Herbal therapy treatment in thromboangiitis obliterans: a retrospective clinical study
Introduction
Thromboangiitis obliterans (TAO) is a segmental nonatherosclerotic inflammatory disorder that involves the small and medium arteries, veins, and nerves of the extremities primarily. Von Winiwarter provided the first description of a patient with TAO in 1879. TAO takes its name from a paper presented in 1908 at a meeting of the Association of American Physicians by Leo Buerger (1,2). At that meeting, he discussed a condition that the disease affected young adults and was characterized by thrombotic vascular occlusions of the lower limbs. The resulting ischemia is associated with rest pain and gangrene (Figure 1).
Although most patients are young, with the usual age of onset less than 45–50 years, men, and chronic tobacco smokers who present with distal extremity ischemia, ischemic ulcers, or frank gangrene of the toes or fingers. A few female patients also suffer from this disease. In some patients, there is recurrent thrombophlebitis, which occurs mostly in the dorsal foot and superficial veins of the calf (1-3).
In the ancient texts of traditional Chinese medicine, there were incidents of TAO more than two thousand years ago during the time of the Miraculous Pivot. “Miraculous Pivot” contains: “the name, main symptoms, a treatment plan of the disease. It is mentioned that the disease can lead to amputation.” Herbs in the USA and many European countries have been prepared as capsules, lotion, tablets, teas, medicines, juice extracts, tincture, and ointments (4). Herbal therapy has also been used to treat many vascular diseases (5).
Therefore, it is hypothesized that the simultaneous usage of herbal medications with modern management of TAO may serve to improve patient outcomes. Some traditional Chinese medicines have been shown to have bactericidal effects. For example, honeysuckle has an excellent inhibitory effect on common methicillin-resistant coccus aureus, escherichia coli, penicillium, bacillus subtilis, aspergillus Niger and aspergillus flavus, etc. (6,7). The Tuoju lotion used in this study is the internal preparation made by the Dongfang Hospital in Beijing. This formulation is easy to store, transport, and apply to affected areas facilitating patient compliance. Because this Tuoju lotion, in particular, is manufactured at Dongfang hospital, it also has beneficial characteristics including quality control during the manufacturing process and less adverse medication reactions due to close follow-up in an outpatient setting. This lotion has been used at Dongfang Hospital since 2007. This retrospective analysis was aimed to evaluate the efficacy of “Wenyang Tongluo” Chinese herbal medicine for the treatment of TAO. The main herbal ingredients of Tuoju lotion includes 30 g of Guizhi (Ramulus Cinnamomi), 15 g of Honghua (Flos Carthami), 15 g of Ru Xiang (Olibanum), 15 g of Moyao (Myrrha), 10 g of Chuanjiao (Zanthoxylum bungeanum Maxim), 15 g of Jinyinhua (Flos Lonicerae), 15 g of Sumu (Ligum Sappan), 30 g of Tougucao (Caulis Impatientis), 15 g of Jixueteng (Caulis Spatholobi), 15 g of Qiannianjian (Rhizoma Homalomenae), 15 g of Zhangnao (Camphora). We present the following article in accordance with the “5-STROBE Checklist” guideline checklist.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-19-578).
Methods
The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Regional Ethics Committee of Dongfang Hospital of Beijing University of Chinese Medicine (No. 2010-16), and informed consent was taken from all the patients.
Patients
There are many diagnostic criteria for TAO (8,9): Olin’s criteria (10), Papa’s scoring system (11), and Japanese standards (12) are all frequently accepted and referred to in modern medical literature.
Clinical criteria—a clinical diagnosis can be established with the following commonly used standards:
- Age less than 45 years;
- Current or recent history of tobacco use;
- Distal extremity ischemia (objectively noted on vascular testing);
- Typical arteriographic findings of TAO;
- Exclusion of autoimmune disease, thrombophilia, diabetes, and proximal embolic sources.
Diagnostic criteria
Diagnostic criteria set by Traditional Chinese Medicine Association. In November 2019, the Chinese Association of Integrated Traditional and Western Medicine Peripheral Vascular Disease Professional Committee TAO Expert committee discussed through the “TAO” expert consensus of integrated traditional and western medicine (4,13). TCM syndrome differentiation is based on the standard of diagnosis and curative effect of peripheral vascular diseases (4).
Criteria
(I) Age of onset <50 years; (II) current (or recent) history of smoking; (III) (i) presence of distal extremity ischemia (infra-popliteal or infra-brachial) with symptoms of claudication, rest pain, acid, swelling, hemp, wood (one or more signs appear); (ii) a cold or burning sensation (1 symbol); (iii) skin, hair, muscle, toes (fingers) are not benign (more descriptive here is probably better, consider bullet points for better formatting); (iv) the leg or foot repeatedly appears in migratory thrombophlebitis; (IV) documented by noninvasive vascular testing such as ultrasound; (V) exclusion of thrombophilia, autoimmune or connective tissue diseases, and a proximal source of emboli; and consistent angiographic findings; (VI) distal extremity ischemia confirmed by noninvasive testing; ultrasound Doppler ultrasound and arteriography were used to confirm the diagnosis (10).
Inclusion and exclusion criteria
Inclusion criteria:
- It conforms to the diagnostic tests of western medicine for TAO, and the clinical stage belongs to Rutherford grade IV (9);
- Standard of TCM syndrome differentiation and blood stasis syndrome;
- Volunteer and sign informed consent.
Exclusion criteria:
- Arteriosclerotic occlusion, diabetic gangrene, Raynaud’s disease, multiple arteritides, acute arterial embolism;
- History of drug allergy, or known drug allergies;
- Patients with severe primary disorders such as cardiovascular and renal hematopoietic system and endocrine system pathologies;
- Acute limb necrosis and infection;
- Chinese and western medicine and other drug testing patients who are using the treatment of the disease within two weeks. Patients enrolled in this study were not simultaneously involved in other patient studies.
Patients grouping
Seventy patients with TAO treated between January 2009 and July 2019 were included in a retrospective analysis of a single university hospital vascular center. Forty patients received topical herbal treatment in addition to conventional therapy and were paired control to a control group who received standard treatment alone (n=30). All patients were Rutherford grade IV at the time of enrolment.
There were 39 males in the treatment group, with a mean age of 45.43±11.49 years. The median duration of treatment was 13.79±4.26 years; There were 28 patients with a history of drinking, nine patients with a history of significant hypothermic exposure (exposed to temperatures less than 0 °C), and 5 cases with patient’s residing in moisture-rich environments.
The control group consisted of 29 male subjects with an average age of 45±12 years and a mean duration of disease symptoms of 12±7 years.
Twenty-two patients had a history of alcohol abuse, five patients with a history of significant hypothermic exposure, and 3 cases with patients residing in moisture-rich environments compared to the experimental group. There was no significant difference in age, gender, course of the disease, and past medical history between the two groups (P>0.05).
There were 39 males in the treatment group, with a mean age of 45.43±11.49 years. The median duration of treatment was 13.79±4.26 years; There were 28 patients with a history of drinking, 9 patients with a history of significant hypothermic exposure (exposed to temperatures less than 0 °C), and 5 cases with patient’s residing in moisture-rich environments.
The control group consisted of 29 male subjects with an average age of 45±12 years and a mean duration of disease symptoms of 12±7 years.
Twenty-two patients had a history of alcohol abuse, 5 patients with a history of significant hypothermic exposure, and 3 cases with patients residing in moisture-rich environments compared to the experimental group. There was no significant difference in age, gender, course of the disease, and past medical history between the two groups (P>0.05).
Drugs
Tuoju lotion (14,15) was prepared by the Pharmacy Department of Dongfang Hospital, which is an affiliated hospital of Beijing University of Chinese Medicine (Beijing, China). The main herbal ingredients included 30 g of Guizhi (Ramulus Cinnamomi), 15 g of Honghua (Flos Carthami), 15 g of Ru Xiang (Olibanum), 15 g of Moyao (Myrrha), 10 g of Chuanjiao (Zanthoxylum bungeanum Maxim), 15 g of Jinyinhua (Flos Lonicerae), 15 g of Sumu (Ligum Sappan), 30 g of Tougucao (Caulis Impatientis), 15g of Jixueteng (Caulis Spatholobi), 15 g of Qiannianjian (Rhizoma Homalomenae), 15 g of Zhangnao (Camphora). Medicinal materials are synthesized by the pharmacy department for the same batch of purchase, according to the unified method decoction. Packing method: 500 mL water, 1 bag, 1 bag each time, 1 time per day, and 14 days for 1 course of treatment. This observation took two courses in total.
Treatment
General treatment
All of the patients were provided with fundamental outpatient health education, which included topics regarding smoking cessation, avoiding mercury rich seafood, avoidance of smoked meat, or meats high in nitrates, safe sexual practices, and the importance of avoiding traumatic injuries. At the same time, the following treatment was given: aspirin (orally, 100 mg/day). Cinepazide Maleate Injection 320 mg/day.
In addition to this medication regimen, the treatment group was given a Tuoju lotion. Medicinal materials are unified by the pharmacy department for the same batch of purchase, according to the unified method decoction. Packing method: 500 mL water, 1 bags, 1 bag each time, 1 times/day. Methods: to determine the proximal part of the lower extremity vascular stenosis or occlusion with peripheral blood tube. Then put the Tuoju lotion into the gauze bag and boil the medicine bag in the water. First, 500 mL of liquid was decocted. When the temperature of the liquid-cooled to approximately 38 degrees centigrade, the affected limb was submerged into the liquid for 20~30 min, 1 time per day, and 14 days for 1 course of treatment. The control group was treated with the same amount of warm water (temperature, method, time, and treatment group) 1 time per day, 14 days for 1 course of treatment, and 2 treatment courses for both groups.
Determination of efficacy criteria: according to the diagnostic efficacy standard of TCM syndrome
After patients were treated for TAO, they were categorically placed according to efficacy criteria:
- Clinical recovery clinical symptoms disappeared; the Ankle-brachial ratio test increased >0.1; Walking speed is 60–80 steps/min, and can walk 1,000 m continuously.
- Markedly: the clinical symptoms were significantly improved. The ankle-brachial ratio assay was developed (ankle-brachial index, ABI) <0.1; The walking speed is 60–80 steps/min, and the walking distance is increased by more than 50%.
- Effective: clinical symptom reduction; ABI improve 0.05; The walking speed was 60~80 steps/min, and the walking distance increased by more than 2.5%.
- Ineffective: after one course of treatment, symptoms and signs did not improve or continue to develop.
Static pain slope and ABI detection
Before and after treatment, two groups of static Pain, slope distance, and ABI pain were measured by TCM symptom score: no pain—0 scores; Occasional Pain—2 scores; Pain is often present, and can tolerate—4 scores; It is hard to bear the substantial daylight—6 scores.
Claudication distance: under the supervision of the doctor, the patient walked at a constant speed in the outpatient corridor. The doctor recorded the distance from the beginning of the walking to the occurrence of the Pain of the affected limb and was forced to stop walking. The claudication distance is more than 1,000 meters, or the chief complaint of intermittent claudication has disappeared, all measured by 1,000 meters. Normal: walking speed of 60–80 steps/min, can continue walking 1,000 M—0 Scores. Light: walking speed of 60–80 steps/min, can continue to walk 500 meters—2 Scores. Moderate: walking speed of 60–80 steps/min, can continue to walk 300 meters—4 Scores. Severe: walking speed of 60–80 steps/min, can continue walking <300 meters—6 Scores.
Automated ABI determination: use PERIPHERAL VASCULAR SYSTEM of PERIPHERAL VASCULAR SYSTEM produced by ATYS MEDICAL company in France.
Blood viscosity
Observed by hemorheology. The patients were treated with venous blood before and after treatment, and the automatic biochemical analyzer was used for testing. Blood viscosity was determined by automated biochemical analyzer SA6900 “Succeeder”®.
Arterial blood pressure in lower extremities
We are using the PERIPHERAL VASCULAR SYSTEM produced by ATYS MEDICAL in France to examine the dorsal artery of the affected limb and the posterior tibial artery, popliteal artery, superficial femoral artery, and femoral artery blood pressure.
Safety observation
One day before treatment and one day after treatment, all patients were examined for general physical examination (respiration, pulse, blood pressure, heart rate). Blood, urine, liver function, and renal function were examined.
Statistical analysis
The counting data is described through (composition ratio). Before and after treatment, ×2 test or non-parametric test was performed. The measurement data is expressed as mean ± standard deviation (SD) values. SPSS v23.0 software (IBM Corp., Armonk, NY, USA) was used for statistical analyses. The data were compared between groups using a one-way analysis of variance (ANOVA), followed by Student’s t-test. Two pairs of comparison were used LSD, Dunnett t-test. P<0.05 was considered statistically significant. Using the procedure of the 80% rule to treat missing data. If a variable had a nonzero measurement value in at least 80% of the variables within one of the two subsets, the variable was included in the data set; otherwise, the variable was removed.
Results
Seventy patients were treated with TAO in the DongFang hospital of Beijing University of Chinese medicine between January 2009 and June 2019. Forty patients received topical herbal treatment in addition to conventional therapy and were paired control to a control group who received standard treatment alone (n=30). All patients were Rutherford grade IV at the time of enrolment.
Seventy patients with a history of TAO were enrolled in our study. The mean age was 45±12 years. There were 68 males and 2 females. One case was from 70 to 79 years old. Nine cases were from 60 to 69 years old. Eleven cases were from 50 to 59 years old. Twenty-two cases were from 40 to 49 years old. Twenty-five cases were from 30 to 39.2 cases was from 20 to 29 years old. The bilateral manifestation of TAO was present in 37 cases, whereas unilateral limb discomfort was present in 33 patients. The duration of clinical symptoms related to TAO ranged from 5 months to 30 years, with an average of 13.65±6.35 years. Twenty-one patients (30%) had a history of migratory superficial phlebitis.
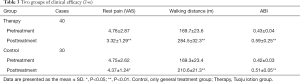
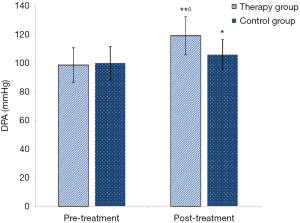
Clinical efficacy of Toujou treatment (Tables 1,2)
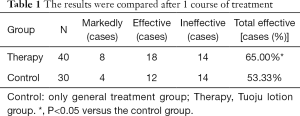
Full table
Full table
Compared with the control group, the total effective rate was higher after one course of treatment and two courses of treatment. The difference was statistically significant (P<0.05).
In 26 patients of the therapy group (65%), clinical results improved after one course of treatment, whereas improvement of clinical symptoms was present in 16 patients (53.3%) of the control group (P<0.05, Table 1).
After two courses of treatment, clinical symptoms improved in 34 patients of the therapy group (85%) and 23 (76.7%) of the control group. The difference was statistically significant (P<0.05, Table 2).
Rest pain, walking distance and ABI (Table 3)
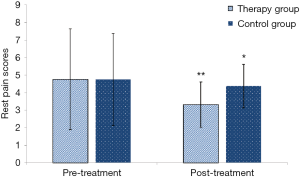
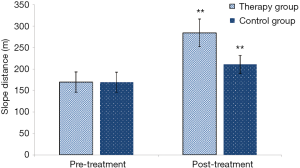
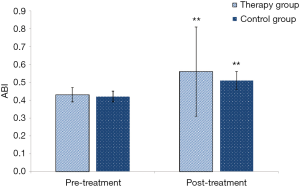
Rest pain score (baseline VAS 4.76±2.87, post-treatment 3.32±1.29, Figure 2) and walking distance (baseline 169.7±23.6 m, post-treatment 284.5±32.3 m, Figure 3) significantly improved in the herbal treatment group (P<0.01, Table 3). In the control group rest patin decreased from VAS 4.75±2.62 pretreatment to 4.37±1.24 (P<0.05) and walking distance improved from 169.3±23.4 to 210±21.3 meter (P<0.01). Ankle brachial index improved in the treatment group from 0.4±0.04 to 0.59±0.25 (P<0.01) and in the control group from 0.42±0.03 to 0.51±0.05 (P<0.01, Figure 4).
Two groups of the Rest pain scores (Figure 2)
In terms of improvement in resting Pain, comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=2.894, P=0.005, **, P<0.01). The control group had no significant differences before and after treatment (t=718, P=0.476, *, P>0.05).
Categorical data of the walking distance (Figure 3)
In terms of improvement in the Slope distance, comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=18.15, P<0.0001, **, P<0.01). The control group had significant differences before and after treatment (t=7.149, P<0.0001, **, P<0.01).
Categorical data of the ABI (Figure 4)
In terms of improvement in the ABI, comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=3.25, P<0.002, **, P<0.01). The control group had significant differences before and after treatment (t=8.46, P<0.0001, **, P<0.05).
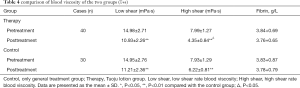
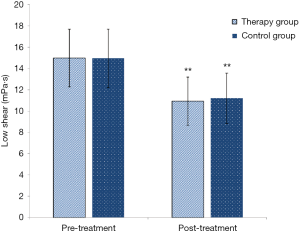
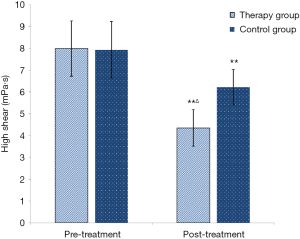
Comparison of blood viscosity in the two groups (Table 4)
Compared with the efficacy before treatment, the total blood viscosity of the two groups was lower than that of the two groups (*, P<0.05, **, P<0.01). Compared with the flat shear rate blood viscosity, the two groups were lower than that of before (Figure 5). In the treatment group, there was a significant change before and after treatment with high shear rate blood viscosity (Figure 6). There was no significant difference in fibrinogen (P>0.05).
Comparison of blood viscosity in Low shear (Figure 5)
In terms of improvement in the low shear, comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=7.26, P<0.0001, **, P<0.01). The control group had significant differences before and after treatment (t=5.64, P<0.0001, **, P<0.01).
Comparison of blood viscosity in High shear (Figure 6)
In terms of improvement in the High shear, comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=15.12, P<0.0001, **, P<0.01). The control group had significant differences before and after treatment (t=6.15, P<0.0001, **, P<0.01).
In terms of improvement in the High shear, the two groups were compared after treatment. There was a significant difference between the therapy group and the control group (t=9.36, P<0.0001, ÄP<0.01).
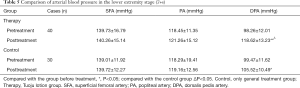
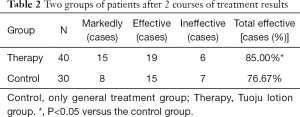
Arterial blood pressure ratio in lower extremity stage (Table 5)
There was no significant difference between the superficial femoral artery and the popliteal artery (P>0.05). There was a significant difference in the treatment of the dorsal artery before and after treatment. Compared with the control group, there was a significant difference between the treatment group (Figure 7) (P<0.05).
Comparison of dorsalis pedis artery blood pressure in the lower extremity stage (Figure 7).
In terms of improvement in the dorsalis pedis artery (DPA), comparisons were made between groups before and after treatment. The therapy group had significant differences before and after treatment (t=7.21, P<0.0001, **, P<0.01). The control group had significant differences before and after treatment (t=2.12, P=0.039, *, P<0.05).
In terms of improvement in the DPA, the two groups were compared after treatment. There was a significant difference between the therapy group and the control group (t=4.47, P<0.0001, ÄP<0.01).
Safety observation
No allergic reactions were observed before and after treatment. There was no significant effect on liver and kidney function before and after treatment.
Discussion
The annual incidence of TAO is reported to be 13 per 100,000 in the United States (12). Although it is observed worldwide, TAO is most prevalent in the Middle East and the Far East. The disease typically presents in patients <45 years of age, with young men being more frequently affected, but TAO can also occur in women (3,16).
Surgical revascularization is usually not feasible in patients with TAO because of the distal and diffuse nature of the disease (16-18). Additional therapeutic options for the treatment of TAO have been limited to vasodilators, intermittent pneumatic compression, spinal cord stimulation, and peripheral periarterial sympathectomy. However, controversy remains regarding the efficacy of these treatment modalities.
The significance of our results is essential for the acceptance of traditional Chinese medical treatment in the treatment of TAO. The results obtained using good experimental designs are well documented. Tuoju lotion was prepared by the Pharmacy Department of Dongfang Hospital, which is an affiliated hospital of Beijing University of Chinese Medicine (Beijing, China). The main herbal ingredients of Tuoju lotion included 30 g of Guizhi (Ramulus Cinnamomi), 15 g of Honghua (Flos Carthami), 15 g of Ru Xiang (Olibanum), 15 g of Moyao (Myrrha), 10 g of Chuanjiao (Zanthoxylum bungeanum Maxim), 15 g of Jinyinhua (Flos Lonicerae), 15 g of Sumu (Ligum Sappan), 30 g of Tougucao (Caulis Impatientis), 15 g of Jixueteng (Caulis Spatholobi), 15 g of Qiannianjian (Rhizoma Homalomenae), 15 g of Zhangnao (Camphora).
Guizhi (Ramulus Cinnamomi) is widely known for its anti-inflammatory effect. Studies report cinnamaldehyde (CM) as a principal active constituent of cinnamon. Furthermore. An antiviral, antineoplastics, and antibacterial effect of CM has been described (19,20). Crocins are mainly derived from traditional Chinese medicine Flos Carthami. It is protective against cardiovascular-related disorders and affects on antiplatelet aggregation (21). Ru Xiang (Olibanum) is the viscous resin of the olivine frankincense. The main active ingredients are triterpenoids, triterpenoids, and triterpenoids. Modern pharmacological studies have shown that it has anti-inflammation, anti-tumor, induced differentiation and apoptosis, anti-ulcer, and other pharmacological activities, with little adverse reactions and potential medicinal value (22). The primary chemical constituents in myrrh are monoterpene, sesquiterpene, triterpene, steroid, and lignin. Pharmacological studies have shown that myrrh has antipyretic, anti-inflammatory, analgesic, neuroprotective, and other pharmacological activities, with no apparent toxic side effects (23). Chuanjiao (Zanthoxylum bungeanum Maxim) a kind of plant resource with high medicinal value, which has many pharmacological functions, such as anesthesia, analgesic, antibacterial, insecticide, antioxidant, and so on. It has good clinical application value (24,25). As a traditional Chinese medicine, Flos Lonicerae is widely used in the clinic. The main active components of Flos Lonicerae are acid, flavonoids, volatile oils, and iridoid compounds. Among them, chlorogenic acid has antibacterial, anti-inflammatory, and anti-oxidation. The flavonoid compound luteolin has the effect of reducing blood lipid and antibacterial, anti-virus, anti-inflammation, and anti-allergy. The volatile component of honeysuckle has the effect of preventing sore throat and anti-oxidation. Cyclic ether terpenoids have antipyretic, anti-inflammatory, and analgesic pharmacological effects (26). Sumu (Ligum Sappan) has antibacterial pharmacological activity. As the research progresses, Sumu also has anti-inflammatory, diastolic blood vessels, immunosuppression, nervous system protection, antioxidants, and other pharmacological effects (27). The anti-inflammatory mechanism of Sumu involved the downregulation of the mRNA expressions of the iNOS, COX-2, and TNF-α genes in a dose-dependent manner. Ligum Sappan is responsible for its anti-inflammatory effect through its ability to inhibit the production of NO, PGE2, and TNF-α. The Ligum Sappan’s test shows no acute toxicity in mice experiments, and it was, therefore, safe to make use of its potent anti-inflammatory and wound healing activities (28). Tougucao (Caulis Impatientis) has anti-inflammatory and analgesic effects. Experiments have demonstrated that Tougucao has analgesic effects on pain models. The acetic acid-induced capillary permeability of the abdominal cavity of mice increases the airway significantly (29). Jixueteng (Caulis Spatholobi) has a variety of pharmacological activities such as blood circulation, pain relief, anti-inflammatory, anti-oxidation, immune regulation, and anti-virus (30). Qiannianjian (Rhizoma Homalomenae) water extract has excellent anti-inflammatory and analgesic effects. At the same time, Qiannianjian extract has excellent antioxidant activity (31). Zhangnao (Camphora) has antiphlogistic, analgesic, antibacterial, promoting, and other pharmacological functions and interacts with other drugs, which is one of the earliest natural organic chemicals used in the world (32).
The treatment observation was only four weeks. Although the symptoms and signs of most patients improved, they did not disappear completely. This study found that the treatment of thrombi occlusive vasculitis could improve or eliminate intermittent claudication, prolong claudication distance, increase ABI (Figure 4), and reduce total blood viscosity (Figures 5,6). In the treatment group, there was a significant change before and after treatment with high shear rate blood viscosity (Figure 6). Compared with the low shear rate blood viscosity, the two groups were lower than that of before (Figure 5). There were significant differences in statistical treatment before and after the treatment of the dorsal pedal artery. The arterial blood pressure ratio in the lower extremity stage showed no difference between the superficial femoral artery and the popliteal artery (Figure 7). It is indicated that the improvement of microcirculation is more evident than the recovery of arterial blood pressure ratio in the lower extremity stage. It is also suggested that the Tuoju lotion can improve the microcirculation status in the short term. The mechanism may be related to reducing the total blood viscosity and improving microcirculation.
Conclusions
In conclusion, the addition of Herbal therapy treatment to conventional treatment in TAO patients with severe extremity pain conferred statistically significant benefits in terms of rest pain control. It also could improve or eliminate intermittent claudication, prolong claudication distance, increase ABI (Figure 4), and reduce total blood viscosity. At the same time, Tuoju lotion can improve microcirculation status in the short term. Multi-centre, prospective, randomized studies with blinded outcome analysis are now needed to elicit more reliable results.
Acknowledgments
Funding: The project of translational application of Beijing University of Chinese medicine (2019-XJ-CGZH-006). The Education Research Science Fund of Beijing University of Chinese Medicine (2019-2021 XJYB1948) (project leader: GL). The work was also supported by the 11th Five-Year Key Specialist Fund of the State Administration of Traditional Chinese Medicine [2015-2020].
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-19-578
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-19-578
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-578). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Regional Ethics Committee of Dongfang Hospital of Beijing University of Chinese Medicine (No. 2010-16). All patients enrolled completed the informed consent form.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stefancik R. Thromboangiitis Obliterans: Changing Demographics for a Preventable Disease. Cureus 2019;11:e3869. [PubMed]
- Brodmann M, Renner W, Stark G, et al. Thrombogenetic risk factors in patients with thrombangitis obliterans. Thromb Res 2000;151:483-3. [Crossref] [PubMed]
- Shima N, Akiyama Y, Yamamoto S, et al. A Non-smoking Woman with Anti-phospholipid Antibodies Proved to Have Thromboangiitis Obliterans. Intern Med 2020;59:439-43. [Crossref] [PubMed]
- Li J, Wang Z. Discussion on the new teaching ideas of traditional Chinese medicine for promoting vascular regeneration in the treatment of peripheral vascular diseases. Chongqing, China, 2019.
- Zhang Z, Ji J, Zhang D, et al. Protective effects and potential mechanism of salvianolic acid B on sodium laurate-induced thromboangiitis obliterans in rats. Phytomedicine 2020;66:153110. [Crossref] [PubMed]
- Gołba M, Sokół-Łętowska A, Kucharska AZ. Health Properties and Composition of Honeysuckle Berry Lonicera caerulea L. An Update on Recent Studies. Molecules 2020;25:749. [Crossref] [PubMed]
- Ge L, Xiao L, Wan H, et al. Chemical constituents from Lonicera japonica flower buds and their anti-hepatoma and anti-HBV activities. Bioorg Chem 2019;92:103198. [Crossref] [PubMed]
- Fakour F, Fazeli B. Visceral bed involvement in thromboangiitis obliterans: a sys-tematic review. Vasc Health Risk Manag 2019;15:317-53. [Crossref] [PubMed]
- Shionoya S. Diagnostic criteria of Buerger's disease. Int J Cardiol 1998;66 Suppl 1:S243-7. [Crossref] [PubMed]
- Olin JW. Thromboangiitis obliterans (Buerger's disease). N Engl J Med 2000;343:864-9. [Crossref] [PubMed]
- Mohamad Yusoff F, Kajikawa M, Takaeko Y, et al. Long-Term Clinical Outcomes of Autologous Bone Marrow Mononuclear Cell Implantation in Patients With Severe Thromboangiitis Obliterans. Circ J 2020;84:650-5. [Crossref] [PubMed]
- Małecki R, Kluz J, Przeździecka-Dołyk J, et al. The Pathogenesis and Diagnosis of Thromboangiitis obliterans: Is It Still a Mystery? Adv Clin Exp Med 2015;24:1085-97. [Crossref] [PubMed]
- Li GZ, Yang BZ, Pang H, et al. Advances in research on the treatment of thromboembolic vasculitis with traditional Chinese and Western medicine. Journal of Vascular and Endovascular Surgery 2019;5:525-30.
- Li GZ, Pang H, Cao JC, et al. Clinical observation on the treatment of thromboangiitis obliterans by oral Mailuotongyu decoction combined with Tuoju lotion. Chinese Journal of Combining Traditional Chinese and Western Medicine 2017;5:119-3.
- Liu Q, Song ZX, Jiang YB. Clinical observation of 32 cases of thromboangiitis obliterated by Tong Yang Huo Xue decoction combined with the treatment of Tuoju lotion. Journal of Mudanjiang Medical College 1992;01:22-3.
- Mousazadeh B, Sharebiani H, Taheri H, et al. Unexpected inflammation in the sympathetic ganglia in thromboangiitis obliterans: more likely sterile or infectious induced inflammation? BioMed Central 2019;17.
- Saito S, Nishikawa K, Obata H, et al. Autologous bone marrow transplantation and hyperbaric oxygen therapy for patients with thromboangiitis obliterans. Angiology 2007;58:429-34. [Crossref] [PubMed]
- Fazeli B, Mirhosseini A, Hashemi Z, et al. Detection of Rickettsia Endosymbiont Bemisia Tabaci in the Amputated Limbs of Three Buerger's Disease Patients. Int Med Case Rep J 2020;13:33-40. [Crossref] [PubMed]
- Liu J, Zhang Q, Li RL, et al. The traditional uses, phytochemistry, pharmacology and toxicology of Cinnamomi ramulus: a review. J Pharm Pharmacol 2020;72:319-42. [Crossref] [PubMed]
- Xu F, Wang DJ, Wang F, et al. Research progress on the pharmacological action of the volatile oil of Gui Zhi. Chinese Journal of Traditional Chinese Medicine 2016;31:4653-4.
- Hatziagapiou K, Kakouri E, Lambrou GI, et al. Crocins: The Active Constituents of Crocus Sativus L. Stigmas, Exert Significant Cytotoxicity on Tumor Cells In Vitro. Curr Cancer Ther Rev 2019. [Crossref]
- Sun Y, Shang QH. Research progress on triterpenoids and pharmacological activities in frankincense. Global Chinese Medicine 2016;9:616-4.
- Sundaram MS, Neog MK, Rasool M, et al. Guggulipid ameliorates adjuvant-induced arthritis and liver oxidative damage by suppressing inflammatory and oxidative stress mediators. Phytomedicine 2019;64:152924. [Crossref] [PubMed]
- Liu X, Xu L, Liu X, et al. Combination of essential oil from Zanthoxylum bungeanum Maxim. And a microemulsion system: Permeation enhancement effect on drugs with different lipophilicity and its mechanism. J Drug Deliv Sci Technol 2020. [Crossref]
- Ma Y, Li X, Hou LX, et al. Extraction solvent affects the antioxidant, antimicrobial, cholinesterase, and HepG2 human hepatocellular carcinoma cell inhibitory activities of Zanthoxylum bungeanum pericarps and the major chemical components. Ind Crops Prod 2019. [Crossref]
- Cui Y, Xu HM. Review on the pharmacological action of honeysuckle. Science and Technology Innovation 2018;02:20-1.
- Das U, Behera SS, Pramanik K. Ethno-Herbal-Medico in Wound Repair: An Incisive Review. Phytother Res 2017;31:579-90. [Crossref] [PubMed]
- Tewtrakul S, Tungcharoen P, Sudsai T, et al. Antiinflammatory and Wound Healing Effects of Caesalpinia sappan L. Phytother Res 2015;29:850-6. [Crossref] [PubMed]
- Tan H. Study on the chemical constituents and pharmacological activities of Chinese traditional Chinese medicine. Chinese Medicine Guide 2015;15:29-1.
- Sun L, Li Q, Guo Y, et al. Extract of Caulis Spatholobi, a novel platelet inhibitor, efficiently suppresses metastasis of colorectal cancer by targeting tumor cell-induced platelet aggregation. Biomed Pharmacother 2020;123:109718. [Crossref] [PubMed]
- Zhao F, Sun C, Ma L, et al. New sesquiterpenes from the rhizomes of homalomena occulta. Fitoterapia 2016;109:113-8. [Crossref] [PubMed]
- Yite X, Jie Q, Pan W, et al. Chemical composition and larvicidal activities of essential oil of Cinnamomum camphora (L.) leaf against Anopheles stephensi. Revista da Sociedade Brasileira de Medicina Tropical 2020.53. [PubMed]