
Effects of atorvastatin combined with bivalirudin on coagulation function, cardiac function, and inflammatory factors of percutaneous coronary intervention in elderly patients with acute myocardial infarction
Introduction
Acute myocardial infarction (AMI) occurs when atherosclerotic lesions which present in the coronary arteries cause the intravascular plate to rupture; this occludes the lumen, blocking the blood vessels and leading to a sharp decrease in the amount of blood returning to the heart. The result is myocardial ischemia, hypoxia, and infarct (1). Clinical data show that elderly patients are more likely to experience AMI, and the incidence is particularly high among those with chronic diseases such as hypertension and diabetes. Along with China’s ageing population, the incidence of AMI is increasing annually (2,3). The treatment of AMI has been reported to be continuously improved, with the mainly represented drugs such as intravenous thrombolysis, β-blockers and angiotensin converting enzyme inhibitors. the percutaneous coronary intervention (PCI) is currently the preferred surgical method for the treatment of AMI, and the choice of anticoagulant and thrombolytic drugs during the operation is the key to the success of the operation (4,5).
Zhang et al. have reported that for the treatment of patients with AMI who undergo PCI, compared with the use of unfractionated heparin, the use of bivalirudin will shows a better anticoagulant effect (6). Bivalirudin is a new kind of anticoagulant. which has significantly better effects on postoperative bleeding and fewer postoperative side effects, compared with unfractionated heparin. Atorvastatin is a statin commonly used in clinic, which can effectively promote the repair of vascular endothelium while preventing bleeding, and improve the function of myocardium. At present, there are few clinical studies on the combination of atorvastatin and bivalirudin of improving clinical symptoms and accelerating the recovery of cardiac function in patients after PIC. Therefore, this study used atorvastatin combined with bivalirudin to treat AMI patients after the PIC treatment. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-925).
Methods
Patients
Patients with AMI who were treated in our hospital between February, 2016, and May, 2018, were enrolled and their clinical data retrospectively analyzed.
Inclusion criteria: (I) diagnosed with AMI and meet the clinical diagnostic criteria; (II) aged ≥60 years; (III) with an onset time ≤12 h. Exclusion criteria were excluded from the study: (I) patients with severe immunodeficiency, coagulation dysfunction, and tumor diseases; (II) allergic to the study drug; (III) recently received other anticoagulants; or (IV) incomplete information.
A total of 86 patients met the criteria. Based on different treatment methods, they were divided into the control group (n=43) and the observation group (n=43). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the hospital’s ethics committee, and signed informed consent was obtained from each patient.
Treatment
Before surgery, both groups of patients underwent routine establishment of venous access, and were given anticoagulation, dilatation, angiotensin, and other drugs to maintain their water-electrolyte balance. An ECG monitor was installed to closely monitor the patient’s vital signs. The patients in the control group were treated with bivalirudin during PIC. The bivalirudin (Jiangsu Haosen, H20051408, China) was in a specification of 250 mL/bottle. Before PCI, the patients were intravenously injected with 0.75 mg/kg bivalirudin. At the completion of the surgery, an intravenous drip of 1.75 mg/kg/h was immediately given, with a total intravenous drip time ≤4 h. After 5 min, the activated coagulation time of the patient was checked; if necessary, a 0.3 mg/kg intravenous drip was maintained. The observation group was given bivalirudin (as in the control group) plus 20 mg of atorvastatin (Pfizer, USA) at 2 and 12 h before surgery, and for 4 weeks after surgery (20 mg/time).
After 4 weeks of treatment, the treatment efficacy was compared between the 2 groups with comparison and analysis of their cardiac function, coagulation function and inflammatory factor levels.
Index observation and efficacy judgment
Efficacy judgment
After treatment, the clinical efficacy was observed in the two groups and was judged as significantly effective, effective, or ineffective, according to the relevant literature (7). Significantly effective was defined as those patients with: no clinical symptoms or signs; recanalization of the blood vessels; residual stenosis of the target lesion <20%, confirmed by coronary angiography; no severe coronary events occurring within 24 hours after the operation, and no significant bleeding. Effective was defined as those patients with: significantly improved symptoms and signs; residual stenosis of the target lesion of 20% to 40%, confirmed by coronary angiography; and only mild coronary symptoms occurring within 24 hours after the operation. Ineffective was judged as those patients with: no improvement in symptoms and signs; residual stenosis of the target lesion >40%, confirmed by coronary angiography; and serious coronary events occurring within 24 hours after surgery. The total effective rate = (significantly effective + effective)/total number of cases ×100%.
Detection of inflammatory factors and coagulation function
Before and after treatment, the patients were tested for inflammatory factors. On the morning of the operation, 5 mL of fasting venous blood was taken. After anticoagulation centrifugation for 10 min, the supernatant was taken and stored at −20 °C for testing. The instrument of flow cytometer and matching kit (B & D, New Jersey, USA) were used for the detection the levels of main factors such as serum transforming growth factor-β1 (TGF-β1), tumor necrosis factor-α (TNF-α) and IL-6, with the method of radioimmunoassay. The coagulation function of patients was detected by ELISA to check the main indicators of fibrin (Fg), D-dimer (D-D) and prothrombin time (PT). The experimental procedures were strictly in accordance with the kit instruction.
Heart function test
The left ventricular end-diastolic diameter (LVEDD), left ventricular ejection fraction (LVEF), and left ventricular end-systolic diameter (LVESD) were monitored before and after treatment, and the incidence of MACE within one month after treatment was compared.
Statistical methods
SPSS 18.0 statistical software package (IBM, USA) was used for data analysis. Measurement data were analyzed using t-test and expressed as
Results
Patient clinical information
The clinical data of 86 patients with AMI who were treated in our hospital between February 2016 and May 2018 were retrospectively analyzed. Included in the study were 41 males and 45 females, aged from 60 to 75 years of age, with an average age of (68.59±3.24) years. Chronic disease types in the entire cohort included hypertension (n=29), diabetes (n=33), and hyperlipidemia (n=24). For the number of diseased vessels, there were 39 cases of single branch lesions, 33 cases of bifurcation lesions, and 14 cases of multivessel lesions. There was no significant difference between the two groups of patients in terms of general clinical data such as age, gender, and types of concomitant diseases (P>0.05).
Comparison of clinical efficacy between the two groups
The total clinical effective rate after treatment in the observation group (90.90%) was significantly higher than that in the control group (72.09%) (P<0.05, Table 1).

Full table
Comparison of coagulation function before and after treatment between the two groups
There was no significant difference in the levels of Fg, DD, or PT between the two groups before treatment (P>0.05). However, after treatment, Fg and DD were significantly decreased in both groups but were significantly lower in the observation group than in the control group. PT was significantly longer in both groups after treatment but was significantly longer in the observation group than that in the control group (P<0.05, Table 2).

Full table
Comparison of cardiac function indexes before and after treatment in the two groups
There was no significant difference in the indexes of LVEDD, LVEF, and LVESD between the two groups before treatment (P>0.05). After treatment, LVEDD and LVESD were significantly reduced in both groups but were significantly lower in the observation group than in the control group, while the LVEF was significantly increased in the observation group compared with the control group (P<0.05, Table 3).
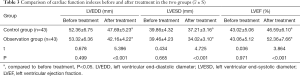
Full table
Comparison of inflammatory factor levels before and after treatment in the two groups
There was no significant difference in serum TGF-β1, TNF-α, or IL-6 levels before treatment (P>0.05). The level of each factor was significantly decreased after treatment in both groups, but the levels were significantly lower in the observation group than in the control group after treatment (P<0.05, Table 4).
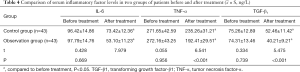
Full table
Comparison of the occurrence of MACE after treatment between the two groups
The overall incidence of MACE in the observation group (9.30%) was significantly lower than that in the control group (30.23%), and the difference between the two groups was statistically significant (P<0.05, Table 5).

Full table
Discussion
With the advancements in medical technology in China, PCI has been widely popularized in clinical practice. PIC has important significance for the treatment and prognosis of AMI patients, and has simultaneously reduced the mortality (8). It is worth noting that during PIC surgery, plaque compression and damage can easily occur, resulting in “self-induced thrombus” and “contact thrombus” from the instrument (9). Clinical data has reported that for patients with high-risk AMI, the use of common anticoagulants during PIC surgery can induce bleeding, thereby reducing the success rate of PIC and increasing the risk of death (10). Therefore, the choice of drugs during PIC surgery is extremely important.
Bivalirudin, as a new thrombin inhibitor, has been identified as having a short-term anticoagulant effect during surgery and is easy to control. Because the inhibition of thrombin is transient, it holds a significant advantage over conventional anticoagulants in the reduction of adverse reactions to intraoperative bleeding (11). Atorvastatin has multidirectional effects. According to clinical pharmacological experiments, atorvastatin has a positive effect on inflammatory responses and stable plaques, which can reduce the occurrence of cardiovascular events by improving vascular endothelial function (12). Wan et al. showed that atorvastatin has a certain lipid regulation capacity to reduce blood lipids, and thus lowers the risk of thrombosis (13). Taken together, these findings suggest that the combination of these two drugs may improve the success rate of PCI surgery.
In this study, the data showed that the total clinical effectiveness of the observation group was significantly higher than that of the control group, suggesting that compared with bivalirudin alone, atorvastatin combined with bivalirudin could improve the total clinical effectiveness. Bleeding is common during the PIC procedure due to the use of anticoagulants during the procedure, which can cause continuous bleeding and lead to the occurrence of cardiovascular events. Bivalirudin can reduce the occurrence of continuous bleeding while inhibiting thrombosis (14,15). Atorvastatin repairs the damaged blood vessel wall and promotes inflammatory absorption. The combined use of these two drugs can greatly improve patients’ clinical symptoms (16).
In the comparison of coagulation function, Fg and D-D were significantly decreased in both groups after treatment and were significantly lower of the observation group than the control group. After treatment, the PT was significantly prolonged and was significantly longer in the observation group than in the control group.
As an important coagulation factor in the blood, Fg mainly reflects the body’s coagulation function, which, when elevated, indicates that the blood is in a hypercoagulable state and is a risk factor for thrombosis (17). D-D is a specific degradation product in the body, and its increase can stimulate fibrinolytic activity, which is a molecular marker indicative of the body’s hypercoagulable state (18). Changes in Fg and D-D levels play an important role in the development of AMI. It is also reported in other literature that the high levels of Fg and D-D in vivo can be deposited on the lining of blood vessels, causing damage to the vascular endothelium, while reducing arterial blood flow velocity and the amount of blood returning to the heart, finally resulting in myocardial ischemia (19). PT is an important indicator that reflects the degree of clotting, and its prolongation can reduce the blood coagulation speed, thereby reducing the formation of thrombus.
In the comparison of various indexes of cardiac function between the two groups, after treatment, LVEDD and LVESD were significantly decreased, and LVEF was significantly increased, which indicated that both treatments could improve cardiac function to a certain extent. Increased LVEDD and LVESD can promote ventricular remodeling after myocardial infarction. Due to the enlargement of the infarct area, myocardial contractility is significantly reduced, which is prone to be compensatory tachycardia. The long-term overload result is the occurrence of myocardial reactive hypertrophy. The level of LVEF mainly reflects the amount of cardiac transfusion (20). The data in this group showed that the total incidence of MACE in the observation group (30.23%) was significantly lower than that in the control group (9.30%), indicating that the combination of drugs can effectively maintain cardiac function, reduce the occurrence of cardiovascular events, and is safe and effective. After treatment, the improvement of each index in the observation group was obviously better than that in the control group, indicating that the improvement of heart cardiac function after combined medication is better. Some studies have indicated that during the development of AMI, the increase in inflammatory cells is a key cause of early arteriosclerosis. The diffusion of inflammation promotes the proliferation of smooth muscle and the disorder of the arrangement of collagen fibers under the intima, which is a core factor in the occurrence of arteriosclerosis (21). After treatment, the levels of serum TGF-β1, TNF-α, IL-6 and factor in the two groups in this study were significantly reduced, and the indicators in the observation group were significantly lower than those in the control group. TGF-β1, NF-α, IL-6 can induce the production of Hs-CRP. Hs-CRP is often used as a non-specific systemic inflammation marker protein, and its increase reflects the spread of inflammation in the body, which shows great significance in the pathological process and the evaluation of treatment as well as in the outcomes of AMI patients.
In summary, compared with bivalirudin alone, atorvastatin combined with bivalirudin can improve the clinical effectiveness of PCI in elderly patients with AMI, including by improving blood coagulation function and reducing bleeding at the same time, decreasing the level of inflammatory factors, promoting vascular recanalization, and improving myocardial ischemia. Ultimately, it can decrease the incidence of MACE and improve the prognosis of the patient.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-925
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-925
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-925). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the hospital’s ethics committee, and signed informed consent was obtained from each patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rout A, Tantry US, Novakovic M, et al. Targeted pharmacotherapy for ischemia reperfusion injury in acute myocardial infarction. Expert Opin Pharmacother 2020.1-15. [Crossref] [PubMed]
- Pi SF, Liu YW, Li T, et al. Effect of sequential nicorandil on myocardial microcirculation and short-term prognosis in acute myocardial infarction patients undergoing coronary intervention. J Thorac Dis 2019;11:744-52. [Crossref] [PubMed]
- Guo W, Yang D, Wu D, et al. Hyperuricemia and long-term mortality in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Ann Transl Med 2019;7:636. [Crossref] [PubMed]
- Oliveira MDP, Navarro EC, Kiemeneij F. Distal transradial access as default approach for coronary angiography and interventions. Cardiovasc Diagn Ther 2019;9:513-9. [Crossref] [PubMed]
- Russo JJ, Bagai A, Le May MR, et al. Immediate non-culprit vessel percutaneous coronary intervention (PCI) in patients with acute myocardial infarction and cardiogenic shock: a swinging pendulum. J Thorac Dis 2018;10:661-6. [Crossref] [PubMed]
- Zhang HF, Dong PS, Wang K, et al. Comparison in curative effects between unfractionated heparan and bivalirudin in patients with acute myocardial infraction during PCI. Chin J Evid Based Cardiovasc Med 2018;26:147-9.
- Hasija S, Kapoor PM. Effect of heparin and bivalirudin on the kinetics of clot formation: viscoelastic coagulation testing. Ann Card Anaesth 2017;20:122. [Crossref] [PubMed]
- You SL, Wang Z. Clinical Efficacy and Bleeding Risk of Tigrilol Combined with Bivaludine in Patients with Acute Coronary Syndrome (ACS) Treated with Emergency PCI. J Clin Res 2018;35:706-9.
- Franchi F, Rollini F, Angiolillo DJ. Antithrombotic therapy for patients with STEMI undergoing primary PCI. Nat Rev Cardiol 2017;14:361. [Crossref] [PubMed]
- Liu G, Chang YF, Zhu HX, et al. Clinical safety of bivalirudin combined with ticagrelor and unfractionated heparin combined with clopidogrel in emergency interventional therapy in elderly patients with acute myocardial infarction. Chinese Journal of Integrative Medicine on Cardio- Cerebrovascular Disease 2018;16:142-423.
- Jin C, Song Y, Zu W, et al. The changes and significance of BNP and NT-proBNP in blood before and after PCI in patients with AMI. Med J West China 2017;29:1421-4.
- Chen y, Xie W, Su ZQ, et al. Effects of tirofiban combined with bivalirudin on myocardial perfusion after emergency PCI in patients with STEMI. Drug Evaluation Research 2018;21:223-4.
- Wan P, Fu Q, Zhang Q, et al. Effect of statins therapy on the levels of serum proprotein convertase subtilisin/kexin 9 in acute ST elevation myocardial infarction. Journal of Jiangsu University Medicine Edition 2017;27:64-8.
- Zhang HF, Dong PS, Wang K, et al. Comparison in curative effects between unfractionated heparin and bivalirudin in patients with acute myocardial infarction during PCI. Chin J Based Cardiovasc Med 2018;16:251-2.
- Lei XY, Guo DL, Zhang ZG. Application of ticagrelor combined with bivalirudin in direct percutaneous coronary intervention in patients with type 2 diabetes mellitus combined with ST-segment elevation myocardial infarction. Shanxi Medical Journal 2017;24:3059-62.
- Gao HW, Wei HS, Niu ZS, et al. Comparison of the efficacy and safety between Bivalirudin and Heparin during emergency percutaneous coronary intervention in elderly patients with acute ST-segment elevation myocardial infarction. Chin J Geriatr 2017;36:410-1.
- Sun SX, Ma W, Zhang Y, et al. Effects of Bivalirudin on myocardial perfusion and infarct size in acute stage for elderly patients with thrombolytic failure and salvage PCI. J Clin Cardiol 2018;16:166-7.
- Feng XX, Zhu BD, Xu XD, et al. Effects of Bivalirudin on ICAM-1 Level in Plasma of Patients Undergoing Percutaneous Coronary Intervention. China Pharmacist 2017;20:1391-2.
- Wang WM, Wang H, Li Z. Effect of bivalirudin on endothelial injury and inflammatory reaction after PCI in patients with acute coronary syndrome. Anhui Medical Journal 2017;38:1016-9.
- Li H, Li CM, Ye MX, et al. Risk factors for elderly patients with acute myocardial infarction complicated with severe arrhythmia. Medical Journal of Air Force 2017;33:118-20.
- Wang ZY, Li G, Zhang LK, et al. Study on the efficacy and safety of bivalirudin in PCI for patients with acute coronary syndrome at high risk of bleeding. Chin J Based Cardiovasc Med 2017;14:1034-6.


