Personal instruction for patients before colonoscopies could improve bowel preparation quality and increase detection of colorectal adenomas
Introduction
Performing a colonoscopy is vital for the diagnosis and treatment of colon diseases. This importance is due to the physiological function of the colon, and bowel preparation quality dramatically impacts the effectiveness and safety of colonoscopy (1,2). While in the clinical practice, when we perform a colonoscopy for patients who complete bowel preparation according to written instructions at home, the quality is adequate. However, for patients who do not adequately prepare or take the bowel preparation drug as required, the quality is reduced (3), which affects the operation and observation; often, patients need to be reexamined after inadequate bowel preparation (4). Bowel preparation quality directly affects the detection rate of colorectal diseases. Colorectal adenomas are precancerous lesions, increasing the adenoma detection rate, and providing effective treatment can reduce the progression risk of colorectal cancer (5). This study aims to see whether face-to-face education by medical staff before colonoscopy can improve the quality of bowel preparation and increase the detection of colorectal adenomas.
Methods
Subjects
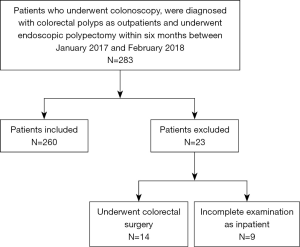
Consecutive adult patients who were diagnosed with colorectal polyps by colonoscopy as outpatients and underwent endoscopic polypectomy within six months between January 2017 and February 2018 were retrospectively included in the study. The study protocol was approved by the Ethics Committee of Capital Medical University affiliated Beijing Shijitan Hospital. All patients signed written informed consent forms before colonoscopy. The exclusion criteria were as follows: (I) patients with incomplete colon examinations not related to bowel preparation at the first colonoscopy as outpatients; (II) patients with incomplete examinations as inpatients; (III) patients who underwent colorectal surgery before the first colonoscopy as outpatients.
Study protocol
Bowel preparation instructions were given in writing for outpatients before colonoscopy. The patients performed the bowel preparation at home by themselves according to these written instructions, which included a diet adjustment and the administration of bowel preparation drugs. The outpatients who were detected to have colorectal polyps and underwent endoscopic polypectomy inpatient within six months were enrolled in our study. When they were admitted to the hospital, they were given personal instructions about bowel preparation before colonoscopy by medical staff in a face-to-face meeting. The pictures of the bowel preparation results were attached to the wall of the bathroom in the ward, which aided patients in evaluating the outcome of the bowel preparation. Doctors confirmed the result of the bowel preparation before the colonoscopy, recommended more bowel preparation according to the results if necessary.
Bowel preparation methods (6)
A low-fiber diet (7,8) one day before colonoscopy and fasting on the day of colonoscopy were required. Two thousand milliliters of a bowel preparation drug [polyethylene glycol electrolyte dispersion (64 g + 1,000 mL water) ×4] was taken between 7 p.m. and 9 p.m. on the night before colonoscopy, and another 2,000 mL was taken between 8 a.m. and 10 a.m. on the day of the colonoscopy. A total of 30 mL of Simethicone Emulsion was taken 3 hours before the examination.
Observation index
Colonoscopies as out- and in-patients are compared in the same group of patients. The time to reach the ileocecal region was recorded, and the bowel preparation was evaluated [the Boston Bowel Preparation Scale (BBPS) and bubble scores were used]. The number, size, location, morphology, and pathology of the colorectal polyps were examined.
The quality of bowel preparation was evaluated by BBPS (9). The bubble scores were assigned as follows: 0= no or few bubbles; 1= bubbles covering at least half of the diameter of the colorectal cavity; and 2= bubbles covering the whole colorectal cavity.
Statistical analyses
Data were entered into SPSS (Statistical Product and Service Solutions) 21.0 for analysis (IBM, Armonk, NY, USA). Time to reach the ileocecal region and bowel preparation quality in the two colonoscopies were analyzed by paired-samples t-tests or Wilcoxon signed-rank tests according to the distribution of data. Missed colorectal adenoma diagnoses were analyzed by multivariate logistic regression considering the quality of bowel preparation, morphology, diameter, and location of the colorectal adenoma. Statistical significance was as accepted when P<0.05.
Results
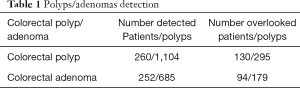
Patient baseline characteristics and polyp detection (Table 1): of the 283 consecutive adult patients who underwent a colonoscopy as outpatients, were diagnosed with colorectal polyps and underwent endoscopic polypectomy within six months, 260 patients were eligible for inclusion (Figure 1). Twenty-three patients were excluded; 14 patients underwent colorectal surgery, and nine patients had incomplete examinations as inpatients. The study population included 169 males and 91 females, with median [IQR] age 63 [56, 68] years old. A total of 1,104 colorectal polyps were found. A total of 252 patients were diagnosed with colorectal adenomas, and 685 polyps were identified as colorectal adenomas. A total of 130 patients had 295 polyps overlooked in the first colonoscopy, and 94 patients had 179 adenomas overlooked.
Full table
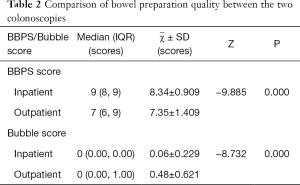
Comparison of bowel preparation quality between the two colonoscopies (Table 2): six of the 260 outpatients were excluded because of failure reaching the ileocecal region in the first colonoscopy due to poor bowel preparation. A total of 254 patients for whom the ileocecal region could be reached in both colonoscopies were included in the statistical analysis. Median [IQR] BBPS score was 9 [8, 9] during inpatient, and 7 [6, 9] during outpatient. In the second colonoscopy, the BBPS scores of 141 patients were higher than those in the first colonoscopy, the BBPS scores of 16 patients were lower than those in the first colonoscopy, and the BBPS scores of 97 patients were equal to those in the first colonoscopy. The difference was statistically significant, with a P value of 0.000. Regarding bubble scores, median (IQR) Bubble Score was 0 (0.00, 0.00) during inpatient, and 0 (0.00, 1.00) during outpatient, in the second colonoscopy, the bubble scores of 98 patients were lower than those in the first outpatient colonoscopy, the bubble scores of only five patients were higher than those in the first outpatient colonoscopy, and the bubble scores of 151 patients were equal to those in the first outpatient colonoscopy. The difference was statistically significant (P value was 0.000).
Full table
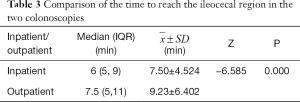
Comparison of the time to reach the ileocecal region in the two colonoscopies (Table 3): six of the 260 outpatients were excluded because of failure reaching the ileocecal region in the first colonoscopy due to poor bowel preparation. The rate of reaching the ileocecal region was 98.07% in the first colonoscopy and 100% in the second colonoscopy. Regarding the time to reach the ileocecal region in the two colonoscopies, the median [IQR] time to reach the ileocecal region was 6 [5, 9] min during inpatient and 7.5 [5, 11] min during outpatient. One hundred sixteen patients had a shorter second colonoscopy, 29 patients had a longer second colonoscopy, and 119 patients had the same time for the two colonoscopies. The difference was statistically significant (P value was 0.000).
Full table
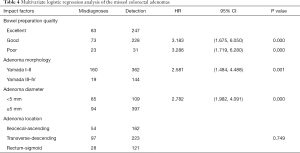
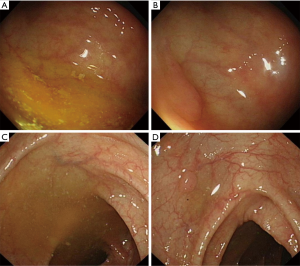
Multivariate logistic regression analysis of the missed colorectal adenomas (Table 4): multivariate logistic regression was used to analyze the factors, including bowel preparation quality, diameter, morphology, and location of colorectal adenoma, associated with missed colorectal adenoma diagnoses. The results suggested that the bowel preparation quality affected the detection of colorectal adenomas. The missed diagnosis rates of colorectal adenomas in patients with excellent and poor bowel preparations were 3.183 and 3.286 times higher, respectively than those in patients with excellent bowel preparation, and the P value was 0.000. Figure 2 shows that adenomas were missed in colonoscopy with inadequate bowel preparation. The morphology and diameter of the colorectal adenomas also affected their detection. The missed diagnosis rate of adenomas with Yamada type I–II morphology was 2.581 times higher than that of adenomas with Yamada type III–IV morphology, and the P value was 0.001. The missed diagnosis rate of adenomas with diameters less than 5 mm was 2.782 times higher than that of adenomas with diameters greater than 5 mm, and the P value was 0.000. The missed diagnosis rate of colorectal adenomas was not related to a location within the colon.
Full table
Discussion
A colonoscopy is a gold standard for diagnosing colon diseases and plays a vital role in screening for colon cancer. The detection and removal of colorectal adenomas by colonoscopy can significantly reduce the risk of colon cancer.
The quality of bowel preparation directly determines the effectiveness of colonoscopy. Inadequate bowel preparation not only reduces the detection rate of adenomas and the rate of reaching the ileocecal region but also significantly prolongs the operation time, increases the suffering of patients, shortens the interval time for reexamination (4), and increases medical expenses (10,11). However, in China, the reported proportion of inadequate bowel preparation is as high as 29.7% (12). The reasons for this high rate is mainly related to diet adjustment (13,14), correct administration of bowel preparation drugs, and required special attention to select patients (15).
Previous studies have shown that the quality of bowel preparation is influenced by the methods the medical staff use to educate and inform the patients (16). Bowel preparation quality also relies on how much information the patient retains and to what degree the patient follows the instructions, such as eating a low-fiber diet the day before the colonoscopy (17) as well as taking the bowel preparation drugs as instructed. The European Society of Gastrointestinal Endoscopy strongly recommends oral and written bowel preparation education (18). However, not all medical units follow these recommendations.
Previous studies have shown that adequate notification was an independent predictor of bowel preparation quality (19), and non-adherence to bowel preparation instructions increased the risk of inadequate bowel preparation (3). In our research, we studied the factors affecting the quality of bowel preparation by using a personal pre- and post-control method. We found that as inpatients, patients received face-to-face bowel preparation education from medical staff, and the patients were able to evaluate their bowel preparations according to the standard pictures that were attached to the wall of the bathroom. The medical staff recommends more bowel preparation according to the results. These methods significantly improved the quality of bowel preparation. An excellent bowel preparation shortened the time to reach the ileocecal region and reduced pain simultaneously.
Bowel preparation quality is closely related to the polyp detection rate (12,20). Early detection and elimination of colorectal polyps can effectively reduce colorectal cancer risk (21). Studies showed that the missed diagnosis prevalence of colon flat adenomas is as high as 27 percent due to poor preparation of the bowel (22). The smaller the diameter of the adenoma, the easier it is to be overlooked (23). The detection rate of adenomas in high-quality bowel preparations was 41% higher than that in low-quality bowel preparations (4). The results of our study showed that face-to-face education from medical staff improved the quality of bowel preparation, and poor bowel preparation increased the possibility of missed colorectal adenoma diagnoses. The missed diagnosis rates of Yamada type I–II adenomas and adenomas with a diameter of less than 5 mm were higher than those of Yamada type III–IV adenomas and adenomas with a diameter of more than 5 mm. In clinical practice, we also found that poor bowel preparation increased the chance of a missed diagnosis of small flat polyps; thus, improving the quality of bowel preparation can increase the detection rate of colorectal adenomas, primarily flat adenomas (24). The detection rate of colorectal adenomas is also related to the ability of the doctors and enough withdrawal time. Doctors who performed colonoscopy in this study were experienced (more than 500 colonoscopies performed) in operation colonoscopy. The withdrawal time for each patient was more than 6 minutes. So we can exclude the impact of the above two variables on colorectal adenoma detection rates. However, this study also had some limitations. The patients with polyps were known by the doctors ahead of the second colonoscopy; this may have resulted in the doctors paying more attention to locating the adenomas, thereby increasing the detection rate of adenomas.
In conclusion, adequate communication with and education of patients are essential for high-quality bowel preparations, which can improve the detection rate of colon lesions. In clinical practice, the most feasible method to improve the patient’s understanding and compliance with the bowel preparation methods is to hand out a standard bowel preparation result picture, and a flow chart mainly based on pictures to general patients during appointments (25-27), provide reeducation via telephone or text messaging (12,28), and send smartphone and social media reminders (29,30) before colonoscopy (31) to improve the quality of bowel preparation and adenoma detection (32). Especially for patients who are assessed as having poor bowel preparation (33,34), such as those with chronic constipation (35,36), should accept personal instruction using the above mentioned methods, or admit to daytime wards if necessary to improve the quality of the bowel preparation for practical colonoscopy examination.
Conclusions
Face-to-face patient education can improve the quality of bowel preparation, then shorten the time to reach the ileocecal region, and increase detection of colorectal adenomas.
Acknowledgments
Thanks are due Dr. Fengxiao Dong for English Language Editing.
Funding: Beijing Science and Technology Program Topic, Capital Citizen’s Health Cultivation: Study on Standardized Quality Control Management of Total Colonoscopy in Opportunistic Screening for Colorectal Cancer (Grant Number: Z161100000116084).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Ethics Committee of Capital Medical University affiliated Beijing Shijitan Hospital. All patients signed written informed consent forms before colonoscopy.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Martens P, Bisschops R. Bowel preparation for colonoscopy: efficacy, tolerability and safety. Acta Gastroenterol Belg 2014;77:249-55. [PubMed]
- Dulskas A, Smolskas E, Kildusiene I, et al. Outcomes of surgical management of iatrogenic colonic perforation by colonoscopy and risk factors for worse outcome. J BUON 2019;24:431-5. [PubMed]
- Okkabaz N, Yilmaz M, Civil O, et al. Outcomes of conversion from laparoscopy to open surgery in geriatric patients with colorectal cancer: a case-controlled study. J BUON 2019;24:1809-16. [PubMed]
- Clark BT, Rustagi T, Laine L. What level of bowel prep quality requires early repeat colonoscopy: systematic review and meta-analysis of the impact of preparation quality on adenoma detection rate. Am J Gastroenterol 2014;109:1714-23; quiz 1724.
- Kucukoner M, Oztekin E, Akdeniz N, et al. Prognostic importance of tumor location and anti-EGFR therapy in patients with K-RAS wild type metastatic colorectal cancer. J BUON 2019;24:1501-6. [PubMed]
- Saltzman JR, Cash BD, Pasha SF, et al. Bowel preparation before colonoscopy. Gastrointest Endosc 2015;81:781-94. [Crossref] [PubMed]
- Soweid AM, Kobeissy AA, Jamali FR, et al. A randomized single-blind trial of standard diet versus fiber-free diet with polyethylene glycol electrolyte solution for colonoscopy preparation. Endoscopy 2010;42:633-8. [Crossref] [PubMed]
- Park DI, Park SH, Lee SK, et al. Efficacy of prepackaged, low residual test meals with 4L polyethylene glycol versus a clear liquid diet with 4L polyethylene glycol bowel preparation: a randomized trial. J Gastroenterol Hepatol 2009;24:988-91. [Crossref] [PubMed]
- Lai EJ, Calderwood AH, Doros G, et al. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc 2009;69:620-5. [Crossref] [PubMed]
- Rex DK, Imperiale TF, Latinovich DR, et al. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol 2002;97:1696-700. [Crossref] [PubMed]
- Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc 2003;58:76-9. [Crossref] [PubMed]
- Liu X, Luo H, Zhang L, et al. Telephone-based re-education on the day before colonoscopy improves the quality of bowel preparation and the polyp detection rate: a prospective, colonoscopist-blinded, randomised, controlled study. Gut 2014;63:125-30. [Crossref] [PubMed]
- Garber A, Sarvepalli S, Burke CA, et al. Modifiable Factors Associated with Quality of Bowel Preparation Among Hospitalized Patients Undergoing Colonoscopy. J Hosp Med 2019;14:278-83. [PubMed]
- Gimeno-García AZ, de la Barreda HR, Reygosa C, et al. Impact of a 1-day versus 3-day low-residue diet on bowel cleansing quality before colonoscopy: a randomized controlled trial. Endoscopy 2019;51:628-36. [Crossref] [PubMed]
- Fang J, Fu HY, Ma D, et al. Constipation, fiber intake and non-compliance contribute to inadequate colonoscopy bowel preparation: a prospective cohort study. J Dig Dis 2016;17:458-63. [Crossref] [PubMed]
- Liu Z, Zhang MM, Li YY, et al. Enhanced education for bowel preparation before colonoscopy: A state-of-the-art review. J Dig Dis 2017;18:84-91. [Crossref] [PubMed]
- Alvarez-Gonzalez MA, Pantaleon MA, Flores-Le RJ, et al. Randomized Clinical Trial: A Normocaloric Low-Fiber Diet the Day Before Colonoscopy Is the Most Effective Approach to Bowel Preparation in Colorectal Cancer Screening Colonoscopy. Dis Colon Rectum 2019;62:491-7. [Crossref] [PubMed]
- Hassan C, Bretthauer M, Kaminski MF, et al. Bowel preparation for colonoscopy: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy 2013;45:142-50. [Crossref] [PubMed]
- Hassan C, Fuccio L, Bruno M, et al. A predictive model identifies patients most likely to have inadequate bowel preparation for colonoscopy. Clin Gastroenterol Hepatol 2012;10:501-6. [Crossref] [PubMed]
- Chiu HM, Lin JT, Wang HP, et al. The impact of colon preparation timing on colonoscopic detection of colorectal neoplasms--a prospective endoscopist-blinded randomized trial. Am J Gastroenterol 2006;101:2719-25. [Crossref] [PubMed]
- Moriyama T, Uraoka T, Esaki M, et al. Advanced technology for the improvement of adenoma and polyp detection during colonoscopy. Dig Endosc 2015;27 Suppl 1:40-4. [Crossref] [PubMed]
- Clark LE, Dipalma JA. Safety issues regarding colonic cleansing for diagnostic and surgical procedures. Drug Saf 2004;27:1235-42. [Crossref] [PubMed]
- Heresbach D, Barrioz T, Lapalus MG, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy 2008;40:284-90. [Crossref] [PubMed]
- Xiang L, Zhan Q, Wang XF, et al. Risk factors associated with the detection and missed diagnosis of colorectal flat adenoma: a Chinese multicenter observational study. Scand J Gastroenterol 2018;53:1519-25. [Crossref] [PubMed]
- Tae JW, Lee JC, Hong SJ, et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastrointest Endosc 2012;76:804-11. [Crossref] [PubMed]
- Spiegel BM, Talley J, Shekelle P, et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation. Am J Gastroenterol 2011;106:875-83. [Crossref] [PubMed]
- Gausman V, Quarta G, Lee MH, et al. A Theory-based Educational Pamphlet With Low-residue Diet Improves Colonoscopy Attendance and Bowel Preparation Quality. J Clin Gastroenterol 2020;54:164-9. [Crossref] [PubMed]
- Lee YJ, Kim ES, Choi JH, et al. Impact of reinforced education by telephone and short message service on the quality of bowel preparation: a randomized controlled study. Endoscopy 2015;47:1018-27. [Crossref] [PubMed]
- Jeon SC, Kim JH, Kim SJ, et al. Effect of Sending Educational Video Clips via Smartphone Mobile Messenger on Bowel Preparation before Colonoscopy. Clin Endosc 2019;52:53-8. [Crossref] [PubMed]
- Desai M, Nutalapati V, Bansal A, et al. Use of smartphone applications to improve quality of bowel preparation for colonoscopy: a systematic review and meta-analysis. Endosc Int Open 2019;7:E216-24. [Crossref] [PubMed]
- Nayor J, Feng A, Qazi T, et al. Impact of Automated Time-released Reminders on Patient Preparedness for Colonoscopy. J Clin Gastroenterol 2019;53:e456-62. [Crossref] [PubMed]
- Wang SL, Wang Q, Yao J, et al. Effect of WeChat and short message service on bowel preparation: an endoscopist-blinded, randomized controlled trial. Eur J Gastroenterol Hepatol 2019;31:170-7. [Crossref] [PubMed]
- Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 2018;30:819-26. [Crossref] [PubMed]
- Martel M, Menard C, Restellini S, et al. Which Patient-Related Factors Determine Optimal Bowel Preparation? Curr Treat Options Gastroenterol 2018;16:406-16. [Crossref] [PubMed]
- Li Y, Jia X, Liu B, et al. Randomized controlled trial: Standard versus supplemental bowel preparation in patients with Bristol stool form 1 and 2. PLoS One 2017;12:e0171563. [Crossref] [PubMed]
- Paik N, Kim ER, Kim TJ, et al. Usefulness of Personal Bowel Habits as a Predictive Factor for Inadequate Bowel Preparation for Colonoscopy: A Prospective Questionnaire-Based Observational Study. Gut Liver 2019;13:169-75. [Crossref] [PubMed]