
Family support is beneficial to the management and prognosis of patients with obstructive sleep apnoea
Introduction
Obstructive sleep apnoea (OSA) is a chronic disorder of the upper respiratory system that is characterized by the repetitive collapse of the upper airway during sleep. The collapse results in hypoxemia along with increased sympathetic overdrive, blood pressure, and carbon dioxide levels in the blood. The resulting hypoxia is, in turn, linked with a wide range of problems stemming from oxidative stress and inflammation, including multiple cardiovascular morbidities and coronary artery-related and all-cause mortality (1). Furthermore, OSA is closely related to metabolic syndrome, including obesity, hyperlipidaemia, hypertension, and diabetes (2).
Patients with OSA must consistently receive continuous positive airway pressure (CPAP) to attain improved functional outcomes and reduce the health risks associated with OSA. Unfortunately, the nonadherence rates of CPAP are high (3). Weaver et al. (4) noted that the domain-specific self-efficacy of patients with OSA might influence CPAP compliance. Stepnowsky et al. further confirmed that self-efficacy and outcome expectation had significantly positive correlations with CPAP compliance (5). Presently, there are few studies on how OSA patients’ self-efficacy relates to family support; most existing studies on CPAP compliance interventions for patients with OSA focused on strategies such as social support cognition (6,7). The purpose of this study was to investigate the self-efficacy and family support of patients with OSA, and to examine the correlation between the two. Ultimately, we hoped to provide further knowledge for improving patients’ treatment compliance.
CPAP is the most common and efficacious therapy for OSA. It has been demonstrated to safely and effectively manage OSA symptoms with regular long-term use, but its therapeutic benefits depend on treatment adherence (2). Specifically, it should be used for more than 4 h/night. Currently, adherence rates to CPAP are low, and there is little evidence regarding how adherence might be improved (8,9). As noted, Weaver et al. (4) and Stepnowsky et al. (5) both showed that improving the self-efficacy of OSA patients might help to improve compliance with CPAP treatment. Lai et al. (10) also found that the better the adherence to CPAP treatment, the greater the improvements in patients’ treatment self-efficacy. Moreover, spouse involvement has been reported to be an important determinant of male patients’ CPAP treatment within the first six months after treatment initiation (11).
Methods
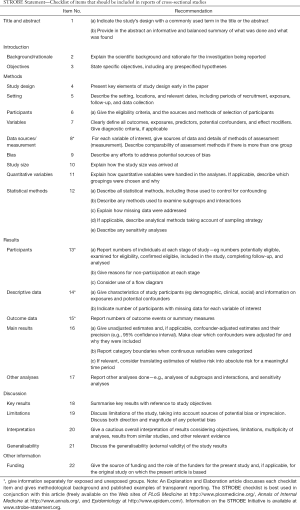
The study conforms to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) statement (see Supplementary).
Research subjects
Convenience sampling was used to select patients who received a diagnosis of OSA between May 1 and Dec 30, 2017 at the Sleep Respiration Monitoring Centre of Ningbo First Hospital, Zhejiang Province, China. The inclusion criteria for this study were as follows: (I) diagnosed with OSA; (II) treated in the emergency wards, otorhinolaryngology wards, respiratory wards, and outpatient clinic of the study hospital; (III) treated with a home ventilator; (IV) aged ≥18 years; and (V) capable of communicating normally. The exclusion criterion was being unwilling to participate in the study.
Assessment tools
Self-efficacy Measure for Sleep Apnoea (SEMSA)
Weaver et al. (4), from the University of Pennsylvania in the United States, developed the SEMSA to evaluate social cognitive factors related to CPAP therapy among OSA patients. This scale contains 26 items, including eight items related to disease risk perception (all rated on a scale ranging from 1 point for ‘very low’ to 4 points for ‘very high’) and nine items each for outcome expectation and self-efficacy (each rated on a scale ranging from 1 point for ‘completely incorrect’ to 4 points for ‘very correct’). These three subscale scores are independent of each other and cannot be added. The subscale score is calculated as the average of all item scores within that subscale. Higher scores indicate higher disease risk perception, outcome expectation, and self-efficacy. The Chinese version of the SEMSA combines items 2 and 6 from the original version to better suit a Chinese context; thus, the total number of items in the Chinese version of the SEMSA is 25 (including seven items for disease risk perception). The Cronbach’s α coefficient of the original scale was 0.92, and the coefficients of the three subscales were all greater than 0.85. The Cronbach’s α coefficient of the Chinese version was 0.886, and the coefficients of the three subscales were between 0.701 and 0.895, with the highest being that of the self-efficacy dimension (0.895); the split-half reliability coefficient was 0.851.
Perceived Social Support from Family (PSS-Fa) Scale
The PSS-Fa scale was designed by Procidano and Heller (12) in USA. It consists of 15 items, each answered with ‘yes’ or ‘no’. An answer of ‘yes’ is given 1 point and an answer of ‘no’ is given 0 points, so the total score ranges from 0 to 15. Higher scores indicate higher family support. Participants’ level of family support can be classified into three levels depending on their total score: low (0–5 points), medium (6–10 points), and high (11–15 points). The Cronbach’s α coefficient in this study was 0.711.
Data collection methods
With the approval of the hospital’s ethics committee (2019-R071), we explained the purpose of this investigation to potential participants. After obtaining their consent, we administered the questionnaires using a unified set of procedures. The questionnaires were collected on the spot to avoid the possibility of missing items. A total of 120 questionnaires were distributed, and 112 valid questionnaires were recovered (effective recovery rate: 93.33%).
Statistical methods
The data were input into Microsoft Excel and then imported to SPSS Statistics 22.0 (SPSS version 22.0; IBM Corp., Armonk, NY, USA) software for analysis, after they had been double-checked for accuracy. Participants’ general characteristics, SEMSA score, and PSS-Fa score were described in terms of frequencies, percentages, and means ± standard deviations. Pearson correlation analysis was used to determine the correlation between self-efficacy and family support.
Results
Participants
This study recruited 112 participants including 99 males (88.4%) and 13 females (11.6%). More information regarding participants is shown in Table 1.
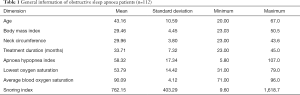
Full table
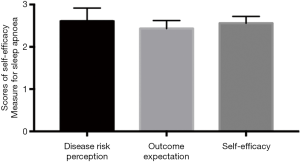
SEMSA scores
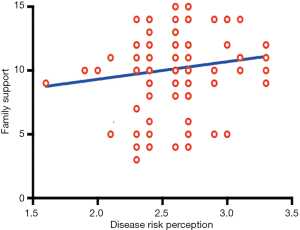
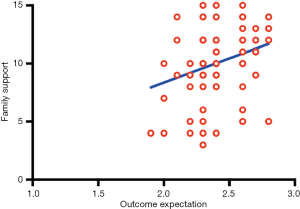
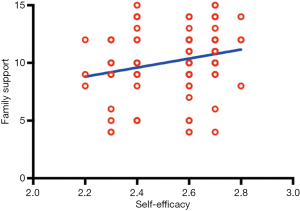
The average scores for disease risk perception, outcome expectation, and self-efficacy were 2.61±0.31, 2.44±0.17, and 2.55±0.13, respectively (Table 2 and Figure 1).
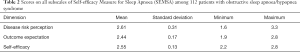
Full table
Family support scores
The mean total score of the PSS-Fa was 10.15±2.73 (range, 3–15). Among them, 12 cases were defined as having low support levels (10.7%), 51 cases as having medium support levels (45.5%), and 49 cases as having high support levels (43.8%) (Table 3).

Full table
Correlation between self-efficacy and family support
A Pearson correlation analysis was used to compare and examine the associations of the three subscales of the SEMSA (disease risk perception, outcome expectation, and self-efficacy) and the total score of the PSS-Fa among patients with OSA. The results showed that the outcome expectation scores (P<0.01) and self-efficacy scores (P<0.01) were positively correlated with family support level, as shown in Table 4 and Figures 2-4.
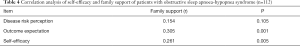
Full table
Discussion
In this study, the subscale scores of the SEMSA were lower than those reported by Sawyer et al. (13). A possible reason for this discrepancy is that patients in the latter study were newly diagnosed with OSA and different underlying diseases.
Our results further showed that patients’ outcome expectation and self-efficacy scores were significantly and positively correlated with the level of family support (P<0.01). This finding is consistent with the results of Puspasari et al. (14), who found that family support was positively correlated with the self-efficacy of adolescent mothers. No harm/side effects of family support were found in this study. Taken together, these findings indicate that the higher the level of family support, the higher the patient’s self-efficacy for CPAP treatment.
Family support may also increase treatment compliance in OSA patients. This is supported by Hu et al. (15) who found a positive correlation between family social support and medication compliance among hypertension patients. Moreover, in her interview study, Luyster asserted that spousal support may be an effective strategy for improving patients’ CPAP compliance (16). Batool-Anwar et al. (11) reported that marriage is an important determining factor in the first six months of CPAP therapy among male patients with OSA. Thus, spousal factors can be considered as the initial motivation for patients to start CPAP therapy.
According to past literature and the results of this study, family support should be considered an important contributor to the self-efficacy of patients with OSA and it may be beneficial to the management of these patients’ treatment. Numerous studies have been conducted on how to improve CPAP treatment compliance (9,10,17), but our results suggest that further research is necessary. Particularly, interventions should be designed to effectively engage patients’ families or partners to optimize CPAP adherence (18).
A previous study showed that 85.5% of nurses perceive themselves to have inadequate fundamental knowledge of health education and feel ill-equipped to provide family support interventions (19). If nursing departments strengthen the on-the-job training of nurses in family support interventions, this may be conducive to more effective communication with patients and relatives, which, in turn, could improve patients’ utilization of family support. After such training, nurses could instruct patients’ families in obtaining more knowledge of the disease and its rehabilitation and lead them to enthusiastically participate in the implementation of patients’ rehabilitation.
When OSA patients are admitted to the hospital, nurses should establish a good relationship with patients and their families, comprehensively evaluate the quality of life and family support of patients, and strive to establish stable, trustworthy, and cooperative relations with all family members as soon as possible. This is close to the result of Broström et al. (20). Before discharge, nurses, patients, and patients’ families should determine a self-care plan for patients that will be enacted after discharge. These plans are often based on patients’ family conditions and require family members to work with patients. Nurses should provide telephone counselling on patients’ health problems and provide continuing care for patients through applications such as WeChat. Moreover, they can hold regular seminars on self-management of CPAP to improve patients’ knowledge of self-care. Family members should assist patients in recording their SPO2 daily as well as evaluate and summarize the effect of treatment.
Due to limited human and material resources, this study only investigated the self-efficacy and family support of OSA patients during CPAP treatment; it did not comprehensively study other relevant factors such as CPAP treatment compliance and family intimacy. Future research should investigate these factors in detail. Further, although the results of our study could provide some suggestions for CPAP treatment-related education for OSA patients, we did not carry out such education or training for patients and their family members. In the future, such education programs should be developed and their efficacy should be examined.
Relevance to clinical practice
Family support, as an important part of patients’ social support, is closely related to patients’ self-efficacy. It is suggested that clinical nurses should attach importance to and obtain the support of patients’ family members, partners, and other people who have a close relationship with patients when carrying out health education for OSA patients. Family members play an important role of supervision, encouragement, and support in the long-term self-management of OSA patients.
Conclusions
In summary, the self-efficacy of OSA patients undergoing CPAP treatment is closely related to their family support. Improving the family support of OSA patients undergoing CPAP treatment can play a role in enhancing their treatment-related self-efficacy. Future CPAP treatment-related health education programs for OSA patients should emphasize the importance of participation of patients’ family members.
Supplementary
Full table
Acknowledgments
The directors of emergency, otolaryngology, respiratory and outpatient departments supported the promotion of this study.
Funding: This study was supported by a grant from the Ningbo First Hospital: Study on CPAP Compliance and Self-efficacy Management of OSAHS Patients (Grant number: H2017YJ001).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-19-310). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics committee of Ningbo First Hospital (2019-R071). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Libman E, Bailes S, Fichten CS, et al. CPAP Treatment Adherence in Women with Obstructive Sleep Apnea. Sleep Disord 2017;2017:2760650. [Crossref] [PubMed]
- Deering S, Liu L, Zamora T, et al. CPAP Adherence is Associated With Attentional Improvements in a Group of Primarily Male Patients With Moderate to Severe OSA. J Clin Sleep Med 2017;13:1423-8. [Crossref] [PubMed]
- Sawyer AM, Deatrick JA, Kuna ST, et al. Differences in perceptions of the diagnosis and treatment of obstructive sleep apnea and continuous positive airway pressure therapy among adherers and nonadherers. Qual Health Res 2010;20:873-92. [Crossref] [PubMed]
- Weaver TE, Maislin G, Dinges DF, et al. Self-efficacy in sleep apnea: instrument development and patient perceptions of obstructive sleep apnea risk, treatment benefit, and volition to use continuous positive airway pressure. Sleep 2003;26:727-32. [Crossref] [PubMed]
- Stepnowsky CJ Jr, Marler MR, Ancoli-Israel S. Determinants of nasal CPAP compliance. Sleep Med 2002;3:239-47. [Crossref] [PubMed]
- Bartlett D, Wong K, Richards D, et al. Increasing adherence to obstructive sleep apnea treatment with a group social cognitive therapy treatment intervention: a randomized trial. Sleep 2013;36:1647-54. [Crossref] [PubMed]
- Dai Y, Li X, Zhang X, et al. Prevalence and Predisposing Factors for Depressive Status in Chinese Patients with Obstructive Sleep Apnoea: A Large-Sample Survey. PLoS One 2016;11:e0149939. [Crossref] [PubMed]
- Park P, Kim J, Song YJ, et al. Influencing factors on CPAP adherence and anatomic characteristics of upper airway in OSA subjects. Medicine (Baltimore) 2017;96:e8818. [Crossref] [PubMed]
- Pépin JL, Tamisier R, Hwang D, et al. Does remote monitoring change OSA management and CPAP adherence? Respirology 2017;22:1508-17. [Crossref] [PubMed]
- Lai AYK, Fong DYT, Lam JCM, et al. The efficacy of a brief motivational enhancement education program on CPAP adherence in OSA: a randomized controlled trial. Chest 2014;146:600-10. [Crossref] [PubMed]
- Batool-Anwar S, Baldwin CM, Fass S, et al. Role of Spousal Involvement in Continuous Positive Airway Pressure (CPAP) Adherence in Patients with Obstructive Sleep Apnea (OSA). Southwest J Pulm Crit Care 2017;14:213-27. [Crossref] [PubMed]
- Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol 1983;11:1-24. [Crossref] [PubMed]
- Sawyer AM, King TS, Hanlon A, et al. Risk assessment for CPAP nonadherence in adults with newly diagnosed obstructive sleep apnea: preliminary testing of the Index for Nonadherence to PAP (I-NAP). Sleep Breath 2014;18:875-83. [Crossref] [PubMed]
- Puspasari J, Nur Rachmawati I, Budiati T. Family support and maternal self-efficacy of adolescent mothers. Enferm Clin 2018;28 Suppl 1:227-31. [Crossref] [PubMed]
- Hu HH, Li G, Arao T. The association of family social support, depression, anxiety and self-efficacy with specific hypertension self-care behaviours in Chinese local community. J Hum Hypertens 2015;29:198-203. [Crossref] [PubMed]
- Luyster FS. Impact of Obstructive Sleep Apnea and Its Treatments on Partners: A Literature Review. J Clin Sleep Med 2017;13:467-77. [Crossref] [PubMed]
- Chang J, Kim J, Becker K, et al. Impact of automated web-education and CPAP tele-monitoring on CPAP adherence at 3 months and 1 year: the tele-OSA randomized clinical trial. Sleep 2017;40:A189-A190. [Crossref]
- Ye L, Kayser K, Gautam S, et al. Spousal involvement in adherence to CPAP treatment. Sleep 2017;40:A190. [Crossref]
- Li S, Di W. Factors influencing health education for cancer patients and nursing strategies. J Nurs Adm 2004;4:18-20.
- Broström A, Fridlund B, Hedberg B, et al. Communication between patients with obstructive sleep apnoea syndrome and healthcare personnel during the initial visit to a continuous positive airway pressure clinic. J Clin Nurs 2017;26:568-77. [Crossref] [PubMed]


