International traditional Chinese medicine guideline for diagnostic and treatment principles of diabetes
Introduction
As one of the major chronic diseases, diabetes has caused great panic of the public. According to the latest data from International Diabetes Federation (IDF), a total of 463 million adults (20–79 years old) worldwide was estimated to have diabetes in 2019, with an incidence rate of 9.3%. Without intervention, the numbers of diabetic patients aged 20–79 years will increase to 700 million in 2045 (1). China is one of the largest developing countries and currently has the largest amount of diabetic patients in the world, about 114.4 million (20–79 years old) people suffer from diabetes (2). Traditional Chinese medicine (TCM) is one of the earliest complementary and alternative medicines worldwide to explore the prevention and treatment of diabetes, and its efficacy has been proven (3,4). A number of clinical studies have been performed, and new herbal products have been developed in order to control the increasing trend of diabetes not only in China but also around the globe (5-9). A case study used a novel approach adopted from cohort studies to analyze the diagnostic process and evaluate the efficacy of TCM treatments for T2DM. The result indicated that after treating with herbal prescriptions based on individual TCM physicians, fasting and post-meal glucose levels, as well as insulin and total triglyceride level of the patients reduced obviously compared to baseline (10). TCM practitioners from different nations have contributed a lot to the management of diabetes, however, no special guideline could be found to offer standard suggestions to them (11,12). Supported by Endocrine Committee of World Federation of Chinese Medicine Societies, this guideline focused on diagnosis and treatment of T2DM with Chinese medicine with the consensus of experts from the fields of endocrinology, methodology and primary care from 13 countries and regions all over the world. Strict quality assessments were conducted according to high-quality TCM systematic review and randomized clinical trials (RCT) in the treatment of diabetes, so as to screen high-level evidences as well as safe and convenient therapeutic methods, which aims to improve the clinical efficacy of TCM treatment on diabetes all over the world.
Diabetes mellitus has been divided into two types, obese and consumptive, known in TCM theory as Pi Dan and Xiao Dan respectively. Obese-type diabetes, Pi Dan, has become the primary condition seen in diabetes clinics, and it can be developed into Consumptive Thirst before ultimately deteriorating further with late-stage complications. Consumptive-type diabetes, Xiao Dan, was seen in patients with type 1 or type 1.5 diabetes and in some with type 2 diabetes. This type manifested as long-term deterioration known as Yin Deficiency Syndrome with Empty Heat in the theory of TCM. Xiao Dan was also gradually developed to the disease of Consumptive Thirst and finally to late-stage complications if not be intervened. In TCM, we concluded that diabetes had four different pathological stages based on clinical symptoms and manifestations, namely stagnation stage, heat stage, deficiency stage and injuring stage. The stagnation, heat, and deficiency stages belonged to the period of diabetes, and the injuring stage belonged to the period of diabetes complications. The stagnation stage represented prediabetes or the early stage of diabetes, such as impaired glucose tolerance (IGT) and impaired fasting glucose (IFG), usually accompanied with insulin resistance. The heat stage represented the attack of diabetes as a result of long-term stagnation and includes symptoms of stomach heat, liver heat, lung heat, intestine heat, etc. The deficiency stage represented the deterioration of diabetes, which was the most common stage seen in the clinic. In TCM, long-term internal heat would result in qi and yin deficiency, and consequently developed into yin and yang deficiency. The TCM pathogenesis in this stage was complex, usually accompanied by heat, sputum, damp or further stasis. The injuring stage represented the end stage of diabetes. This stage was similar to chronic complications of diabetes, and the primary pathogenesis was internal organs deficiency as a result of injured collaterals (microangiopathy) and injured meridians (macroangiopathy). Obstruction of collaterals was observed in the whole process of diabetes, even in the early stage. Thus, the application of herbal medicine to remove blood stasis and promoting circulation of blood vessel as well as collaterals was critical. Sanqi [Panax notoginseng (Burk.) F.H.Chen] and Shuizhi (Hirudo nipponica Whitman) were the most commonly used medicine in the clinic to improve the blood stasis in this situation (13).
Methodology
Guidelines panel composition
For this update, 30 experts were chosen to participate in peer review. Finally, Technical Committee on Standardization of TCM careful revised.
Announcement of interest conflicts and fund sources
International Guideline for Diagnostic and Treatment Principles of Chinese Medicine—Diabetes was made by Endocrine Professional Committee of WFCMS independently, and all of the members declared that there was not any fund sources or interest conflicts.
Evidence evaluation and recommendation principle
The evidence classification principle of this guideline is based on the Composition of Evidence Body of Traditional Medicine and Recommendations for Its Evidence Grading by Prof. Jianping Liu (14). In addition, if a randomized controlled trial is defined as high risk, its grade recommendation is reduced by one level. The process of screening and evaluation of the literature is carried out independently by two evaluators. If the views of the two parties are inconsistent, they would resolve through negotiation or adjudication by a third party (Table 1).

Full table
Because the fact that most of studies on the treatment of diabetes and prediabetes in TCM are not comprehensive, the design of studies is often less standardized, the selection of formula is diverse, and the efficacy standard is not uniform, which attributed to the outcome bias. Therefore, all the evidences of this guideline are required to obtain expert consensus before being included into the recommendation. The recommended grading criteria on the current guidelines are generally recommended for evidence based on the recommended strength level criteria developed by the GRADE (Grading of Recommendations Assessment, Development and Evaluation) team, which is divided into strong and weak levels. When the evidence clearly shows the advantages or disadvantages of the intervention, it can be classified as a high priority by groups of this guideline. When the pros and cons are uncertain in a study or when the quality of the evidence shows the pros and cons are equivalent, it can be considered as a low priority.
In view of the above, this guideline stipulates that if the evidence is level I and obtain expert consensus, then it is considered to be a high priority. If the evidence is level II and obtain expert consensus, it is considered to be a low priority.
Diagnosis
Clinical manifestation
Symptoms
The main clinical manifestations are polydipsia, polyphagia, polyuria and weight loss. Patients can present with tuberculosis, dizziness, chest stuffiness, heart pain, dropsy, stroke, eye disease, carbuncle or other symptoms, such as thirst, irritability and loss of consciousness. Some patients may be asymptomatic.
Signs
Most T2DM patients do not have obvious signs in the early stage. Acute complications such as dehydration can occur when the condition worsens. Prolonged diabetes can cause macrovascular and microvascular complications; peripheral nerve, muscular, bone and joint injuries; and other severe complications.
Physicochemical examination
Criteria for the diagnosis of diabetes (15)
Standards of medical care in diabetes-2019, ADA:
- PG ≥126 mg/dL (7.0 mmol/L). Fasting is defined as no caloric intake for at least 8 h; OR
- 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTT. The test should be performed as described by the WHO, using a glucose load containing the equivalent of 75-g anhydrous glucose dissolved in water; OR
- A1C ≥6.5% (48 mmol/mol). The test should be performed in a laboratory using a method that is NGSP certified and standardized to the DCCT assay; OR
- In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random plasma glucose ≥200 mg/dL (11.1 mmol/L).
Treatment
Basic interventions for diabetes are essential and include a healthy diet, weight control, mental regulation, etc. (16-19). Treatment determination based on syndrome differentiation is a typical characteristic of TCM. Studies reported, for example, Gegen Qinlian Decoction (GQD) reduced HbA1C effectively and it was dose-dependent (High-Dose, Middle Dose, Low Dose and Placebo groups reduced HbA1C by 0.95%, 0.79%, 0.28%, 0.31% respectively) (20). Tianqi capsule reduced the risk of diabetes by 32.1%, and the difference was statistically significant (P<0.05). The result was close to acarbose which reduced the risk by 25% and metformin which reduced the risk by 31% (21). Dachaihu Decoction reduced HbA1C 1.02%, FBG 0.8 mmol/L and 2-h PG 2.70 mmol/L compared with the controlled group, and Dachaihu Decoction was observed that could improve HOMA-β level and lowered body weight, BMI as well as waist circumference (22). The TCM doctor should identify the stage at which the patients initially presented, determine their current syndrome types, and then administer the suggested prescription (Figure 1, TCM diagnosis and treatment of diabetes) (23).
Stagnation stage
In TCM theory, the stagnation stage represents the early stage of diabetes. Most patients with prediabetes are in this stage.
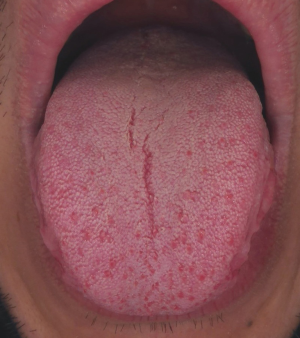
- Observations: obese body type (mainly abdominal obesity) with a fat tongue (Figure 2, Fat tongue of stagnation-stage patients).
- Symptoms: obesity, fatigue, increased appetite and abdominal fullness, frequent belching and flatulence, excessive stool; depressive states with frequent sighing, nervousness, fullness in the chest and flank, catching a cold easily.
- Signs: slippery pulse, tight pulse, pathoglycemia.
Syndrome of accumulation in the spleen and stomach congestion
- Key differentials: abdominal obesity, fat or white tongue with a thick coating.
- Therapeutic method: promoting qi circulation and dredging the accumulation.
- Prescription: modified Houpo Sanwu Decoction (Synopsis of the Golden Chamber) (24). Houpo (Magnolia Officinalis Rehd. et Wils.) 15–25 g, Dahuang (Rheum officinale Baill.) 5–15 g and Zhishi (Aurantii fructus immaturus) 5–15 g are included. (IV, low priority) (The evidence classification principle of this guideline is based on the Composition of Evidence Body of Traditional Medicine and Recommendations for Its Evidence Grading by Prof. Jianping Liu., Table 1).
Syndrome of liver depression and Qi stagnation
- Key differentials: depression, fullness in the chest and flank.
- Therapeutic method: soothing the liver and relieving depression.
- Prescription: modified Xiaoyao Powder (Formulary of the Bureau of Taiping People’s Welfare Pharmacy) (25-28). Chaihu (Bupleurum chinense DC.) 5–15 g, Danggui [Angelica sinensis (Oliv.) Diels] 10–15 g, Baishao (Paeonia lactiflora Pall.) 10–20 g, Baizhu (Atractylodes macrocephala Koidz.) 10–15 g, Fuling [Poria cocos (Schw.) Wolf] 10–20 g, Bohe (Mentha haplocalyx Briq.) 5–15 g and Shengjiang (Zingiber officinale Rosc.) 5–15 g are included. (IV, low priority).
Heat stage
The heat stage is equivalent to the early-to-mid period of diabetes and indicates the attack of disease. Patients with obese-type diabetes mainly suffer from excess heat, while those with lean-type diabetes mainly suffer from deficient heat.
- Observations: red tongue (Figure 3, Red tongue of heat-stage patients), redness on face.
- Symptoms: afraid of heat, dry mouth, increased appetite, yellowish urine, constipation; irritability, bad mood, bitter taste, thirst and yellow thick coating; extreme thirst and excessive sweating; bad breath and excessive appetite; sticky and stinking stool; or dysphoria and heat in chest, and skin condition such as scabies, carbuncle, necrosis, and skin itching.
- Signs: rapid pulse, hyperglycemia.
Tongue appearance in the heat stage.
Syndrome of heat accumulation in stomach and liver
- Differential key: fullness in the chest and flank, irritation, bitter taste, tight pulse.
- Therapeutic method: resolving depression and clearing heat.
- Prescription: modified Da Chaihu Decoction (Treatise on Cold Damage) (22,29). Chaihu (Bupleurum chinense DC.) 10–15 g, Huangqin (Scutellaria baicalensis Georgi) 15–30 g, Banxia [Pinellia ternata (Thunb.) Breit] 10–15 g, Zhishi (Aurantii fructus immaturus) 10–15 g, Baishao (Paeonia lactiflora Pall.) 15–30 g, Dahuang (Rheum officinale Baill.) 3–10 g and Shengjiang (Zingiber officinale Rosc.) 5–15 g are included. (Ib, high priority).
Syndrome of phlegm-heat accumulation
- Key differentials: obesity, yellow and greasy coating, tight and slippery pulse.
- Therapeutic method: clearing heat and eliminating phlegm.
- Prescription: modified Xiao Xian Xiong decoction (Treatise on Cold Damage) (30-32). Huanglian (Coptis chinensis Franch.) 5–30 g, Banxia [Pinellia ternata (Thunb.)Breit] 10–15 g, Gualou (Trichmanthes kiriloxvii Maxim.) 15–30 g and Zhishi (Aurantii fructus immaturus) 5–15 g are included. (Ib, high priority).
Syndrome of intense heat in lung and stomach
- Key differentials: extreme thirsty, excessive sweating, full and forceful pulse.
- Therapeutic method: clearing heat-fire.
- Prescription: modified Baihu Decoction (Treatise on Cold Damage) (33-36) or Sangbaipi Decoction (Medical Complete Books, Ancient and Modern) and Yunu Decoction (Jing Yue’s Collected Works) (37-39). Shigao (Gypsum) 10–45 g, Zhimu (Anemarrhena asphodeloides Bge.) 10–30 g, ShengGancao (Glycyrrhiza uralensis Fisch.) 5–10 g, Sangbaipi (Mori cortex), Huangqin (Scutellaria baicalensis Georgi), Tiandong [Asparagus cochinchinensis (Lour.) Merr.], Maidong [Ophiopogon japonicus (L. f) Ker-Gawl.] 10–20 g and Nan Shashen (Adenophora radix) 5–15 g are included. (IIb, low priority).
Syndrome of excess heat in stomach and small intestine
- Key differentials: sever constipation, bad breath, rapid and forceful pulse.
- Therapeutic method: clearing the excess heat.
- Prescription: modified Dahuang Huanglian Xie Xin Decoction (Treatise on Cold Damage) (40) or modified Xiao Chengqi Decoction (Treatise on Cold Damage) (41). Dahuang (Rheum officinale Baill.) 5–15 g, Huanglian (Coptis chinensis Franch.) 5–30 g, Zhishi (Aurantii fructus immaturus) 5–15 g, Shigao (Gypsum) 5–15 g, Gegen(Puerariae lobatae radix) 15–30 g and Xuanmingfen (Natrii sulfas exsiccatus) 5–20 g are included (42). (IIb, low priority).
Syndrome of intestinal damp-heat
- Key differentials: sticky and stinking stool, rapid and slippery pulse.
- Therapeutic method: clearing heat and promoting diuresis.
- Prescription: modified GQD (Treatise on Cold Damage) (43-45). Gegen (Puerariae lobatae radix) 15–30 g, Huanglian (Coptis chinensis Franch.) 5–30 g, Huangqin (Scutellaria baicalensis Georgi) 15–20 g and stir-frying with liquid adjuvant Gancao (Glycyrrhiza uralensis Fisch.) 5–15 g are included. (Ib, high priority).
Syndrome of intense heat-toxin
- Key differentials: dysphoria and heat in chest, scabies, carbuncle, necrosis, skin itching.
- Therapeutic method: clearing heat and detoxicating.
- Prescription: San Huang Decoction (Supplement to Prescriptions Worth a Thousand Gold Pieces) (46-48) and Wuwei Xiaodu Decoction (Golden Mirror of the Medical Ancestors) (44,49). Huanglian (Coptis chinensis Franch.) 5–10 g, Huangqin (Scutellaria baicalensis Georgi) 5–15 g, Shengdahuang Rheum officinale Baill.) 5–10 g, Jinyinhua (Lonicerae japonicae Flos) 15–30 g, Zihuadiding (Viok yedoensis Makino) 10–30 g, Lianqiao [Forsythia suspensa (Thunb.) Vahl] 10–15 g, Zhizi (Ganiema jasminoides Ellis) 10–15 g and Yuxingcao (Houttuyniae Herba) 10–30 g are included. (IV, low priority).
Deficiency stage
The deficiency stage is equivalent to the middle and end periods of diabetes and indicates disease development. Patients in the deficiency stage comprise the majority of those presenting in the clinic, and their syndromes are always complex with a simultaneous mix of excess and deficient symptoms.
- Observations: red dry tongue (Figure 4, red dry tongue of deficiency-stage patients).
- Symptoms: obvious fatigue, dry mouth, and thirst, excess sweating; frequent urination, polyuria, yellow dry coating; dysphoria in chest, palms and soles; irritation, insomnia and dreaminess, dry stool; emaciation, less and dry coating; gastric stuffiness, nausea and anorexia, watery stool; or bad mood, bitter taste, burning upper abdomen, vomiting, diarrhea and cold limbs.
- Signs: weak pulse, hyperglycemia.
Tongue appearance in the deficiency stage.
Syndrome of heat injuring body fluid
- Observations: extreme thirst, preferring cold drinks, full but weak pulse.
- Therapeutic method: clearing heat, supplementing qi and promoting the production of body fluid.
- Prescription: modified Bai Hu Jia Renshen Decoction (Treatise on Cold Damage) (50,51) or Xiaokefang (Danxi’s Experiential Therapy) (52,53). Shigao (Gypsum) 15–50 g, Zhimu (Anemarrhena asphodeloides Bge.) 10–15 g, Taizishen (Pseudostellariae radix) 20–30 g, Tianhuafen (Trichosanthis radix) 20–30 g, Shengdihuang (Rehmannia glutinosa Libosch.) 10–20 g, Huanglian (Coptis chinensis Franch.) 5–10 g, Gegen (Puerariae lobatae radix) 15–20 g, Maidong [Ophiopogon japonicus (L. f)Ker-Gawl.] 10–15 g and Ouzhi 5–15 g are included. (IIb, high priority).
Syndrome of yin deficiency and fire intense
- Observations: dysphoria in chest, palms and soles; rapid but thin pulse.
- Therapeutic method: nourishing yin and decreasing fire.
- Prescription: Modified Zhibai Dihuang Pill (Jing Yue’s Collected Works) (54,55). Zhimu (Anemarrhena asphodeloides Bge.) 10–20 g, Huangbai (Phellodendri chinensis cortex) 10–20 g, Sheng Dihuang (Rehmannia glutinosa Libosch.) 20–30 g, Shanyurou (Cornus officinalis Sieb.et Zucc.) 10–15 g, Shanyao (Dioscoreae rhizoma) 10–15 g and Mudanpi (Moutan cortex) 10–15 g are included. (IV, low priority).
Syndrome of qi-yin deficiency
- Observations: emaciation, red tongue with dry and less coating, rapid but weak pulse.
- Therapeutic method: supplementing qi, nourishing yin and clearing heat.
- Prescription: modified Sheng Mai Powder (Revelation of Medicine) (56-59) and Zengye Decoction (Detailed Analysis of Warm Diseases) (60-62). Renshen (Panax ginseng C. A. Mey.) 5–20 g, Shengdihuang (Rehmannia glutinosa Libosch.) 10–20 g, Wuweizi [Schisandra chinensis (Turcz.) Baill.] 5–15 g, Maidong [Ophiopogon japonicus (L. f)Ker-Gawl.] 5–15 g and Xuanshen (Scrophularia ningpoensis Hemsl.) 10–15 g are included. (IIb, low priority).
Syndrome of spleen insufficiency and stomach stagnation
- Observations: gastric stuffiness, anorexia, sublingual varices, tight slippery but weak pulse.
- Therapeutic method: acrid opening and bitter downbearing.
- Prescription: modified Banxia Xie Xin Decoction (Treatise on Cold Damage) (63-65) (IIb low priority) or modified Ganjiang Huangqin Huanglian Renshen Decoction (Treatise on Cold Damage) (66-69). Ganjiang (Zingiberis rhizoma) 5–10 g, Huangqin (Scutellaria baicalensis Georgi) 5–30 g, Huanglian (Coptis chinensis Franch.) 5–30 g and Renshen (Panax ginseng C. A. Mey.) 5–30 g are included. (IIIa, low priority).
Syndrome of upper heat and lower cold
- Observations: bad mood, bitter taste, cold lower limbs, thick and greasy coating on the tongue base.
- Therapeutic method: clearing upper and warming lower.
- Prescription: modified Wumei Pill (Treatise on Cold Damage) (70-72). Wumei (Smoked Plum) 15–30 g, Huanglian (Coptis chinensis Franch.) 5–10g, Huangbai (Phellodendri chinensis cortex) 10–15 g, Ganjiang (Zingiberis rhizoma) 5–10 g, Shujiao (Prickly Ash Peel) 5–10 g, Fuzi (Aconiti lateralis radix praeparata) 3–10 g, Danggui [Angelica sinensis (Oliv.) Diels] 10–15 g, Rougui (Cinnamomum cassia Presl) 3–10 g and Dangshen [Codonopsis pilosula (Franch.) Nannf.] 10–15 g are included. (IIb, low priority).
Injuring stage
Both obese and nonobese type 2 diabetes can lead to liver-kidney yin deficiency or yin-yang deficiency. There are a variety of chronic complications. Severe patients can even die. The injuring stage indicates the end-stage of diabetes or the period of diabetes complications. The main pathological changes in this stage include microvascular and macrovascular lesions, which gradually induce organ damage.
- Observations: pale tongue, sublingual varices (Figure 5).
- Symptoms: all the symptoms that patients with diabetes complications will manifest, including frequent and turbid urine, blurred vision, dizziness, tinnitus, dreaminess, seminal emission, dry skin, night blindness, muscae volitantes and even blindness, itching skin; dry mouth and throat, fatigue, dry ear, darkish complexion, soreness and weakness of waist and knees, erectile disorder, edema and even anasarca of lower limbs; or fear of cold, cold limbs, frequent and long urination, dysuria, watery stool, edema.
- Signs: sinking and thin pulse, hyperglycemia.
Tongue appearance in the injuring stage.
Syndrome of liver-kidney yin deficiency
- Key differentials: blurred version; soreness and weakness of waist and knees; dysphoria in chest, palms and soles; dreaminess; seminal emission; rapid and thin pulse.
- Therapeutic method: nourishing liver and kidney.
- Prescription: modified Qiju Dihuang Pill (Precious Mirror for Advancement of Medicine) (73). Gouqizi (Lycium barbarum L.) 10–15 g, Juhua (Chrysanthemi flos) 10–15 g, Shudi (Rehmanniae radix praeparata) 10–30 g, Shanyurou (Cornus officinalis Sieb.et Zucc.) 10–15 g, Shanyao (Dioscoreae rhizoma) 10–30 g, Fuling [Poria cocos (Schw.) Wolf] 10–30 g, Mudanpi (Moutan cortex) 10–15 g, Zexie [Alisma orientale (Sam) Juzep.] 10–15 g, Nuzhenzi (Ligustri lucidi fructus) 10–15 g and Mohanlian (Ecliptae herba) 10–15 g are included. (IIa, low priority).
Syndrome of yin-yang deficiency
- Key differentials: frequent urination; dysphoria in chest, palms and soles; darkish complexion; cold limbs.
- Therapeutic method: nourishing yin and tonifying yang.
- Prescription: modified Jingui Shenqi Pill (Synopsis of the Golden Chamber) (74-78). Zhifuzi (Aconiti lateralis radix praeparata) 5–10 g, Guizhi (Cinnamomi ramulus) 3–10 g, Shudi (Rehmanniae radix praeparata) 10–30 g, Shanyurou (Cornus officinalis Sieb.et Zucc.) 15–20 g, Shanyao (Dioscoreae rhizoma) 15–20 g, Zexie [Alisma orientale (Sam) Juzep.] 10–15 g, Fuling [Poria cocos (Schw.) Wolf] 10–15 g and Danpi (Moutan cortex) 10–15 g are included. (Ib, high priority).
Syndrome of spleen-kidney yang deficiency
- Key differentials: frequent urination at night, fear of cold, cold limbs, watery stool, edema, fat and pale tongue.
- Therapeutic method: tonifying the spleen and kidney.
- Prescription: modified Fuzi Lizhong Pill (Treatise on Cold Damage) (79). Zhifuzi (Aconiti lateralis radix praeparata) 15–20 g, Ganjiang (Zingiberis rhizoma) 10–15g, Renshen (Panax ginseng C. A. Mey.) 10–15 g, Chaobaizhu (Atractylodes macrocephala Koidz.) 15–20 g and Zhigancao (Glycyrrhizae radix et rhizome praepapata cum melle) 10–15 g are included. (IIIb, low priority).
Concurrent syndrome
In addition to the above syndromes, phlegm, damp, turbidity and stasis are common concurrent syndromes. Concurrent phlegm syndrome always appears in obese diabetic patients. concurrent damp syndrome always appears in patients with diabetic gastrointestinal lesions, concurrent turbidity syndrome always appears in patients with hyperlipidemia or hyperuricemia, and concurrent stasis syndrome always appears in patients with diabetic vascular disease.
Concurrent phlegm syndrome
- Therapeutic method: activating qi and eliminating phlegm.
- Prescription: modified Erchen Decoction (Formulary of the Bureau of Taiping People’s Welfare Pharmacy) (80-82). Banxia (Pinellia ternata) 10–15 g, Chenpi (Citri reticulatae pericarpium) 5–15 g, Fuling (Poria cocos) 10–20 g, Zhigancao (Glycyrrhizae radix et rhizome praepapata cum) 3–10 g, Shengjiang (Zingiber officinale Rosc.) 5–15 g and Dazao (Jujubae fructus) 5–15 g are included. (IIIb, low priority).
Concurrent damp syndrome
- Therapeutic method: drying damp and strengthening spleen.
- Prescription: modified Pingwei Powder (Formulary of the Bureau of Taiping People’s Welfare Pharmacy) (83). Cangzhu (Atractylodes Rhizoma) 5–15 g, Houpo (Magnolia Officinalis Rehd. et Wils.) 5–10 g, Chenpi (Citri reticulatae pericarpium) 5–15 g, Gancao (Glycyrrhiza uralensis Fisch.) 3–10 g and Fuling [Poria cocos (Schw.)Wolf] 5–20 g are included. (IIb, low priority).
Concurrent turgidity syndrome
- Therapeutic method: clearing turbidity.
- Prescription: modified Xiaogao Jiangzhuo Decoction. Hongqu (Red yeast rice), Wuguchong (Oriental Latrine Fly Larvina), Shengshanzha (Crataegus pinnatifida Bgc.), Xihonghua (Saffron) and Weilingxian (Clematis chinensis Osbeck) are included. (IV, low priority).
Concurrent stasis syndrome
- Therapeutic method: invigorate blood circulation.
- Prescription: modified Taohong Siwu Decoction (Golden Mirror of the Medical Ancestors) (84,85). Modified Didang Decoction (Treatise on Cold Damage) (86,87) is a choice for patients with retinopathy or kidney vein lesions. Taoren (Persicae semen) 5–15 g, Honghua (Saffron) 5–15 g, Chuanxiong (Ligusticum chuanxiong Hort.) 5–15 g, Danggui [Angelica sinensis (Oliv.) Diels] 5–15 g, Shengdihuang (Rehmannia glutinosa Libosch.) 15–30 g, Baishao (Paeonia lactiflora Pall.) 5–15 g, Jiu Dahuang (Rheum officinale Baill.) 5–15 g and Shuizhi 5–10 g (Hirudo nipponica Whitman) are included. (IIb, low priority).
Discussion
Guideline establishment process
TCM clinical practice guidelines play essential roles in the development of TCM. International Guideline for Diagnostic and Treatment Principles of Chinese Medicine in Diabetes was approved by International Standard Department of World Federation of Chinese Medicine Societies (WFCMS-SCM/NP 2017-0022). The standard was supported by Endocrine Committee of World Federation of Chinese Medicine Societies. The process is as follows: the draft of this guideline was initiated by WFCMS, and was drafted according to the standardization of ISO, which followed standard principles by WFCMS. Many domestic and foreign committees have cooperated to accomplish the first draft, which adopted to the principle of “evidences, consensus and clinical practice combined”. Then 50 TCM diabetes experts across the country participated in the discussion and revise of the draft, and another 30 experts participated in peer review and all gave agreement on the draft, and 9 of them proposed revising suggestions in March 2017. After revising according to the peer review, the draft was published online by WFCMS. The draft was approved by Technical Committee on Standardization of TCM in Beijing on Sept. 7, 2017 and was finalized in Oct. 2017 after careful revising. The guideline allows for standardize and improve the therapies and treatment of diabetes in TCM, which has a significance in the clinical practice of TCM.
Summary of the evidence and explanation of the results
Management of T2DM is still a challenge. Standard therapy for T2DM includes diet and exercise, use of oral hypoglycemic medication, and/or insulin injections. Although a lot of progress has been made to indicate hypoglycemic drugs and insulin are effective and safety, Western medicine still has some limitations. Currently, TCM are popular in both developing and developed countries. Due to positive views of patients regarding TCM therapies, they are frequently used for T2DM globally, especially in China. Although TCM formula varied in their herbal components, they form part of a “group” of herbal medicines with anti-hyperglycemic effects. TCM formula contains multiple active ingredients, which could provide multiple therapeutic efficacy on multiple targets, such as improvement of insulin sensitivity, stimulation of insulin secretion, or reduction of carbohydrate absorption. Additionally, TCM help make holistic regulation of metabolic problems by single formula, as patients with metabolic syndrome often suffer from complex and combined medication. TCM also have the advantages of reversing the risk factors leading to T2DM and delaying diabetic complications.
In the Stagnation stage, the high-quality evidence was unavailable. Based on the clinical experience, the classical formula modified Houpo Sanwu Decoction derived from Synopsis of the Golden Chamber was recommended for spleen and stomach congestion syndrome. Currently, there are no data available to address the effectiveness of modified Houpo Sanwu Decoction. One observational study found that modified Xiaoyao Powder combined with conventional anti-hypoglycemic therapies was more effective than anti-hypoglycemic therapies alone. This study concluded that Xiaoyao Powder could sooth the liver to relieve depression, which is effective in treating liver depression and qi stagnation syndrome of T2DM and could improve the symptoms related to T2DM (25).
In the Heat stage, one RCT (22), performed at 10 hospitals in China, included 480 overweight type 2 early-stage diabetic patients with Heat Accumulation in Stomach and Liver Syndrome. Modified Da Chaihu Decoction decreased HbA1c by 1.02% from the before treatment, and effectively controlled fasting plasma glucose (FPG), 2-hour postprandial blood glucose (2hPG), body weight, BMI and weight circumference. The study also indicated that modified Da Chaihu Decoction was safe to use. In the animal experiment, Baihu decoction significantly improved glycemic control, which may be related to improvement of inflammation (33). No randomized trials have been conducted to evaluate the effectiveness of modified Dahuang Huanglian Xie Xin Decoction (DHXD) in the treatment of T2DM. A retrospective study reported data for 183 patients with T2DM, DHXD led to a significant reduction in blood glucose, blood lipids and body weight, and improve symptoms of excess heat in stomach and small intestine syndrome (42). Two RCTs of modified GQD were included. In the 12-week, multi-centers randomized, double-blinded, placebo-controlled clinical trial, the efficacy of GQD for type 2 diabetes mellitus (T2DM) intestinal damp-heat syndrome was evaluated. A total of 187 T2DM patients were randomly allocated to receive high, moderate, low dose GQD or the placebo. The results demonstrated that GQD significantly improved glycemic control and HOMA-β in T2DM patients, the mechanism of action is related to the abundance of beneficial bacteria (19). Another RCT also demonstrated that GQD was effective in decreasing the level of fasting blood-glucose (FBG), postprandial blood sugar (PBG) and hemoglobin A1c (HbAlc) (88).
In the Deficiency stage, one case-control studies found that modified Bai Hu Jia Renshen Decoction may enhance the hypoglycemic action as an add-on medication to metformin monotherapy (89). A systematic review and meta-analysis reviewed the evidence for Sheng Mai Powder to treat T2DM with qi-yin deficiency syndrome. It included 4 RCTs, with 336 patients, who received Sheng Mai Powder vs. blank. Results suggested that compared with blank, Sheng Mai Powder was better on reducing the blood glucose. However, the methodological quality of the randomized controlled trials was generally low (90).
In the Deficiency stage, a systematic review and meta-analysis published in 2009 reviewed the evidence for Qiju Dihuang Pill (QDP) to treat T2DM. It included 5 RCTs, with 259 patients with T2DM, who received QDP or conventional Western drugs. Results indicated that QDP may improve the symptoms related to T2DM, and be efficacious for treating T2DM (91). A systematic review and meta-analysis assessed the effects of Shenqi Pill on T2DM with yin-yang deficiency syndrome. It included 7 RCTs (910 patients) that compared Shenqi Pill plus anti-hyperglycemic agent with anti-hyperglycemic agent alone. Results indicated that compared with controls, Shenqi Pill was better on the improvement of FBG, PBG and hemoglobin A1c. The evidence currently available showed that Shenqi Pill may have preliminary effect as an add-on medication to anti-hyperglycemic agent monotherapy, further large-scale trials are required to confirm the role of Shenqi Pill in the treatment of T2DM (92).
Research limitations
The guideline also had some unavoidable limitations. Firstly, the evidence level recommended in this TCM clinical practice guideline for T2DM was generally low, because high quality evidences, such as systematic review and RCTs, were not available. Considering this situation, the recommendation of TCM clinical evidences has its specific system rather than using GRADE, which has been mentioned above. Secondly, Different schools of TCM existed, because of different understandings of classics of TCM, different ideas of diagnosis and treatment of diseases. When confronted with the same disease, different schools of TCM had different therapeutic methods, which led that the recommendation could not be widely adopted and used in clinical practice. Thirdly, the lack of methodological rules in TCM clinical practice guidelines leads to a series of methodological quality problems.
Acknowledgments
Special thanks to Tawat Buranatawonsom (Thailand); Wensheng Chen (Philippines); Liu Dong (Canada); Huilan Du, Guanjie Fan, Zhihai Feng, Ying Gao, Huailin Gao, Sihua Gao, Tianshu Gao, Xiumei Gao, Xin Gao, Yanbin Gao, Jiao Guo, Yi Guo, Dongpeng Hu, Yongsheng Huang, Zhongqin Huang, Liangduo Jiang, Qingliang Jiang, Hui Li, Huilin Li, Jing Li, Min Li, and Ming Li (Mauritius); Ping Li, Shuanglei Li, Zegeng Li, Zhen Li, Zhenji Li, Chao Liu, Jianping Liu, Tonghua Liu, and Weiying Liu (Singapore); Chuanjian Lu, Zheng Nan, Guoming Pang, Qiuhai Qian, and Jiangang Shen (Hong Kong, China); Jun Song, Ping Song, and Brenda Bin Su (Canada); Xudong Tang, Chengde Wang, Gang Wang, Hongcai Wang, and Ning Wang (Grand Duchy of Luxembourg); Shouchuan Wang, Wencheng Wang, Xiu’e Wang, Xu Wang, and Chongkai Wen (Taiwan, China); and Shentao Wu, Nan Xiang, Chunguang Xie, Yanming Xie, Boshou Xue, Shijia Yu, Jiangyi Yu, Rensong Yue, Dinghua Zhang, Huiqin Zhang, Jiajun Zhao, Jinxi Zhao, Zhonghua Zheng, and Zhengzhe Zhong (Canada) for their technical assistance with these guidelines. Professor Xiaolin Tong is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-271). The authors have no conflicts of interest to declare.
Ethics Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This research was approved by the ethics committee of Guang’anmen Hospital, China Academy of Chinese Medical Sciences.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 2019;157:107843. [Crossref] [PubMed]
- Wang L, Gao P, Zhang M, et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. JAMA 2017;317:2515. [Crossref] [PubMed]
- Tong X, Dong L, Chen L, et al. Treatment of diabetes using traditional Chinese medicine: past, present and future. Am J Chin Med 2012;40:877-86. [Crossref] [PubMed]
- Liu JP, Zhang M, Wang WY, et al. Chinese herbal medicines for type 2 diabetes mellitus. Cochrane Database Syst Rev 2004;(3):CD003642. [PubMed]
- Lian F, Li G, Chen X, et al. Chinese Herbal Medicine Tianqi Reduces Progression From Impaired Glucose Tolerance to Diabetes: A Double-Blind, Randomized, Placebo-Controlled, Multicenter Trial. J Clin Endocrinol Metab 2014;99:648-55. [Crossref] [PubMed]
- Lian F, Tian J, Chen X, et al. The Efficacy and Safety of Chinese Herbal Medicine Jinlida as Add-On Medication in Type 2 Diabetes Patients Ineffectively Managed by Metformin Monotherapy: A Double-Blind, Randomized, Placebo- Controlled, Multicenter Trial. PLoS One 2015;10:e0130550. [Crossref] [PubMed]
- Cao H, Ren M, Guo L, et al. JinQi-Jiangtang tablet, a Chinese patent medicine, for pre-diabetes: a randomized controlled trial. Trials 2010;11:27.
- Pang B, Zhang Y, Liu J, et al. Prevention of Type 2 Diabetes with the Chinese Herbal Medicine Tianqi Capsule: A Systematic Review and Meta- Analysis. Diabetes Ther 2017;8:1227-42. [Crossref] [PubMed]
- Ji L, Tong X, Wang H, et al. Efficacy and Safety of Traditional Chinese Medicine for Diabetes: A Double-Blind, Randomised, Controlled Trial. PLoS One 2013;8:e56703. [Crossref] [PubMed]
- Gu X, Huang N, Gu J, et al. Employing observational method for prospective data collection: A case study for analyzing diagnostic process and evaluating efficacy of TCM treatments for diabetes mellitus. J Ethnopharmacol 2016;192:516-23. [Crossref] [PubMed]
- Yang W, Weng J. Early therapy for type 2 diabetes in China. Lancet Diabetes Endocrinol 2014;2:992-1002. [Crossref] [PubMed]
- Maddaloni E, Pozzilli P. Why China guidelines for type 2 diabetes represent an opportunity for treating this disease. Diabetes Metab Res Rev 2016;32:438-9. [PubMed]
- Diabetes Branch Committee of China Association of Chinese Medicine. China Guideline For Type 2 Diabetes (2017 Edition). Chin J Diabetes Mellitus 2017;10:4-67.
- Liu J. The composition of evidence body of traditional medicine and recommendations for its evidence grading. Chin J Integr Tradit West Med 2008;27:1061-5. [PubMed]
- American Diabetes Association. Standards of Medical Care in Diabetes-2019. Diabetes Care 2019;42:S1-194. [Crossref] [PubMed]
- Khazrai Y, Defeudis G, Pozzilli P. Effect of diet on type 2 diabetes mellitus: a review. Diabetes Metab Res Rev 2014;30:24-33. [PubMed]
- Aune D, Norat T, Leitzmann M, et al. Physical activity and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Epidemiol 2015;30:529-42. [Crossref] [PubMed]
- Delahanty L, Pan Q, Jablonski K, et al. Effects of weight loss, weight cycling, and weight loss maintenance on diabetes incidence and change in cardiometabolic traits in the Diabetes Prevention Program. Diabetes Care 2014;37:2738-45. [Crossref] [PubMed]
- Endocrinology L. Poor mental health in diabetes: still a neglected comorbidity. Lancet Diabetes Endocrinol 2015;3:393. [Crossref] [PubMed]
- Xu J, Lian F, Zhao L, et al. Structural modulation of gut microbiota during alleviation of type 2 diabetes with a Chinese herbal formula. ISME J 2015;9:552-62. [Crossref] [PubMed]
- Lian F, Tong X, et al. Chinese herbal medicine Tianqi reduces progression from impaired glucose tolerance to diabetes: a double-blind, randomized, placebo-controlled, multicenter trial. J Clin Endocrinol Metab 2014;99:648-55. [Crossref] [PubMed]
- Tong X, Wu S, Lian F, et al. The safety and effectiveness of TM81, a Chinese herbal medicine, in the treatment of type 2 diabetes: a randomized double-blind placebo-controlled trial. Diabetes Obes Metab 2013;15:448-54. [Crossref] [PubMed]
- Guo J, Chen H, Song J, et al. Syndrome Differentiation of Diabetes by the Traditional Chinese Medicine according to Evidence-Based Medicine and Expert Consensus Opinion. ECAM 2014;2014:492193. [PubMed]
- Yu C, Hongmei H, Qiyou W, et al. Influence of Hypoglycemic Effect and Inflammatory State for Treating Spleen and Stomach Stagnation Syndrome Diabetes Patients with Houpo Sanwu Decoction. Journal of Liaoning University of Traditional Chinese Medicine 2016;18:164-6.
- Ni H, Liu G, Luo S. Clinical study in treating type 2 diabetes mellitus according to liver in TCM. Zhongguo Zhong Xi Yi Jie He Za Zhi 2000;20:577-9. [PubMed]
- Feng S, Xiuzhen T. Clinical Effect of Xiaoyao Powder Combined with Maiwei Dihuang Decoction on Treating Diabetes of Yin Deficiency and Qi Stagnation. Journal of Liaoning University of Traditional Chinese Medicine 2016;18:156-8.
- Qiwei D. Clinical observation of Xiaoyao San on the treatment of type 2 diabetes mellitus. Hubei Journal of Traditional Chinese Medicine 2003;25:31.
- Yuling W, Jialan T. Treatment of 51 Cases of Diabetes with Xiaoyao Powder. Jilin Journal of Chinese Medicine 2003;23:20.
- Hongyan C, Yanling C. Clinical observation of Dachaihu Decoction in the treatment of type 2 diabetes mellitus. Hebei Journal of Traditional Chinese Medicine 2015;37:1195-7.
- Hairong Z. Clinical observation and cost analysis of Xiaozhanxiong Decoction in the treatment of type 2 diabetes mellitus with hot and cold type. Hebei Journal of Traditional Chinese Medicine 2015;37:1369-71.
- Shijie L. Minor Chest-Draining Decoction for Treating 57 Cases with Type-2 Diabetes of Intermingling of Phlegm and Heat. Henan Traditional Chinese Medicine 2015;35:1493-5.
- Limin Z, Yi T, Wei H, et al. Clinical observation of Xiaozhanxiong Decoction combined with metformin in the treating phlegm-heat type 2 diabetic patients. Chinese Journal of Information on Traditional Chinese Medicine 2014;21:32-4.
- Fang Y, Chen H. The effect of Baihu Decoction on blood glucose levels in treating systemic inflammatory response syndrome. Chin J Integr Med 2010;16:472-9. [Crossref] [PubMed]
- Qing S, Yilin M. Clinical observation of 55 cases of type 2 diabetes treated with Jiawei Baihu Decoction. J New Chin Med 2007;39:75-6.
- Wenguang C, Linhe W. Treatment of 30 Cases of Type 2 Diabetes with Jiawei Baihu Decoction. Fujian Journal of Traditional Chinese Medicine 2006;37:40.
- Qing L, Zongliang S. Clinical observation of 30 cases of type 2 diabetes mellitus treated with Zhibai Dihuang Decoction and Baihu Decoction. Hunan Journal of Traditional Chinese Medicine 2018;34:64-5.
- Hongmei C, Tengteng H, Kai C. Clinical observation on 60 cases with stomach-heat type diabetes IItreated with modified Yunv decoction. Clinical Journal of Chinese Medicine 2014;6:50-1.
- Xiaoliang S. Clinical experience of Yufu Jianliu Liuwei Dihuang Decoction in the treatment of diabetes mellitus. Nei Mongol Journal of Traditional Chinese Medicine 2014;33:9-10.
- Ming Z. Clinical study on treatment of type 2 diabetes with Yufujian plus reduction prescription. Journal of Zhejiang Chinese Medical University 2010;34:67.
- Zhiqiang Z, Chengqiang L. Observation on the therapeutic effect of rhubarb Huanglian Xiexin Decoction combined with Western medicine in the treatment of type 2 diabetes mellitus (heat syndrome). Guiding Journal of Traditional Chinese Medicine and Pharmacy 2016;22:104-6.
- Na L, Yu C. Observation on the efficacy of Jiawei Xiaochengqi Decoction in the treatment of diabetic real heat constipation. Shanxi Journal of Traditional Chinese Medicine 2016;32:15-6.
- Pang B, Guo J, Zhao L, et al. Retrospective study of Traditional Chinese Medicine treatment of type 2 diabetes mellitus. J Tradit Chin Med 2016;36:307-13. [Crossref] [PubMed]
- Ying L. Clinical observation of Gegen Qinlian Decoction combined with metformin in the treatment of type 2 diabetes mellitus with damp-heat type. Journal of Guangxi University of Chinese Medicine 2017;20:28-9.
- Li L, Chang Y. Effect of Wuwei Xiaodu Decoction on Immune Function of Patients with Diabetic Foot. Chin J Integr Med on Cardio Cerebrovascular Disease 2012;10:508-9.
- Shaolin P, Dongcai W, Wenzhao Z, et al. Observation on the efficacy of Baihu plus ginseng decoction in the treatment of type 2 diabetes mellitus with qi and yin deficiency and dry heat. J New Chin Med 2015;47:84-6.
- Zhu Z, Xiong M, Lin A. Effect of sanhuang jiangtang recipe on insulin peripheral resistance in type II diabetics. Zhongguo Zhong Xi Yi Jie He Za Zhi 1997;17:590-3. [PubMed]
- Lifang Y, Xu W, Wenbin S, et al. Effect of Sanhuang Tang on Insulin Resistance Index and Inflammatory Factors of Obese Type-2 Diabetes. Chin J Exper Tradit Med Formulae 2013;19:289-92.
- Dayong H, Zhiyou G. Summary of 33 Cases of Early Type II Diabetes Treated with Dachaihu Decoction and Sanhuang Decoction. Cuiding J Tradit Chin Med Phar 2008;14:68-9.
- Fengxia L. Observation on the Curative Effect of Modified Wuwei Xiaodu Decoction Combined with Insulin in the Treatment of Diabetic Skin Ulcer. Modern J Integr Tradit Chin Western Med 2012;21:3345-6.
- Shaolin P, Dongcai W, et al. Observation on the efficacy of Baihu plus ginseng decoction in the treatment of type 2 diabetes mellitus with qi and yin deficiency and dry heat. Journal of New Chinese Medicine 2015;47:84-6.
- Yi T, Chunguang X. Clinical observation of Baihu plus ginseng decoction in the treatment of type 2 diabetes mellitus. Journal of Chengdu University of Traditional Chinese Medicine 2002;25:23-4.
- Zhengqin X, Lin D. Clinical observation of Jiawei Xiaoke Decoction in the treatment of newly diagnosed type 2 diabetes mellitus. Diabetes New World 2017;20:93-4.
- Xiuxia L. Treatment of 82 Cases of Type 2 Diabetes with Xiaoke Fangjia Decoction. Guide of China Medicine 2010;8:60-1.
- Jibin Z, Changer C, Chunyuan C, et al. Effect of Zhibai Dihuang Decoction on Yin-deficiency and Fire-excess in Patients with Type 2 Diabetes Mellitus HOMA-IR. Journal of Yunnan University of Traditional Chinese Medicine 2016;39:70-2.
- Songtao C. Clinical Observation on 62 Cases of Type 2 Diabetes Mellitus Treated by Zhibai Dihuang Decoction and Modified Decoction. Forum on Traditional Chinese Medicine 2013;28:36.
- Ning L, Jie Y, Jun W. Clinical study on 42 cases of newly diagnosed type 2 diabetes mellitus treated with Jiawei Shengmai Powder. Asia-Pacific Traditional Medicine 2015;11:121-2.
- Min L. Clinical observation of Jiawei Shengmai Powder in the treatment of insulin resistance in type 2 diabetes. J North Phar 2015;12:25.
- Youli L. Therapeutic effect of Shengmaisan on the treatment of type 2 diabetes mellitus with deficiency of Qi and Yin. Guide of China Medicine 2012;10:292-3.
- Xiaochen T. Treatment of 60 Cases of Type 2 Diabetes with Jiawei Shengmai Powder. Henan Traditional Chinese Medicine 2007;27:52-3.
- Fu H, Xiuge W, Yang B. Efficacy Analysis Type 2 Diabetes Treated by Baihu Renshen Decoction and zengye Decoction for 79 cases. Chinese Medicine Modern Distance Education of China 2014;12:15-6.
- Zhenghua L. Observation on the therapeutic effect of Baihu ginseng Tanghe Zengjing Decoction on type 2 diabetes mellitus. Hubei Journal of Traditional Chinese Medicine 2013;35:45-6.
- Wei H, Jie Y. Effect of Jiawei Zengye Decoction on Insulin Resistance in Type 2 Diabetes. Chinese Archives of Traditional Chinese Medicine 2003;21:234-5.
- Weiyue S, Aiming Z, Lvya L. Observation on 40 Cases of Type 2 Diabetes Mellitus Treated by Modified Banxia Xiexin Decoction. Zhejiang Journal of Traditional Chinese Medicine 2014;49:813.
- Xiuling Z, Guojun Z, Wenzhao S, et al. Observation on the effect of adjusting the ratio of Banxia Xiexin Decoction and bitterness to reduce insulin resistance in type 2 diabetes. Guangming Journal of Chinese Medicine 2014;29:1522-4.
- Yaowu Z. A Clinical Observation of Banxiaxiexin Decoction on the Treatment of 60 Diabetes Patients with Spleen Deficiency and Stomach Heat Type. Yunnan Journal of Traditional Chinese Medicine and Materia Medica 2014;35:34-6.
- Yugang Z, Dahu T, Chao M. Clinical observation on treatment of qi and yin deficiency type 2 diabetes with dried turmeric and Huanglian ginseng soup. Shaanxi Journal of Traditional Chinese Medicine 2017;38:568-9.
- Jing W, Qingyu W. Clinical observation of 30 cases of type 2 diabetes mellitus treated with dried turmeric and Huanglian Ginseng Decoction. Guide of China Medicine 2016;14:194-5.
- Jianying W. Clinical observation of metformin combined with dried turmeric and Huanglian Ginseng Decoction in the treatment of type 2 diabetes mellitus. Information on Traditional Chinese Medicine 2014;31:80-2.
- Xinyan C, Shoushu J, Hangyu J, et al. Clinical observation of using Ginger Skullcap Coptis Ginseng Decoction in treating 80 patients with type 2 diabetes. China Journal of Traditional Chinese Medicine and Pharmacy 2013;28:463-5.
- Gengzhong X, Yanhui H, Zhiling Z, et al. Clinical Observation on the Treatment of Cold-heat Mixture of Type 2 Diabetes Mellitus with Wumei Pill. Clinical Journal of Traditional Chinese Medicine 2017;29:1272-6.
- Wei N. Evaluation on Curative Effect of Classical Prescription of Wumeiwan in Treatment of Type 2 Diabetes in Upper Heat and Lower Cold. Diabetes New World 2017;20:72-3.
- Zheng Lixing, Lei W, Yi L, et al. Clinical observation of Wumei Wanhua cut prescription in the treatment of type 2 diabetes mellitus. Clinical Focus 2008;23:1150-2.
- Bo D, Zhiyang O. Therapeutic effect of Qiju Dihuang Pill on type 2 diabetes mellitus in elderly patients with liver and kidney yin deficiency. Clinical Journal of Traditional Chinese Medicine 2005;17:544-5.
- Ming D, Shuiyan Z, Yiheng L. Clinical observation of Jinqi Shenqi Pills combined with metformin in the treatment of type 2 diabetes mellitus in the elderly. Strait Pharmaceutical Journal 2015;27:118-20.
- Fushu X. Therapeutic effect of Jinqi Shenqi Pills on 106 cases of diabetes mellitus. China Health Industry 2012;9:159.
- Lina C. Clinical observation on Jinkui Shenqi Pill in the treatment of 60 patients with type 2 diabetes mellitus. China Medical Herald 2012;9:102-3.
- Xin J. Therapeutic effect of Jinqi Shenqi Pills on 50 cases of diabetes mellitus. China Modern Doctor 2011;49:60.
- Dehua L. Clinical Observation on Treatment of 62 Cases of Type 2 Diabetes with Yin and Yang Deficiency Type by Jinqi Shenqi Pill. Journal of New Chinese Medicine 2004;36:31-2.
- Zhiyong Z. Treatment of 23 Cases of Type 2 Diabetes with Fuzi Lizhong Decoction. Henan Traditional Chinese Medicine 2013;33:1647-8.
- Huazhen C, Guimei W, Yonghua D, Fusheng W. Effects of Shenling Baizhu San and Erchen decoction and acupuncture on insulin resistance in type 2 diabetes mellitus. Clinical Journal of Chinese Medicine 2014;6:1-3.
- Chunhong W. Therapeutic effect of Xuefu Zhuyu Decoction and Erchen Decoction on obesity type 2 diabetes Xuefuzhuyu Decoction Aggregate Erchen Decoction Treatment of Obesity and Type 2 Diabetes Efficacy. China & Foreign Medical Treatment 2013;32:6-7.
- Ying Z, Xiaojing L, Tao J. Therapeutic effect of Xuefu Zhuyu Decoction and Erchen Decoction on obesity type 2 diabetes mellitus. Liaoning Journal of Traditional Chinese Medicine 2007;34:1089-90.
- Guoqing Z, Jufu Z, Jinwei Z. Effect of Qilianpingwei Powder on type 2 diabetes mellitus with dampness and heat syndrome and blood sugar and blood lipids Shaanxi Journal of Traditional Chinese Medicine 2011;32:425-6.
- Haixia Z, Mingbo L. An observation of the clinical effect of Taohong Siwu decoction in the treatment of T2DM. China Medicine and Pharmacy 2014;4:78-80.
- Lingzhen Z, Xiaozheng L, Caixin Y. Analysis of Jiawei Taohong Siwu Decoction in the Treatment of Type 2 Diabetic Peripheral Neuropathy with Qi and Yin Deficiency and Blood Stasis Syndrome. Chinese Archives of Traditional Chinese Medicine 2005;23:378-9.
- Yingchun Z. Add and Subtract in When soup Treatment the Clinical Curative Effect of Phlegm and Blood Stasis Type of Type 2 Diabetes. Diabetes New World 2016;19:45-6.
- Gong D, Caiyun S, Yucui C, Zhiyan C. Clinical observation of modified Didang decoction on the treatment of type 2 diabetes with blood stasis - phlegm type. Hebei Journal of Traditional Chinese Medicine 2015;37:1667-70.
- Tong X, Zhao H, Lian F, et al. Clinical observations on the dose-effect relationship of Gegen Qin Lian Decoction on 54 out-patients with type 2 diabetes. J Tradit Chin Med 2011;31:56-9. [Crossref] [PubMed]
- Yao D, Cheng SJ. Effect of Bai Hu Jia Renshen Decoction on type 2 diabetes. Zhong Yao Yao Li Yu Lin Chuang 2015;31:300.
- Li K, Ma L. Shengmai Powder for type 2 diabetes mellitus: A systematic review and meta analysis. Zhong Cheng Yao 2009;31:20-3.
- Li K, Ma L. Liu wei Dihuang Wan for treating type 2 diabetes mellitus: A systematic review and meta analysis. Shan Dong Zhong Yi Za Zhi 2009;28:684-6.
- Ming S, Liu Y, Yang T. Shenqi Pill combined western medicine therapy for type 2 diabetes clinical randomized controlled trial system evaluation. Zhong Yi Yao Lin Chuang Za Zhi 2015;27:645-9.