
Correlation between common postoperative complications of prolonged bed rest and quality of life in hospitalized elderly hip fracture patients
Introduction
Hip fracture, which mainly includes femoral neck fractures and intertrochanteric fractures, is a common problem encountered by older people, especially postmenopausal women (1). Hip fracture not only seriously impacts the physical and mental health of patients but also places a heavy burden on families and society. It has therefore become a global medical problem (2,3). At present, surgery is the preferred treatment for hip fractures (4). However, declined physical function and decreased organ function are common in older patients and are often accompanied by various chronic diseases and poor compensatory ability. The reduced postoperative mobility resulting from these conditions predisposes elderly patients with hip fractures to a variety of complications associated with prolonged bed rest including acute cerebral infarction, pressure injury, deep vein thrombosis of the lower limbs, and lung and urinary tract infections (5-7). Deep vein thrombosis of the lower limbs and pulmonary infections are risk factors for adverse outcomes in elderly patients with hip fractures (8,9). There were many studies on postoperative complications of elderly hip fracture patients, but they only studied what complications occurred. Few studies to date have investigated the relationship between the complications commonly associated with prolonged bed rest after hip fracture surgery and the outcomes of discharged patients. This study was designed to explore the correlation between common postoperative complications of prolonged bed rest and quality of life (QoL) in hospitalized elderly hip fracture patients, in an attempt to inform the development of early and tailored assessment protocols and interventions.
Methods
Subjects
A total of 502 elderly hip fracture patients who underwent surgical treatment at the Affiliated Hospital of Jiangnan University between December 2014 and October 2019 were enrolled in this study. Patients meeting the following criteria were included in the study: (I) 65 years old or above; (II) with a first diagnosis of femoral neck fracture or intertrochanteric fracture; (III) with a fresh fracture within 3 weeks; (IV) with complete medical records; (V) without an acute infectious disease before injury; and (VI) provided signed informed consent. Patients were excluded from the study if they met any of the following criteria: (I) with pathological fractures; (II) with systemic composite injury; (III) with an acute infectious disease before injury; (IV) with old fractures; (V) with coagulation disorders such as old thrombosis and hemophilia; and (VI) with malignant tumors. This study received approval from the ethics committee of our hospital (Ethics Approval Number: [(2014) KY052]) and was conducted in accordance with the Declaration of Helsinki. Signed informed consent was obtained from all subjects.
Survey methods
Survey tools
Survey on the basic information of elderly patients with hip fracture
The survey was based around a self-designed questionnaire, which covered the patient’s age, gender, education level, type of health insurance, days of bed rest, days of hospital stay, any common complications of prolonged bed rest experienced, and diagnosis at discharge. The severity of a patient’s condition was also assessed, based on the Charlson Comorbidity Index (CCI) score (10).
Post-discharge QoL assessment form
The patients’ QoL was assessed by using the Chinese version of the EuroQoL 5-Dimension (EQ-5D) (11). EQ-5D includes five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is assessed based on three possible levels: none, mild to moderate, and severe. The Chinese version of EQ-5D has been demonstrated to have a Cronbach’s α coefficient of 0.624, a Spearman’s rank correlation coefficient of 0.592–0.699, and structural validity of 0.685, indicating that it has good reliability and efficiency (11). The scale has been widely used in clinical settings (6,12).
Data collection
Each participating department selected 2–3 nurses (with an educational background of college or above and with work experience of at least 3 years) as investigators, who received uniform training before the survey was initiated. After the patients were enrolled, their basic information such as sex, age, and educational background were recorded, and complications, treatment, and nursing information from during the hospitalization underwent timely assessment. The patients were followed up by telephone on the 90th day of enrolment after discharge or transfer. During the follow-up, the patients’ QoL was investigated by recording the score of each entry in the EQ-5D scale. Quality control measures were performed for medical records (20% of the cases were selected at random to double-check the consistency between the information entered and the original medical records), the field survey (each of the participating department were visited to check whether the data collected and entered were consistent with the patient’s condition), and background data (data submitted by investigators during data collection were periodically reviewed) to ensure the authenticity, reliability, and integrity of the research data.
Statistical analyses
The results were analyzed with SAS 8.12 software. The measurement data were described as mean ± standard deviation and compared by independent two-sample t-test. The count data were presented with rates and percentages and compared using chi-square test and rank sum test. The influence from various confounding factors was ruled out with multivariate logistic regression analysis. A P value of <0.05 represented statistically significant difference.
Results
Basic information of the hospitalized elderly patients with hip fracture
Of the 502 older hip fracture patients included in the study, 281 were female (55.98%) and 221 were male (44.02%). The ages of 287 (65.17%) patients ranged between 65 and 80 years old, and 215 (42.83%) patients were >80 years old. The patients’ educational background included primary school or below in 301 cases (59.96%), middle school/high school in 150 cases (29.88%), and junior college or above in 51 cases (10.16%). In 93 cases (18.53%), the patients had self-funded their treatment, while in the remaining 409 cases (81.47%), the patients’ treatment was covered by medical insurances or public health services. The duration of bed rest was 1–3 days in 110 patients (21.91%), 4–7 days in 145 patients (28.88%), and 8 days and above in 247 patients (49.20%). The length of hospital stay ranged from 1 to 7 days in 74 patients (14.74%), 8–14 days in 212 patients (42.23%), and 15 days and above in 216 patients (43.03%). Femoral neck fractures and intertrochanteric fractures accounted for 298 (59.36%) and 204 (40.64%) of the hip fracture cases, respectively. The CCI score was 0–2 points in 79 cases (15.74%), 3–4 points in 185 cases (36.85%), and 5 points and above in 238 cases (47.41%).
Incidences of complications caused by prolonged bed rest
During hospitalization, 98 of the 502 patients (19.52%) experienced at least 1 common complication; these included acute cerebral infarction (n=15, 2.99%), pressure injury (n=25, 4.98%), deep vein thrombosis of the lower limbs (n=14, 2.79%), pulmonary infections (n=84, 16.73%), and urinary tract infections (n=30, 5.98%). The age, hospitalization billing type, days of bed rest, days of hospital stay, and CCI score significantly differed between patients who experienced the common post-operative complications of prolonged bed rest and those who experienced none of these complications (Table 1).

Full table
Correlation between common postoperative complications of prolonged bed rest and QoL in hospitalized elderly hip fracture patients
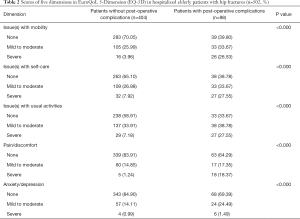
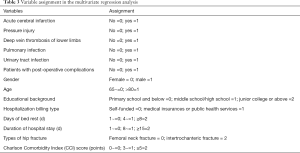
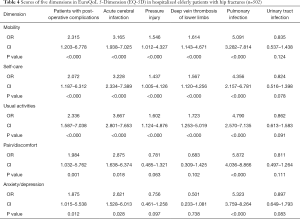
Univariate analysis showed that the score of each dimension in EQ-5D was significantly lower in patients with post-operative complications than in those without post-operative complications after discharge. In issue(s) with mobility, there were 105 (25.99%) patients had mild to moderate mobility impairment and 16 (3.96%) patients had severe in the group without complications, while there were 33 (33.67%) patients with mild to moderate mobility impairment and 26 (26.53%) patients had severe in the complication group (P<0.000). In issue(s) with self-care, there were 109 (26.98%) patients had mild to moderate self-care difficulties and 32 (7.92%) patients had severe in the group without complications, while there were 33 (33.67%) patients with mild to moderate self-care difficulties and 27 (27.55%) patients with severe in the complication group (P<0.000). In issue(s) with usual activities, there were 137 (33.91%) patients had mild to moderate difficulties in usual activities and 29 (7.18%) patients had severe in the group without complications, while there were 38 (38.78%) patients with mild to moderate difficulties in usual activities and 27 (27.55%) patients had severe in the complication group (P<0.000). In issue(s) with pain/discomfort, there were 60 (14.85%) patients had mild to moderate pain/discomfort and 5 (1.24%) patients had severe in the group without complications, while there were 17 (17.35%) patients with mild to moderate pain/discomfort and 18 (18.37%) patients had severe in the complication group (P<0.000). In issue(s) with anxiety/depression, there were 57 (14.11%) patients had mild to moderate anxiety/depression and 4 (0.99%) patients had severe in the group without complications, while there were 24 (24.49%) patients with mild to moderate anxiety/depression and 6 (1.49%) patients had severe in the complication group (P<0.000) (Table 2). Multivariate regression analysis was then performed with the scores of each dimension of EQ-5D as the dependent variables and the factors including age, gender, education background, days of bed rest, days of hospital stay, and post-operative complications as independent variables. The results of variable assignment in the multivariate regression analysis are shown in Table 3. It Acute cerebral infarction (mobility: OR =3.165, CI: 1.938–7.025, P<0.000; self-care: OR=3.228, CI: 2.334–7.389, P<0.000; usual activities: OR =3.667, CI: 2.801–7.653, P<0.000; pain/discomfort: OR =2.875, CI: 1.638–6.374, P=0.018, and anxiety/depression: OR =2.621, CI: 1.528–6.013, P=0.028), pressure injury (mobility: OR =1.546, CI: 1.012–4.327, P<0.000; self-care: OR =1.437, CI: 1.005–4.126, P<0.000; usual activities: OR =1.602, CI: 1.124–4.876, P<0.000; pain/discomfort: OR =0.781, CI: 0.485–1.321, P=0.063, and anxiety/depression: OR =0.756, CI: 0.461–1.258, P=0.097), deep vein thrombosis of the lower limbs (mobility: OR =1.614, CI: 1.143–4.671, P<0.000; self-care: OR =1.567, CI: 1.120–4.256, P<0.000; usual activities: OR =1.723, CI: 1.253–5.019, P<0.000; pain/discomfort: OR =0.683, CI: 0.309–1.425, P=0.102, and anxiety/depression: OR =0.501, CI: 0.233–1.081, P=0.738), and pulmonary infections (mobility: OR =5.091, CI: 3.282–7.814, P<0.000; self-care: OR =4.356, CI: 2.157–6.781, P<0.000; usual activities: OR =4.790, CI: 2.570–7.135, P<0.000; pain/discomfort: OR =5.872, CI: 4.036–8.866, P<0.000, and anxiety/depression: OR =5.323, CI: 3.759–8.264, P<0.000) were found to potentially affect QoL for older patients with hip fractures after discharge, while urinary tract infection (mobility: OR =0.835, CI: 0.537–1.438, P=0.124; self-care: OR =0.824, CI: 0.516–1.398, P=0.078; usual activities: OR =0.862, CI: 0.613–1.583, P=0.091; pain/discomfort: OR =0.811, CI: 0.497–1.264, P=0.111, and anxiety/depression: OR =0.897, CI: 0.649–1.793, P=0.083) had no effect (Table 4).
Full table
Full table
Full table
Discussion
The incidences of postoperative complications of prolonged bed rest are high in older patients with hip fractures
Surgical treatment can promote fracture healing and shorten the disease course for elderly hip fracture patients; however, due to limited mobility in the postoperative stage, patients are required to stay in bed for a long period of time, and consequently, the risks of various complications are remarkably increased (13). Ryan et al. (14) found that a longer period of bed rest before surgery was associated with longer hospital stay and higher risk of pressure injury, deep vein thrombosis of the lower limbs, and lung infections. In our current study, the incidence of post-operative complications of prolonged bed rest was high in hospitalized elderly hip fracture patients (19.52%), especially the incidence of pulmonary infection (16.73%), which was similar to the finding of Del Toro et al. (15). Lung infections in older patients with hip fractures may be attributed to a variety of factors including multiple underlying diseases, low immunity, impaired cough reflex, decreased sputum for expelling, poor resistance to pathogenic bacteria, and aspiration of gastric contents (16-18). The occurrence of deep vein thrombosis in the lower limbs is related to venous vessel wall impairment and hypercoagulation (19). In serious cases, the thrombi may break off and travel through the bloodstream to the lungs, resulting in a highly fatal pulmonary embolism. One previous study reported that the incidence of deep vein thrombosis in the lower extremities was as high as 50% in hip fracture patients (9). In the current study, the incidence of deep vein thrombosis in the lower extremities was 2.79%, which was strikingly lower than that reported by Geerts et al., and may be explained by differences in the sample size, treatment, and research population. Postoperative pressure injury in elderly hip fracture patients may be related to limited limb mobility, pain, and psychological factors. Studies have shown that the incidence of perioperative pressure injury in patients with hip fractures ranged from 10.0% to 22.7% (20,21), which was significantly higher than the 4.98% observed in our current study. Reasons for this difference may be attributed to differences in the quality of care in various hospitals and the research population. Cerebral infarction and urinary tract infection are two other bed rest-associated complications commonly experienced by elderly patients with hip fractures. Postoperative stress may be the cause of acute cerebral infarction. Indwelling catheter can cause damage to the urethral mucosa. In addition, the patient’s postoperative immune function declines and the urethral mucosa’s defense ability decreases, which may be the cause of urinary tract infection. In our current study the incidences of cerebral infarction and urinary tract infection were 2.99% and 5.98%, respectively. Therefore, complications from being bedridden are quite common in elderly patients with hip fractures.
In our current study, a large proportion of elderly patients with hip fracture were also shown to experience problems with mobility, self-care, and performing usual activities, which was consistent with previous research (22). The incidence of postoperative anxiety or depression was 18.13% in elderly patients with hip fracture, which suggests that hip fracture patients may encounter psychological problems in addition to the more visible severe physical dysfunction. Zhang et al. (6) implemented early activity interventions in older patients with hip fractures; these effectively shortened the length of hospital stay and improved the QoL, suggesting clinical nursing staff should promptly screen high-risk patients and take comprehensive nursing measures to ensure early intervention with their activities.
Hospitalized elderly hip fracture patients experiencing common complications of prolonged bed rest had lower QoL after discharge
Univariate analysis showed that the score of each dimension in EQ-5D was significantly lower in patients who had post-operative complications than in those who had no post-operative complications after discharge. For older hip fracture patients who experience complications such as acute cerebral infarction, pressure injury, and/or lung infection, the same problem(s) may persist after discharge, resulting in a continuous adverse effect on the patient’s health status. As shown in our current study, elderly patients with hip fractures who had suffered from complications of prolonged bed rest had longer bed rest, longer hospital stays, and more comorbidities; accordingly, they were more likely to have problems in daily activities and self-care and thus have a lower QoL.
Four common complications of prolonged bed rest (acute cerebral infarction, pressure injury, deep vein thrombosis of the lower limbs, and pulmonary infections) were identified by multiple regression analysis to potentially affect the QoL of elderly patients with hip fractures after discharge. Among the patients who experienced these complications, those with pulmonary infections scored lowest across all dimensions of EQ-5D. Previous studies (5,7) have shown that pulmonary infection is an independent risk factor of dysfunction and death after discharge. Our current analysis also revealed that all of the dimensions of QoL were negatively affected in patients with lung infections. In fact, patients with lung infections often have more severe conditions; lung infections can impair the immune system, leading to a decline in the physiological function of the body; and finally, lung infections can increase the physical and mental burden on patients. As a result, the QoL of these patients declines. Some foreign studies (23,24) have demonstrated that acute cerebral infarction, pressure injury, and deep vein thrombosis in the lower limbs were the risk factors for death in elderly patients with hip fractures. Medical personnel play a crucial role in preventing complications such as pulmonary infection, pressure injury, acute cerebral infarction, and deep vein thrombosis of the lower limbs. They should make effective interventions to reduce the incidence of complications for older patients with hip fractures. After the operation, instruct the patients to carry out cough training, lung function exercise and lower limb function exercise, assist the patient to eat in the correct posture, get out of bed in a special posture and correct the bad posture, and perform functional exercise as soon as possible, which may prevent the occurrence of bed-complications.
Conclusions
Elderly hip fracture patients who experience common complications associated with prolonged bed rest have poor QoL after discharge. Therefore, medical personnel should take effective measures to prevent and treat these complications, such as deep vein thrombosis of the lower limbs and pulmonary infections, during the patients’ stay at hospital. By doing this, the recovery of these patients’ physical and mental health can be effectively promoted and the impact of the condition on their QoL can be reduced.
Acknowledgments
Funding: This work was supported by the Wuxi Medical and Public Health Technology Innovation and Application Project, Jiangsu Province, China, N 20192025 (to XSW) and the Public Health Center at Jiangnan University of China, No. JUPH201808 (to XSW). We thank these funds and the Affiliated Hospital of Jiangnan University for providing experimental equipment support for the study.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/apm-20-891
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm-20-891). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was performed in compliance with the ethical principles of the Declaration of Helsinki and was approved by the Ethics Committee of the Affiliated Hospital of Jiangnan University [(2014)KY052]. All subjects agreed and signed informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tucker NJ, Kamath AF. Comparing total hip arthroplasty and hemiarthroplasty in the treatment of hip fracture. Ann Transl Med 2019;7:S259. [Crossref] [PubMed]
- Baidwan NK, Naranje SM. Epidemiology and recent trends of geriatric fractures presenting to the emergency department for United States population from year 2004-2014. Public Health 2017;142:64-9. [Crossref] [PubMed]
- Quinn RH, Murray JN, et al. The american academy of orthopaedic surgeons appropriate use criteria for management of hip fractures in the elderly. J Bone Joint Surg Am 2016;98:1222-5. [Crossref] [PubMed]
- Le Manach Y, Collins G, Bhandari M, et al. Outcomes after hip fracture surgery compared with elective total hip replacement. JAMA 2015;314:1159-66. [Crossref] [PubMed]
- Chatterton BD, Moores TS, Ahmad S, et al. Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J 2015;97-B:246-51. [Crossref] [PubMed]
- Zhang Y, Wang TT, Che L, et al. Effects of hip fractures to the quality of life in old patients. Journal of Practical Orthopaedics 2019;54:1615-20.
- Ryan DJ, Yoshihara H, Yoneoka D, et al. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma 2015;29:343-8. [Crossref] [PubMed]
- Roche JJ, Wenn RT, Sahota O, et al. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 2005;331:1374. [Crossref] [PubMed]
- Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 2008;133:381S‐453S.
- Thygesen SK, Christiansen CF, Christensen S, et al. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish national registry of patients. BMC Med Res Methodol 2011;11:83. [Crossref] [PubMed]
- Xing YB, Ma AX. Study on reliability and validity of Chinese version of EQ-5D-5L. Shanghai Medical & Pharmaceutical Journal 2013;(9):40-3.
- Lu WS, Huang SL, Yang JF, et al. Convergent validity and responsiveness of the EQ-5D utility weights for stroke survivors. J Rehabil Med 2016;48:346-51. [Crossref] [PubMed]
- Bekelis K, Desai A, Bakhoum SF, et al. A predictive model of complications after spine surgery: the National Surgical Quality Improvement Program (NSQIP) 2005-2010. Spine J 2014;14:1247-55. [Crossref] [PubMed]
- Ryan DJ, Yoshihara H, Yoneoka D, et al. Delay in hip fracture surgery: an analysis of patient-specific and hospital-specific risk factors. J Orthop Trauma 2015;29:343-8. [Crossref] [PubMed]
- del Toro MD, Nieto I, Guerrero F, et al. Are hip hemiarthroplasty and total hip arthroplasty infections different entities? The importance of hip fractures. Eur J Clin Microbiol Infect Dis 2014;33:1439-48. [Crossref] [PubMed]
- Morris BJ, Unger RZ, Archer KR, et al. Risk factors of infection after ORIF of bicondylar tibial plateau fractures. J Orthop Trauma 2013;27:e196-e200. [Crossref] [PubMed]
- Sun Y, Wang H, Tang Y, et al. Incidence and risk factors for surgical site infection after open reduction and internal fixation of ankle fracture. Medicine 2018;97:e9901. [Crossref] [PubMed]
- Korim MT, Payne R, Bhatia M. A case-control study of surgical site infection following operative fixation of fractures of the ankle in a large U.K. trauma unit. Bone Joint J 2014;96-B:636-40. [Crossref] [PubMed]
- Choi WS, Lee HJ, Kim DY, et al. Does osteoporosis have a negative effect on the functional outcome of an osteoporotic distal radial fracture treated with a volar locking plate? Bone Joint J 2015;97-B:229-34. [Crossref] [PubMed]
- Chiari P, Forni C, Guberti M, Gazineo D, Ronzoni S, D'Alessandro F. Predictive Factors for Pressure Ulcers in an Older Adult Population Hospitalized for Hip Fractures: A Prognostic Cohort Study. PLoS One 2017;12:e0169909. [Crossref] [PubMed]
- Larsson G, Holgers KM. Fast-track care for patients with suspected hip fracture. Injury 2011;42:1257-61. [Crossref] [PubMed]
- Li HD, Chen Y, Yang JH, et al. Effects of hip fractures to the quality of life in old patients. Journal of Practical Orthopaedics 2018;24:799-801.
- Castronuovo E, Pezzotti P, Franzo A, et al. Early and late mortality in elderly patients after hip fracture: a cohort study using administrative health databases in the Lazio region, Italy. BMC Geriatr 2011;11:37. [Crossref] [PubMed]
- Luksameearunothai K, Sa-Ngasoongsong P, Kulachote N, et al. Usefulness of clinical predictors for preoperative screening of deep vein thrombosis in hip fractures. BMC Musculoskelet Disord 2017;18:208. [Crossref] [PubMed]


