronbach’s α coefficients of different dimensions ranged from 0.86 to 0.92.
Nursing service satisfaction
Nursing satisfaction is the relative relation between patients expectation of nursing service and their actual feeling after service. In this study, patients gave a rating out of 5 points in response to the following closed-ended question: “Would you please rate your satisfaction with the discharge care service?”. The Likert scale was adopted, with a higher score indicating a higher patient satisfaction with the nursing service.
Statistical analysis
Data were processed and analyzed using SPSS 16.0 software package. Measurement data are expressed as mean ± standard deviation (mean ± SD). Comparisons of the scores among multiple groups were based on the analysis of variance (ANOVA) with repeated measures, and rates were compared using Chi-square test. A P value of <0.05 (two-sided) was considered statistically significant.
Results
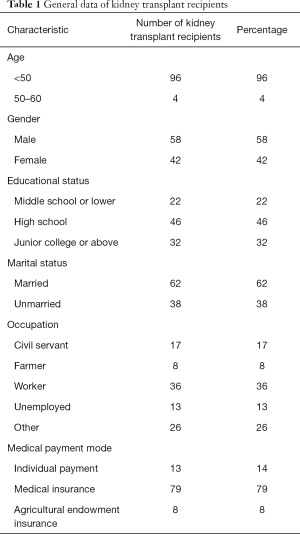
General data of kidney transplant recipients
A total of 100 kidney transplant recipients [including 58 males (58%) and 42 females (42%)] were included in this study. Among them 96 (96%) were younger than 50 years old, and 4 (4%) were aged between 50 and 60 years. For educational status, 22 patients (22%) had an education background of middle school or lower, 46 (46%) graduated from high school, and 32 (32%) graduated from junior college or above; 62 (62%) had been married and 38 (38%) were currently unmarried; their occupation status included civil servants (n=17, 17%), farmers (n=8, 8%), workers (n=36, 36%), unemployed (n=13, 13%), and others (n=26, 26%). The medical payment modes included individual payment (n=13, 13%), medical insurance (n=79, 79%), and agricultural endowment insurance (n=8, 8%) (Table 1).
Full table
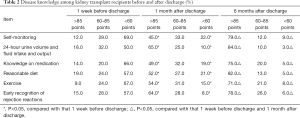
Disease knowledge among kidney transplant recipients
The questionnaire-based survey showed that the disease knowledge among these 100 kidney transplant recipients gradually increased 1 and 6 months after discharge (both P<0.05) (Table 2).
Full table
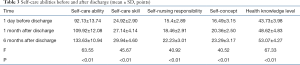
Self-care ability before and after discharge
The self-care ability among these 100 kidney transplant recipients gradually increased 1 and 6 months after discharge (both P<0.01) (Table 3).
Full table
Comparison of nursing service satisfaction at different time points
Compared with the day before discharge, the nursing service satisfaction of 100 kidney transplant patients gradually improved 1 month after discharge and 6 months after discharge, and the difference was statistically significant (P<0.05) (Table 4).

Full table
The occurrence of complications in patients
After continuous nursing service intervention, two cases of mild rejection and eight cases of pulmonary infection occurred, with a complication rate of 10%. Four cases of mild rejection and one severe rejection, along with ten cases of pulmonary infection and three cases of drug poisoning, occurred in the patients receiving routine care in the first 2 years, and the incidence of complications was 18%. The incidence of complications in patients with continuous nursing service intervention was lower than that in patients with conventional nursing intervention (P<0.05).
Discussion
Transitional care improved the patients’ disease knowledge
The transitional care team conducted a 6-month follow-up study on the patients and found that the patients’ self-care ability had constantly improved in terms of self-monitoring of vital signs, recognition of rejection reactions, exercise, reasonable diet, and medication adherence. It has also been reported that mobile health interventions have achieved the goals of transitional care (7). In addition to telephone visits, our transitional care team also offered health education to the patients via outpatient visits, home visits, and patient events. The health education included self-monitoring methods, recognition of rejection reactions, exercise, reasonable diet, and infection prevention. After the continuous intervention by the team members, the level of disease knowledge showed significant improvement 6 months after discharge (P<0.05, compared with the level 1 week before discharge and 1 month after discharge), which was consistent with the findings of Low et al. (8). Furthermore, the members of the transitional care team regularly assessed the patients and provided health guidance by answering their questions and organizing patient events (which allowed the patients to communicate with each other and share their experiences); thus, the patients had a greater knowledge of the disease and of how to follow a healthy lifestyle.
Transitional care improved the self-care ability of kidney transplant recipients
A higher ESCA score indicates higher self-care ability (9). In our current study, the ESCA score was 133.63±10.94 points 3 months after discharge, which was significantly higher than that 1 week before discharge [92.13±13.74) points] and 1 month after discharge [109.92±12.08) points] (both P<0.01). Therefore, transitional care, which is offered by telephone visits, outpatient visits, home visits, and patient events, can improve patient management and increase their self-care ability. The establishment of the transitional care team helps to optimize the content of transitional care and lower the pain and psychological burden of patients, thereby decreasing the readmission rate, reducing the waste of health resources, and improving the quality of life of patients. This is consistent with the nursing management goals required by the Clinical Practice Guidelines for Postoperative Nursing of Renal Transplant Recipients (10). Notably, patient events are particularly helpful for the kidney transplant recipients during transitional care. These events allow the experienced patients to share their success stories with other patients and enable the patients to discuss their experiences, especially their solutions to common problems. The patients agree that the patient events are quite informative and improve their social skills.
The influence of continuous nursing intervention on nursing service satisfaction of renal transplant recipients
The nursing service satisfaction survey is one of the most commonly used indexes to evaluate nursing effect. Nurses make continuous nursing service plans according to patients' physical recovery after discharge, mainly including telephone follow-up, kidney transplant outpatient follow-up, family follow-up, kidney transplant patient association, etc. The results of this study showed that, compared with the day before discharge, the nursing service satisfaction scores of 100 kidney transplant patients were gradually improved 1 month after discharge and 6 months after discharge (P<0.05). As can be seen from the results of the data, this is similar to the results of similar studies (11). This indicates that the continuous nursing service can meet the health-care needs of patients, and improve patients' satisfaction with the content, form, and effects of the nursing service.
Despite these encouraging findings, our study was limited by the duration of interventions. Thus, the long-term effectiveness of transitional care after discharge warrants further investigation.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1120
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1120
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-1120). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013) and was approved by the Institutional Review Board of The First Affiliated Hospital of Soochow University [approval number: (2020)068]. Each recipient provided written informed consent for participation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Jiang JW, Zhou YJ, Hu HF, et al. Research on relationship between self-efficacy and quality of life in patients with diabetic complications. Shanghai Nursing 2011;11:13.
- Coleman EA, Boult C. American Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc 2003;51:556-7. [Crossref] [PubMed]
- Xu JX. Research advance in transitional care in China. Chinese Nursing Management 2012;12:18-9.
- Duan YZ, Li YH, Lu XY. Application of continuous nursing in self-management of discharged patients after kidney transplantation. Int J Nurs 2018;37:2995-8.
- Tang M. Application of continuous nursing in selfmanagement of discharged patients after kidney transplantation. Chinese General Practice Nursing 2015;13:2226-7.
- Wang HH, Laffrey SC. Preliminary development and testing of instruments to measure self-care agency and social support of women in Taiwan. Kaohsiung J Med Sci 2000;16:459-67. [PubMed]
- Cho YM, Lee S, Islam SMS, et al. Theories Applied to m-Health Interventions for Behavior Change in Low- and Middle-Income Countries: A Systematic Review. Telemed J E Health 2018;24:727-41. [Crossref] [PubMed]
- Low JK, Williams A, Manias E, et al. Interventions to improve medication adherence in adult kidney transplant recipients: a systematic review. Nephrol Dial Transplant 2015;30:752-61. [Crossref] [PubMed]
- Yamashita M. The exercise of self-care agency scale. West J Nurs Res 1998;20:370-81. [Crossref] [PubMed]
- Baker RJ, Mark PB, Patel RK, et al. Renal association clinical practice guideline in post-operative care in the kidney transplant recipient. BMC Nephrol 2017;18:174. [Crossref] [PubMed]
- Boter H. Multicenter randomized controlled trial of an outreach nursing support program for recently discharged stroke patients. Stroke 2004;35:2867-72. [Crossref] [PubMed]


