
Clinical effect of Rougan Tongdu combined with point-pressing massage therapy on children at high risk of delayed motor development
Introduction
Delayed motor development (DMD) is an extremely common development disorder in children. It is clinically manifested as obvious growth retardation at all ages. Multiple factors, including mother’s influence, diseases, physical or chemical factors and trauma, are strongly associated with DMD. Without effective treatment in time, it causes cognitive impairment and behavioral defects to various degrees (1). Research into DMD has indicated that for children at high risk of the disorder, early clinical intervention can, to a certain extent, reverse and repair damaged brain function, significantly reduce the sequelae of brain injury, and improve the child’s prognosis and their quality of life (1-4). This study enrolled 63 children at high risk of DMD and with exercise retardation who were treated in the Pediatrics Department of the First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine between March 2017 and March 2019. Improvements in their movement were observed and compared with those of normal children of the same age, and effective planning and the optimal intervention time for high-risk children were explored, with the aim of effectively improving damaged brain function to reduce the chance of disability, thus improving the quality of life of these children and their families.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/apm-20-1057).
Methods
Study population
All procedures performed in this study were in accordance with the Declaration of Helsinki and was approved by the ethic committee of our hospital. A signed informed consent form was obtained from each child’s parents or guardians.
Between March 2017 and March 2019, 63 children at high risk of DMD were treated in the Department of Pediatrics of the First Affiliated Hospital of Guizhou University of Traditional Chinese Medicine. After enrolment, the children were divided into three intervention groups (IGs) according to their month age: 22 children in IG I (0–3 months), 25 children in IG II (4–6 months), and 16 children in IG III (7–12 months). All children at high risk of brain injury aged between 0–12 months underwent Gesell Infant Development Scale (GESELL) developmental examination by an independent doctor (4,5). Their exercise energy scores were all ≤75 points. Children aged >12 months; or who had central dyskinesia caused by other diseases were excluded from the study. During the same period, 63 healthy age-matched children were enrolled as a control group (CG) and split into CG I, CG II, and CG III, each with the same number of children as the corresponding IG.
Therapy
In the IGs, the prescriptions for Rougan Decoction (6) were mulberry parasite, wolfberry fruit, white peony root, angelica root, and Radix Polygoni multiflori (10 g each as king medicine), with Uncaria chrysanthemum, chrysanthemum, Prunella vulgaris, Yuanshen, and red peony root as subjects medicine, (10 g each), mother-of-pearl, Achyranthes bidentata, Angelica sinensis, Tribulus terrestris, as adjuvant medicine (10 g each), those with spleen deficiency plus Poria, Codonopsis, Campanulaceae, etc., decoction with water, 1 dose/day, taken twice in the morning and evening. At the same time, the children were given Tongdu massages, hand massages, Xunjing massages, and point-pressing massages (4–5 min/time, once a day), and an effort was made to avoid any obvious discomfort for the children. The healthy children did not receive any intervention. A signed informed consent form was obtained from each child’s parents or guardians.
GESELL evaluation
The motor function of each child was evaluated by GESELL both before and three months after the intervention (7). After 3 months, the intervention was considered to be significantly effective if the total athletic energy score had increased by at least ≥15 points; effective if the total athletic energy score had increased by 10 to 15 points; and invalid if the athletic energy score had increased by <10 points.
Statistical analysis
Continuous variables were expressed as the mean ± standard deviation (SD) and compared using an unpaired two-sided Student’s t-test when normal distribution and equal dispersion were confirmed. When the variance was unequal, the Mann-Whitney U test and Wilcoxon signed-rank test were used. Categorical variables were expressed as percentages (%) and compared using χ2 analysis or Fisher’s exact test if necessary. A P value <0.05 was considered statistically significant. All statistical analyses were performed with SPSS (version 22.0 for Windows, SPSS, Inc., Chicago, IL, USA).
Results
Changes of GESELL exercise energy score before and three months after intervention
After 3 months of combined treatment with Rougan Tongdu massage and point-pressing massage, the scores of coarse movement, fine movement, and total motor function of the children in the three IGs were significantly higher than those recorded pre-intervention, and the difference was significant (P<0.05). In IG I, the increase in each motor function score was significantly higher than those in the other two IGs (P<0.05). No intervention was given to the children in the three CGs, and no significant difference was observed in the coarse motor, fine motor, and total motor function scores during the same time period (P>0.05). Before and after treatment, the coarse movement, fine movement, and total motor function scores of the children in IG I and CG I, IC II and CG II, and IG III and CG III were compared respectively (all P<0.05). See Table 1 for details.
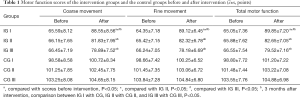
Full table
Comparison of clinical effectiveness
The total effective (significantly effective and effective) rates of the three IGs were 95.5%, 80.0%, and 62.6%, respectively. The total effective rate in IG I was better than the other two groups (P<0.05), as shown in Table 2.
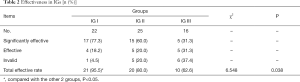
Full table
Discussion
DMD can be caused by three types of factors: (I) innate factors: the mother’s mental development is dysplasia caused by environmental or psychological factors during pregnancy; (II) acquired factors: intelligence damage caused by various diseases or other causes soon after birth; (III) trauma factors: head damage caused by obstetrical instruments during delivery that affects the child's intellectual development (8). Children with DMD mainly present with motor impairment or retardation but, after effective treatment, various functions can be recovered to a normal level. However, for children with cerebral palsy and mental retardation, early clinical diagnosis, treatment, and rehabilitation is recommended (8,9).
In traditional Chinese medicine (TCM), movement retardation belongs to the category of “five delays” and “five softnesses”. It attributes the main cause of the disease to fetal loss, congenital insufficiency, acquired infertility, deficiency of yin and yang, blood and liver and kidney loss (TCM definition, not anatomical). It is closely related to the liver and kidneys, governing veins, spleen and stomach, and bladder meridian (9,10). The liver is the hiding of Fengmu (which refers to wind and tree). Children often have large range of “liver”, which can be easily disturbed by “evil”. The wind is good and always changes, and the wind evil is blocked in the meridians, making the veins impassable and the qi and blood become disharmonized and convulsive. The treatment is based on softening and calming the “liver”, promoting blood circulation, and removing wind (6,11,12). The viscera of children is neither complete nor strong, and the use of medicine should be minimized. In this study, Rougan Xifeng Recipe, Uncaria, Prunella, Red Peony, Chrysanthemum, and Yuanshen were used to calm the liver, relieve spasms, and disseminate the liver heat and wind. The liver is just visceral and cannot be reconciled unless it is soft and moist. Red peony has the power to soften the liver and relieve urgency. Mulberry parasite, wolfberry fruit, angelica, and Shouwu promote blood circulation, nourishing the wind and the liver and kidney. Liver winds are reasons to, cause liver regulation, impair the ventilation function of the entire body and cause sputum to increase. Poria, Codonopsis, and Bellflower can strengthen the spleen and reduce phlegm (6). Mother-of-pearl has a calming effect on the mind, the liver, and yang, while achyranthes can nourish the yin and kidney. The combination of various medicines has the effect of calming and softening the liver, promoting blood circulation and removing wind, and strengthening the spleen and kidney.
From the perspective of differentiating between the syndromes of traditional Chinese medicine, the combined massage technique of Tongdu massage, manipulation massage, meridian massage, and point pressing can play a role in the overall regulation and nourishment of the liver and kidney, and its relaxation technique can effectively relieve spasm and improve the degree of articulation in the joints. It can be used to activate the qi and then to relieve spasm, thereby promoting blood circulation, improving the supply of blood and nutrition to the child’s limbs and spine, helping to restore their motor function (13-18). At the same time, gentle kneading, pushing, pressing, rolling, touching, and other techniques can alleviate the feelings of nervousness and vulnerability felt by children during treatment, meaning there is higher parental acceptance and a better treatment effect is achieved (8,9). From the perspective of modern medicine, massage and acupuncture can promote joint blood vessel expansion and increase local blood circulation. Massage can increase skin temperature, muscle tension and elasticity, and promote blood circulation around joints, thus promoting ligament elasticity and eliminating joint contracture spasticity In addition, massage and acupuncture can strengthen skeletal muscle protein synthesis, reduce the proliferation of connective tissue between muscle fibers, effectively regulate the function of joints in the musculary system, promote the recovery of muscle morphology and structure, improve patient’s motor function, improve the abnormal posture of children with DMD, and promote their movement development (15-18).
Wang Chunhua and other investigators found that early rehabilitation and early combined massage treatment could significantly improve the motor function of children at high risk of DMD (8). In this study, after 3 months of treatment with acupoint therapy with Rougan Tongdu massage, the rough action scores of the children in the three IGs (IG I, IG II, and IG III) were 88.55±8.56, 81.83±7.95, and 78.89±7.52, respectively; the elaborate action scores were 89.12±6.45, 82.32±6.78, and 78.18±6.69, respectively; and the total motor function scores were 89.85±7.20, 82.65±7.05, and 79.52±7.16, respectively. The scores for each group were significantly higher than those before the intervention (P<0.05). The increases in coarse movement, fine movement, and total motor energy scores in IG I were significantly higher than those in the other two IGs (P<0.05). This is consistent with the findings of Wang Chunhua, who showed that the intervention of Rougan Tongdu massage acupoint therapy can significantly improve coarse movement, fine movement, and total motor performance. While a gap still remained in relation to the healthy group, these results showed that in children at high risk of DMD, the earlier the intervention, the better the improvement was. In terms of clinical efficacy, the total effective rate was 95.5% in IG I, 80.0% in IG II, and 62.6% in IG III. The clinical effect of IG I was more significant than that of the other two groups (P<0.05). In a study of the effect of early rehabilitation intervention on the prognosis of preterm infants with high risk factors, Yang et al. pointed out that the treatment efficiency in children younger than 3 months is significantly better than that of children over the age of 6 months, and this study produced similar results (19). Infancy is a key stage in children’s neuromotor development, and so neuroplasticity should be an important treatment direction for children. As well as having only few adverse effects, traditional Chinese medicine can maximize the recovery of damaged brain function through benign stimulation (20). It is of great significance for the treatment of children who are at high risk of DMD and is suitable for clinical application. Otherwise, the sample size of this study is relatively small.
Conclusions
In summary, early Rougan Tongdu massage therapy has a positive clinical effect in children who are at high risk of DMD. It is worth further promotion and application.
Acknowledgments
Funding: Guizhou Scientific Plan, (2016)-7522.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/apm-20-1057
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-1057
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at Available at http://dx.doi.org/10.21037/apm-20-1057). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the Declaration of Helsinki and was approved by the ethic committee of our hospital. A signed informed consent form was obtained from each child’s parents or guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ma L, Zhang Y, Yu H, et al. Follow-up study of early intervention on high-risk neonates intelligence development. Maternal and Child Health Care of China 2014;29:560-2.
- Yang G, Liu Y, Liu Y. Clinical Observation on Early Intervention of High-risk Infant Development by Acupoint Massage and Touching. Chin J Inf Tradit Chin Med 2014;21:100-1.
- Xie L, Wang R, Wu X, et al. Influence of early intervention on motor development prognosis of infants at high risk of cerebral palsy. Chinese Journal of Child Health Care 2014;22:426-9.
- Wang D, Zhong Q, Tang X, et al. Effect of acupuncture and massage therapy on balance function and fear of falling in school-age children with cerebral palsy. Chinese Journal of Rehabilitation Medicine 2017;32:440-2.
- Children's Rehabilitation Professional Committee of Chinese Society of Rehabilitation Medicine. 2015 China Rehabilitation Guideline for Cerebral Palsy: Part 10. Chinese Journal of Rehabilitation Medicine 2016;31:494-8.
- Zhang L, Liu K, Pan L. Professor An Xiaoxian's diagnosis and treatment of pediatric difficult cases. Global Traditional Chinese Medicine 2013;6:932-3.
- Hu S, Huang R, Peng G, et al. Application Analysis of Alberta Infant Exercise Scale in Early Intervention of High Risk Children. Chinese Journal of Rehabilitation Medicine 2015;30:157-9.
- Wang G, Wang C, Feng J. Clinical observation on the value of early intervention of traditional Chinese medical massage on high-risk infants. Chinese Journal of Child Health Care 2018;26:459-61.
- Wang G, Feng J. Clinical Observation on Early Intervention in Motor Developmental Delay High-risk Children by the Massage Therapy. Systems Medicine 2017;2:121-3.
- Jia X, Li T, Liu J. Effects of early intervention of neurodevelopmental therapy on the movement and cognitive development of high-risk preterm infants. Maternal and Child Health Care of China 2014;29:4767-9.
- Zhao X, Zhang Z, Li J. Effect of Warming Acupuncture Combined with Rougan Xifeng Decoction on Hemorheology and Limb Function in Patients with Ischemic Stroke. Journal of Liaoning University of TCM 2019;21:219-21.
- Deng L. Clinical Application of Rougan Method in Pediatrics. Hebei J TCM 2015;37:26264.
- Chen D, Zhong N, Huang H, et al. Effect of motor development massage and neural development approach on the children with cerebral palsy. Chin J Rehabil Theory Pract 2015;21:85-7.
- Miao Z, Zhou Y. Observation on clinical curative effect of Chinese medicine massage on children with motor retardation. Latest Medical Information Digest 2019;19:187-8.
- Hong W, Jia J, He Y, et al. Effects of acupoint massage and exercise therapy on muscle tone and motor function in patients with spastic cerebral palsy. Lishizhen Medicine and Materia Medica Research 2018;29:1903-5.
- Ma MM, Liu ZH, Zhao Y, et al. Clinical observation on treatment of spastic cerebral palsy with tuina plus music therapy. Journal of Acupuncture and Tuina Science 2009;7:213-7. [Crossref]
- Zhang L. Efficacy of acupuncture and massage plus the Tiaozhi therapy on muscular tension of children with spastic cerebral palsy. Clinical Journal of Chinese Medicine 2017;9:36-8.
- Wu S, Yun G, Wu L, et al. Research of Correction Technique Combined with Massage for Motor Dysfunction in Children with Spastic Cerebral Palsy. Journal of Clinical Acupuncture and Moxibustion 2017;33:45-8.
- Yang C, Xu P. Prognosis research of early rehabilitation on premature infant with risk factors. Chinese Journal of Child Health Care 2014;22:735-8.
- Zou L, Lin X, Chen W, et al. The effect of early intervention based on NICU environment on the neurodevelopmental outcome of premature high-risk infants. Chinese Journal of Rehabilitation 2017;32:136-7.


