Symptom burden and characteristics of patients who die in the acute palliative care unit of a tertiary cancer center
Introduction
As cancer care advances and patient expectations increase, patients increasingly spend their final months of life in acute care hospitals receiving aggressive anti-cancer treatments. As a result they often lose the opportunity to receive adequate end-of-life (EOL) care under hospice programs (1). These advanced cancer patients often suffer from severe physical and psychosocial distress that requires intensive interdisciplinary palliative care (2,3).
Several tertiary cancer centers in the United States and Canada now operate palliative care programs that include inpatient and outpatient services to help advanced cancer patients to manage their symptom burden (4,5). While outpatient palliative care clinics focus on the early integration of palliative care with standard oncology care, inpatient services often include more advanced cancer patients who need transition to hospice care. The acute palliative care unit (APCU) is a novel inpatient palliative care program that provides intensive symptom management and facilitates the transition to hospice care (6-10). However, nearly one-third of advanced cancer patients are unable to transfer properly from tertiary cancer centers to hospice (6). These patients are often not prepared for death and unexpectedly die while receiving treatment at APCUs.
South Korea has recently joined to the international effort to improve EOL care by incorporating hospice and palliative care into the Nationalized Health Insurance (NHI) in July 2015. However, Korea’s progress has focused primarily on hospice care, leaving room for improvement in broader palliative care within tertiary cancer centers. Cancer patients, who cannot receive further chemotherapy and are likely to die within a few months, can utilize government-certified hospice centers in Korea. Compared to greater proportions in Western healthcare systems, only 17.5% of advanced cancer patients are successfully transferred to government-certified hospice centers (11). To provide adequate palliative care for advanced cancer patients in tertiary cancer centers, Seoul National University Bundang Hospital (SNUBH) began a palliative care program in 2015 that includes an outpatient supportive care clinic, consultation service and inpatient APCU. Since then, efforts to improve the transition to hospice have increased the referral rate to 46% of advanced cancer patients successfully transferring to government-certified hospice centers from SNUBH by 2017. However, as seen in the United States and elsewhere, many patients often died in the APCU before reaching proper hospice programs.
The aim of this study was to analyze the symptom burden and characteristics of advanced cancer patients who died in the APCU at a Korean tertiary cancer center. Based on the determined characteristics from the present study, we hope to better identify patients in need of earlier and more intensive palliative care in the tertiary cancer centers before it is too late.
Methods
Patient population
Advanced cancer patients admitted to the APCU at SNUBH between April 2015 and March 2016 were included in this retrospective study. We defined advanced cancer as locally advanced, metastatic, or locally recurrent disease for solid tumors, and as primary progressive or relapsed/refractory disease for hematologic malignancies. Locally advanced patients, who were able to receive curative treatments, were excluded. Of the 405 consecutive APCU admissions during this time period, there were 312 individual patients. Within this cohort, 267 patients, who were able to complete the Edmonton Symptom Assessment System (ESAS), were included in this study.
Palliative care service
Our APCU is a 12-bed unit equipped with a comprehensive cancer center. The unit is staffed by an interdisciplinary team composed of palliative care physicians, palliative care nurses, medical oncologists, a social worker, a psychiatrist, pharmacists and chaplains. In addition to serving the APCU, this team also provides services through a consultation-based service and the Outpatient Supportive Care Clinic. Patients are admitted to the APCU following recommendations by their oncologists and subsequent evaluation by palliative care physicians. Sources of admission included transfer from the medical oncology ward, outpatient clinic, emergency department or intensive care unit (ICU) after evaluation by the consultation team. Patients are initially assessed by a palliative care nurse with assessment tools such as the ESAS and Eastern Cooperative Oncology Group (ECOG) performance status scale. ESAS assessments are repeated within 1 week of admission. The palliative care nurse discusses the results with the palliative care specialist, and the physician performs an interview and physical examination to assess the patient. The patients are then managed by the appropriate interdisciplinary team members based on the individual needs of the patient and family.
Clinical characteristics
We collected the following information from the patients’ electronic medical records: demographic features such as age at the time of palliative care consultation prior to APCU admission, gender, religion, and marital status (married, single, widowed, or divorced). We noted cancer-related information such as cancer type and previous lines of chemotherapy. For patients with multiple cancer diagnoses, the cancer diagnosis most responsible for hospitalization was used for analysis. The ECOG performance status of each patient was also assessed. We also obtained the type of discharge from the APCU (hospice, convalescent hospital, home, or death) and source of the APCU admission (oncology service through the consultation team, outpatient clinic, emergency department, or ICU). Last, we collected the time interval from cancer diagnosis to APCU admission, survival after cancer diagnosis, survival after APCU admission and length of APCU stay.
Symptom burden
ESAS scores assessed the severity of ten cancer-associated symptoms (pain, fatigue, nausea, depression, anxiety, drowsiness, dyspnea, anorexia, feeling of well-being, and insomnia). Symptom levels were rated on a numerical scale from 0–10 (0, no symptoms; 10, worst possible symptoms) (12). In accordance with previous studies, symptoms of moderate to severe intensity (scores ≥4) were defined as clinically significant symptoms. The symptom distress scores (SDS) were defined as the sum of the scores of nine items excluding insomnia. Physical SDS (pain, fatigue, nausea, drowsiness, dyspnea, and anorexia), psychological SDS (depression and anxiety) and overall SDS were also calculated. Spiritual distress and financial distress were assessed together with the ESAS by the numerical rating scale.
Statistical analysis
Patient characteristics and symptom assessments were summarized using descriptive statistics including means, medians, frequencies, and percentages. Median ESAS scores were compared between groups using the Wilcoxon Rank-Sum test. Median survival intervals were calculated using Kaplan-Meier analysis. The comparison of survival outcomes between patients who died and patients who were discharged alive was performed using log-rank tests. A stepwise logistic regression analysis was performed to identify factors associated with APCU death. Age, gender and variables with P values less than 0.20 from univariate analysis were included in multivariate analysis. In the case of collinear variables, only one variable was chosen for the multivariate analysis. ESAS scores ≥4 were considered clinically significant symptoms when dividing clinical factors into binary categorical groups. Two-sided P values less than 0.05 were considered statistically significant and confidence intervals (CI) were calculated at a 95% confidence level. All analyses were performed using IBM SPSS Statistics for Windows, version 21.0 (IBM Corp., Armonk, NY, USA).
Results
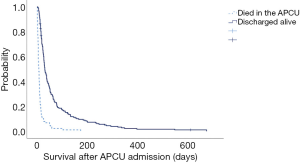
Table 1 shows the demographic information and baseline characteristics of the patients admitted to the APCU. Of the 267 patients, 87 patients (33%) died in the APCU. The entire sample population was South Korean with a median age of 66 years (range, 23–97 years). There were slightly fewer female patients (45%) than male patients. Most patients were married (91%) and affiliated with a religion (61%). The most common primary cancer types were lung (21%), gastric (17%) colorectal (15%), hepatobiliary and pancreatic cancer (14%). Baseline characteristics according to APCU death are summarized in Table S1.
Full table

Full table
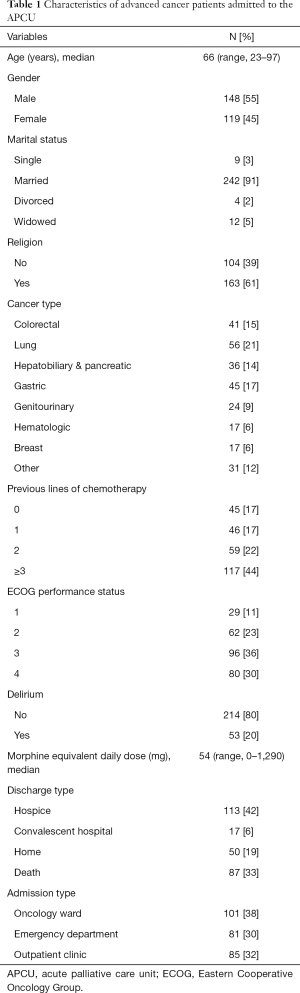
Table 2 compares the baseline ESAS and SDS scores of advanced cancer patients upon APCU admission. Patients who died in the APCU showed higher symptom distress upon APCU admission compared with patients who were discharged from the APCU alive. These patients had higher median ESAS scores for drowsiness (6 vs. 5, P=0.002), dyspnea (4 vs. 2, P=0.001), anorexia (8 vs. 6, P=0.014), and insomnia (6 vs. 4, P=0.002). Physical SDS (28 vs. 25, P=0.002) and overall SDS (47 vs. 40, P=0.004) were also significantly higher in patients who eventually died in the APCU. Pain, fatigue, nausea, depression, anxiety, and feeling of well-being were not significantly different between the two groups.
Full table
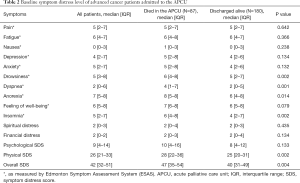
The univariate analysis identified several baseline characteristics and symptoms that were significantly associated with APCU death. These clinical factors were divided into categorical groups and were included in the multivariate analysis: age (≥70 vs. <70), gender (male vs. female), delirium (present or absent), drowsiness (<4 vs. ≥4), dyspnea (<4 vs. ≥4), anorexia (<4 vs. ≥4), insomnia (<4 vs. ≥4), ECOG performance status (1 vs. 2 vs. 3 vs. 4) and religion (nonreligious vs. religious). Because of high collinearity with drowsiness, delirium was not included in the final multivariate analysis. In the multivariate analysis, patients who died in the APCU were more likely to be male [odds ratio (OR) 2.63, 95% confidence interval (CI): 1.49–4.64, P=0.001], have significantly higher ESAS scores of drowsiness (OR 2.08, 95% CI: 1.08–3.99, P=0.029) and higher ESAS scores of dyspnea (OR 2.19, 95% CI: 1.26–3.80, P=0.005) as shown in Table 3.
Full table
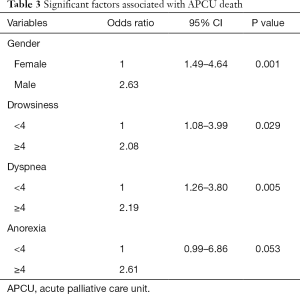
Table 4 shows the median time intervals associated with survival according to discharge type from the APCU. The time from advanced cancer diagnosis to APCU admission did not significantly differ for patients who died compared to patients who were discharged alive from the APCU (13.6 vs. 11.1 months, P=0.959). Median survival following advanced cancer diagnosis did not differ significantly between patients who died in the APCU and those who were discharged alive (14.3 vs. 13.8 months, P=0.189). However, as the grouping was based on APCU death, survival after APCU admission was significantly lower for those who died in the APCU compared to those who were discharged alive (7.0 vs. 31.0 days, P<0.001).

Full table
Figure 1 shows the Kaplan-Meier survival curves for patients who died in the APCU compared to patients who were discharged alive from the APCU. Patients who were successfully discharged from the APCU to a convalescent hospital, hospice center or back home had a median survival time of 31 days. In contrast, patients, who died in the APCU before transferring to proper hospice care, had a median survival time of 7 days. Survival after APCU admission was significantly shorter in males than in females (15 vs. 29 days, P=0.001). This survival time spans from the first day of APCU admission until death regardless of whether it was at the APCU or elsewhere.
Discussion
In this study, we demonstrated that patients who die in the APCU before transferring to hospice are more likely to be male and have significantly higher symptom burden such as drowsiness and dyspnea. To the best of our knowledge, this is the first study in Korea to evaluate the characteristics and symptom levels of advanced cancer patients who die in the APCUs of tertiary cancer centers compared to patients who are discharged alive.
The purpose of the APCU is to enhance quality of life and facilitate the transition of advanced cancer patients to hospice. It is notable that 67% of our advanced cancer patients were able to be discharged from the APCU alive and that almost two-thirds of the discharged patients were successfully referred to government-certified hospice centers. In Korea, home hospice is not formally established, and the majority of patients receive palliative care in government-certified hospice centers. Although nearly half of advanced cancer patients were successfully referred to hospice centers, one-third of patients eventually died in the APCU in our study. These patients, who did not have the opportunity to transfer to hospice or return back home, were the focus of the present study. The patients who died in the APCU showed significantly higher ESAS scores for drowsiness, dyspnea, anorexia and insomnia compared with patients who were discharged alive. This finding is in accordance with the previous study that reported an increase in the severity of dyspnea, drowsiness, poor feeling of well-being, anorexia, and fatigue particularly in the last week of life (13). The increased symptom burden experienced by the patients who died in the APCU indicates the need for more proactive EOL care for this subset of advanced cancer patients in tertiary cancer centers.
In a US study, male gender, specific cancer primaries, and admissions from oncology units were associated with death in the APCU (6). In a Korean study, male sex and poor performance status were also significantly associated with shorter survival after enrollment in palliative care services (14). Our multivariate analysis also showed that patients who died in the APCU were more likely to be male. As explained in the previous study, late referral to palliative care in males may reflect the patriarchal culture of Korea (14). Although further studies may be needed to validate this finding, male patients tend to get more support from the family members and receive more aggressive cancer care at the EOL compared with female patients. Another recent study found that admission from emergency departments, poor feelings of well-being, dyspnea and delirium were independently associated with APCU death (15). Our study also showed that patients who died in the APCU have a significantly higher symptom burden in drowsiness and dyspnea. Delirium is a well-established prognostic factor for increased symptom burden and in-hospital mortality for advanced cancer patients admitted to comprehensive cancer center APCUs (16,17). Drowsiness often overlaps with delirium and sleeping problems for advanced cancer patients and, alongside dyspnea, these symptoms should be considered as primary factors indicating imminent death in advanced cancer patients. Based on the present study and previous studies (6,14,15), we would like to suggest that male patients expressing high levels of drowsiness and dyspnea at the time of APCU admission require immediate EOL interventions including family conferences to prepare for impending death.
Our study highlights the importance of the timing of palliative care referrals. The median overall survival after APCU admission was only 21 days in our patients. Although this is similar to a previous study that reported 21 days of survival after APCU admission (6), it is striking that even patients who were discharged alive survived about one month after discharge. Furthermore, one-third of patients who died in the APCU, survived only a week after APCU admission. Therefore, there is a demonstrated need to alter this timeline to provide adequate EOL care in advanced cancer patients. Early integration of palliative care, concurrent with standard oncology care, may be an answer to this problem. In Temel’s renowned study, patients who received early palliative care, were less likely to receive chemotherapy within 60 days of death and were more likely to be enrolled in hospice programs (18,19).
Our study has several limitations. First, as it was a retrospective study, we could not collect some important data. For instance, ESAS assessments were incomplete in 45 patients, and we were unable to identify the exact reasons for why these assessments were incomplete. Second, we did not systematically screen for delirium using tools such as the Memorial Delirium Assessment Scale. As the diagnosis of delirium was made clinically in our patients, and as many patients with overt delirium were excluded from this study (probably due to incomplete ESAS), the data on delirium may not be reliable in our study. Finally, this study was performed in a single center in Korea, which limits the generalizability of this study.
In conclusion, advanced cancer patients who die in the APCU are more likely to be male and have significantly higher symptom burden including drowsiness and dyspnea. These patients are admitted to the APCU later and have much lower survival compared with those who are discharged alive from the APCU.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The institutional review board at Seoul National University Bundang Hospital approved this study (No. B-1702/384-104) and waived written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Saito AM, Landrum MB, Neville BA, et al. The effect on survival of continuing chemotherapy to near death. BMC Palliat Care 2011;10:14. [Crossref] [PubMed]
- Elsayem A, Smith ML, Parmley L, et al. Impact of a palliative care service on in-hospitalmortality in a comprehensive cancer center. J Palliat Med 2006;9:894-902. [Crossref] [PubMed]
- Cleeland CS, Gonin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 1994;330:592-6. [Crossref] [PubMed]
- Hui D, Kim YJ, Park JC, et al. Integration of oncology and palliative care: a systematic review. Oncologist 2015;20:77-83. [Crossref] [PubMed]
- Ferrell BR, Temel JS, Temin S, et al. Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2017;35:96-112. [Crossref] [PubMed]
- Hui D, Elsayem A, Palla S, et al. Discharge outcomes and survival of patients with advanced cancer admitted to an acute palliative care unit at a comprehensive cancer center. J Palliat Med 2010;13:49-57. [Crossref] [PubMed]
- Bruera E, Hui D. Integrating supportive and palliative care in the trajectory of cancer: establishing goals and models of care. J Clin Oncol 2010;28:4013-7. [Crossref] [PubMed]
- Hui D, Bruera E. Models of integration of oncology and palliative care. Ann Palliat Med 2015;4:89-98. [PubMed]
- Amano K, Morita T, Tatara R, et al. Association between early palliative care referrals, inpatient hospice utilization, and aggressiveness of care at the end of life. J Palliat Med 2015;18:270-3. [Crossref] [PubMed]
- Mercadante S, Adile C, Caruselli A, et al. The palliative-supportive care unit in a comprehensive cancer center as crossroad for patient’s oncological pathway. PLoS One 2016;11:e0157300. [Crossref] [PubMed]
- National Cancer Center, Hospice and Palliative Care website. Available online: accessed May 27, 2018.http://hospice.cancer.go.kr/home/contentsInfo.do?menu_no=443&brd_mgrno
- Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patient. J Palliat Care 1991;7:6-9. [Crossref] [PubMed]
- Hui D, dos Santos R, Chisholm GB, et al. Symptom expression in the last seven days of life among cancer patients admitted to acute palliative care units. J Pain Symptom Manage 2015;50:488-94. [Crossref] [PubMed]
- Baek YJ, Shin DW, Choi JY, et al. Late Referral to Palliative Care Services in Korea. J Pain Symptom Manage 2011;41:692-9. [Crossref] [PubMed]
- Shin SH, Hui D, Chisholm GB, et al. Characteristics and outcomes of patients admitted to an acute palliative care unit from the emergency centre. J Pain Symptom Manage 2014;47:1028-34. [Crossref] [PubMed]
- Hui D, Bush SH, Gallo LE, et al. Neuroleptic dose in the management of delirium in patients with advanced cancer. J Pain Symptom Manage 2010;39:186-96. [Crossref] [PubMed]
- de la Cruz M, Yennu S, Liu D, et al. Increased symptom expression among patients with delirium admitted to an acute palliative care unit. J Palliat Med 2017;20:638-41. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Greer JA, Pirl WF, Jackson VA, et al. Effect of early palliative care on chemotherapy use and end-of-life care in patients with metastatic non-small-cell lung cancer. J Clin Oncol 2012;30:394-400. [Crossref] [PubMed]