
Distribution of cerebral artery stenosis and risk factors in ethnic Zhuang and Han patients with ischemic stroke in Guangxi province
Introduction
Intracranial and/or extracranial atherosclerosis (I-ECAS) is the primary cause of ischemic stroke worldwide. Past research has established that the distribution of I-ECAS is influenced by regional and ethnic factors. For instance, stroke patients in the west more commonly suffer from ECAS, while intracranial atherosclerosis (ICAS) is more prevalent in the Asian population (1,2). In China, approximately 30–40% of acute ischemic strokes and more than 50% of transient ischemic attacks (TIAs) are caused by ICAS (3,4), with a regional north-to-south gradient in the distribution of strokes (5). Indeed, Pu et al. (6) reported that the proportion of patients with ICAS in China is significantly higher in the northern region (50.22%) than in the southern region (41.88%).
One southern area, the Guangxi Zhuang Autonomous Region, is a multi-ethnic province located in southwest China. The Zhuang ethnic group, the largest minority in China, accounts for 31.39% of the total population of Guangxi. However, few studies have investigated the distribution of arterial stenosis in ischemic stroke patients of the Zhuang population in Guangxi, while the differences between stroke distribution in Zhuang and Han ethnicities also remains unclear. The present study aimed to summarize the distribution characteristics of intracranial/extracranial artery stenosis in Guangxi patients of different ethnicities following their first ischemic stroke using 64-slice spiral computed tomographic angiography (CTA) scanning.
Methods
Patient population
The present study was approved by the ethics committee of our institution, and was carried out at the Department of Neurology in the First Affiliated Hospital of Guangxi Medical University (Guangxi, Nanning, China). From January 1 to December 31, 2017, patients who experienced their first ischemic stroke onset within 14 days of admission and were within the age of 18–80 years old, were enrolled into the present study. Patients were excluded when their cerebral infarction was attributable to head trauma, or when their ischemic lesions were attributable to complications from subarachnoid hemorrhage or an angiography procedure.
A total of 1,122 patients, who were diagnosed with ischemic stroke via computed tomography (CT) or magnetic resonance imaging (MRI), were examined. On admission, baseline data including age, gender, ethnicity, medical history, and physical examination results, were collected. All patients underwent a specified clinical evaluation, including laboratory tests, a wide range of blood tests, and electrocardiography. Furthermore, intracranial and extracranial carotid vessels were examined by CTA. Stroke subtypes were classified according to the Chinese ischemic stroke subclassification (CISS) criteria (7). The stroke subtype was assigned to each patient by 2 investigators. In case of discrepancies, these patient records were reviewed by a senior investigator. The final categorization was based on the consensus agreement of all investigators.
Definition of intracranial and extracranial arterial stenosis
The internal carotid artery (ICA) can be separated into 7 segments, as described by Bouthillier et al. (8): C1, cervical; C2, petrous; C3, lacerum; C4, cavernous; C5, clinoid; C6, ophthalmic; C7, communicating. C5 is the boundary of the intracranial/extracranial segment. Meanwhile, the vertebral artery can be divided into intracranial/extracranial segments, with the foramen magnum serving as the boundary. The intracranial arteries include the following: the carotid intracranial segment (I-ICA: C5-C7), the middle cerebral artery (MCA), the anterior cerebral artery (ACA), the posterior cerebral artery (PCA), the intracranial segment of the vertebral artery (I-VA), and the basilar artery (BA). The extracranial arteries include the following: the carotid extracranial segment (E-ICA: C1-C4), the extracranial segment of the vertebral artery (E-VA), the common carotid artery (CC), and the subclavian artery (SUBA).
Extracranial artery stenosis was measured according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) stenosis grading method (9) as follows: stenosis (%) = (1 − N/D) × 100% (N: the diameter of the narrowest lesion; D: the diameter of the distal normal vessel). The categories of stenosis were as follows: no stenosis, 0%; mild stenosis, ≤29%; moderate stenosis, 30–69%; severe stenosis, 70–99%; and complete occlusion.
Intracranial artery stenosis was measured according the method proposed by the Warfarin-Aspirin Symptomatic Intracranial Disease Study (WASID) (10,11) as follows: stenosis (%) = [(Dn − Ds)/Dn) ×100% (Ds, the diameter of the artery at the site of the most severe stenosis; Dn, the diameter of the proximal normal vessel). If the proximal segment was diseased, contingency sites, including the distal artery (second choice), and the feeding artery (third choice), were chosen to measure Dn). The categories of intracranial arterial stenosis and occlusion were as follows: (I) normal, 0–29%; (II) mild, 30–49%; (III) moderate, 50–79%; (IV) severe, 80–99%; (V) occlusion, 100%.
Definition of vascular risk factors
Hypertension (12), diabetes (13), hyperlipidemia (14), heart disease, and Hyperhomocysteinemia (15) were defined based on the personal history of these diagnoses, and on the present diet or medical treatment for these disorders. Smoking habit was qualified as smoking >5 cigarettes per day, while alcohol consumption was qualified as the consumption of >50 mL of alcohol/day.
Statistical analysis
All analyses were performed using SPSS version 19.0 (SPSS Inc., Chicago, IL, USA). Categorical variables are presented as percentages. The chi-square test or Fisher’s exact test were used to compare categorical variables. Continuous variables are presented as mean [standard deviation (SD)]. The independent samples t-test or Wilcoxon test were used to compare continuous variables. Multinomial logistic regression analyses were performed to identify vascular risk factors that were independently associated with each type of atherosclerosis using the non-atherosclerotic group as the reference for all analyses. For traditional vascular risk factors, all risk factors significantly associated with any type of atherosclerosis were included in the model for the univariate analyses (P<0.05). All tests were two-sided, and P<0.05 was considered to be statistically significant.
Results
Overall baseline characteristics of the study groups
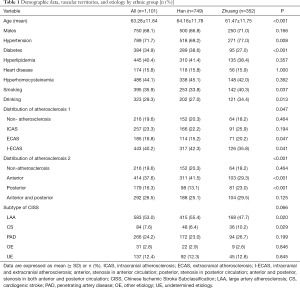
Table 1 shows the baseline characteristics of the cohort as a whole and within the categories determined by participant ethnicity. A total of 1,122 patients met the inclusion criteria. Furthermore, among these patients, 749 patients were of Han ethnicity, 352 patients were of Zhuang ethnicity, while 21 patients were of another ethnicity. Since the number of patients of other ethnicities was too small to be analyzed, only 1,101 patients of the Han and Zhuang ethnicities were included in the study. Overall, the mean age at admission and onset of stroke was 63.28±11.84 years (range, 18–80 years). Among all patients, 68.1% were male, 71.7% had a history of hypertension, 34.9% had a history of diabetes mellitus, 40.4% had a history of hyperlipidemia, 15.8% had a history of heart disease, 44.1% had a history of hyperhomocysteinemia, 35.9% were current smokers, and 29.3% were heavy drinkers.
Full table
Patients in the Zhuang group were younger on average than patients in the Han group. Zhuang patients were more likely to consume alcohol and cigarettes, and had a significantly higher rate of hypertension and a lower rate of diabetes mellitus.
Differences in the distribution of cerebral artery stenosis between ethnic groups
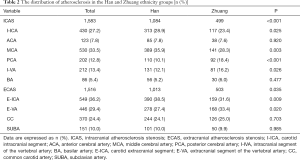
The distribution of cerebral artery stenosis is shown in Tables 1 and 2. In total, there were 885 (80.4%) patients with atherosclerosis. Furthermore, a total of 3,099 stenotic vessels were detected in 597 patients with arterial stenosis in the Han group and in 288 patients in the Zhuang group. Among these, 1,583 (51.1%) were cases of ICAS, while 1,516 (48.9%) were cases of ECAS. The trend in the distribution was consistent between these two ethnic groups, with I-ECAS being the most common lesion type, followed by ICAS. However, in the Zhuang group, the percentage of ECAS was notably higher than that in the Han group, while the percentage of I-ECAS was significantly lower than that in the Han group. The percentage of stenosis in the anterior circulation in the Zhuang group was significantly lower than that in the Han group. Conversely, the percentage of stenosis in the posterior circulation in the Zhuang group was significantly higher than that in the Han group. In the Zhuang group, the proportion of I-ICA, MCA, and E-VA were notably lower than those in the Han group, while the proportion of PCA, I-VA, and E-ICA were notably higher than those in the Han group.
Full table
Differences in stroke etiology between groups
The stroke etiology is shown in Table 1. Large artery atherosclerosis (LAA) was the most commonly identified cause of stroke, followed by penetrating artery disease (PAD). In the Zhuang group, the proportion of LAA was significantly lower than that of the Han group, while the proportion of cardiogenic stroke (CS) was higher than that in the Han group.
Differences in risk factors between groups
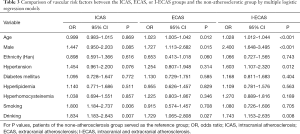
When the non-atherosclerosis group was used as a reference group, the multiple logistic regression analysis (Table 3) indicated that smoking and drinking were independent risk factors for ICAS; older age, male gender, and drinking were independent risk factors for ECAS, while older age, male gender, hypertension and drinking were independent risk factors for I-ECAS.
Full table
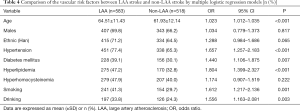
The multiple logistic regression analysis indicated that older age, hypertension, diabetes mellitus, hyperlipidemia, smoking, and drinking were significantly associated with an increased risk of LAA stroke (Table 4).
Full table
Discussion
The present study demonstrated that the incidence of ICAS was higher than the incidence of ECAS (51.1% vs. 48.9%) in the Guangxi population. Furthermore, the rate of cerebral artery stenosis was higher than that reported in previous studies, which was 46.6% in the CICAS study (3) and 49.8% in Shi’s study (16). This change in prevalence may be explained by the following: (I) the subjects were selected using a method that differed from the previous studies, as the CICAS study (3) excluded patients with heart disease, while the present study enrolled patients with heart disease. Thus, the present inclusion criteria were broader; (II) the definition of arterial stenosis was different to that used in previous studies: in the CICAS study, ICAS was defined as a ≥50% diameter reduction of the MRA, while in the study conducted by Shi et al., a lesion of extracranial artery stenosis <30% was defined as “atherosclerotic change”, and not ECAS (16). In contrast, the present study evaluated the different degrees of stenosis, including mild stenosis, through CTA. According to the literature and digital subtraction angiography data, the sensitivity and specificity of CTA in the diagnosis of intra-extracranial artery stenosis was significantly higher than that of MRA (17,18); (III) in recent years, several studies have demonstrated that the proportion of ECAS is increasing in the Asian population. Katsumata et al. (19) revealed that carotid plaques could be identified in 76.2% of Japanese patients, while bilateral plaques can be found in 58.2% of patients. These lesions are more frequently observed at present when compared to the rate observed in the last century. Furthermore, a Korean study reported that the incidence of I-ECAS (39%) was significantly higher in the Korean population, when compared to the incidence of ICAS and ECAS. These present results are consistent with the above findings. The reasons for these changes may be the adoption of a Western life style by the Asian population. In addition, Asian dietary habits have changed with an increase in the intake of animal fats and proteins, and the reduction in the intake of carbohydrates and rice.
The present data demonstrate that the trend in the distribution of atherosclerosis is consistent between the Zhuang and Han ethnicities, with I-ECAS being the most common lesion type, followed by ICAS. However, ethnic variations were observed between these groups, with a higher rate of ECAS and a lower rate of I-ECAS in the Zhuang group, when compared to the Han group. Furthermore, Zhuang patients had a higher percentage of stenosis in the posterior circulation and a lower percentage of stenosis in the anterior circulation, when compared to Han patients. These differences were considered to be the result of comprehensive factors. Environmental factors, lifestyle, age, susceptibility genes, and the anatomy of the intra-/extracranial artery may be involved in the progression of cerebral arterial stenosis. It was found that patients of male gender and older age were more likely to suffer from ECAS, and hypertension was only associated with ECAS, while smoking was an independent risk factor of ICAS, which is consistent with previous findings (20,21). Zhuang patients were more likely to consume cigarettes and alcohol, and this may increase the risk of hypertension. The difference in risk factors between groups may explain the observed difference in the distribution of cerebral artery stenosis. Moreover, many studies (22-25) have shown that having a genetic polymorphism is another influential factor for these differences. The difference in genetic polymorphisms between the Zhuang and Han ethnicities should be further investigated.
CISS is a new sub-classification of ischemic stroke that takes into consideration both etiological and pathophysiological information. In CISS, the atherosclerosis of the aortic and intra-/extracranial large arteries belong to LAA (7,26). The present study revealed that LAA was the most frequent subtype of stroke in the populations studied, which is supported by previous studies (27,28). The logistic regression models revealed that among the uncontrollable factors (such as age, gender, and ethnicity), only age was associated with LAA stroke. It is known that age is a non-negligible primary risk factor that contributes to atherosclerosis, because of the exposure time to risk factors is longer in the older population (20,29). After multinomial regression analysis, diabetes mellitus, hyperlipidemia, smoking, and drinking were independent risk factors of LAA stroke. The results of the present study are similar with the report of Tan et al. (28).
Some limitations of this study should also be addressed. First, the study was hospital-based, and the participating hospital was in the upper range of first-class hospitals. Thus, some degree of sampling bias existed. Secondly, the selected cases were all patients with ischemic stroke, and did not include patients with asymptomatic cerebral artery stenosis or healthy people. Thus, these results may not be representative the whole population. In addition, not all influential factors of atherosclerosis were tested, and thus further studies are necessary.
Conclusions
The present study contributes to the understanding of the distribution of cerebral artery stenosis and risk factors in Zhuang and Han Patients with ischemic stroke in Guangxi Province. There is an ethnicity-dependent difference in the distribution of cerebral artery stenosis in Guangxi. The proportion of ECAS was higher and the proportion of I-ECAS was lower in Zhuang patients. These observed differences in risk factors between groups can help to explain the variation in the distribution of cerebral atherosclerosis. This observation may have practical implications for the design of specific prevention strategies in stroke. In order to decrease the risk of stroke, public health measures should be strengthened and social determinants of health and risk factor prevention/control should be improved for those at high risk of artery atherosclerosis.
Acknowledgments
Funding: This work was supported by the Natural Science Foundation of China (No. 81860222), self-Foundation of Guangxi Health Commission (Z20190458), and Science Foundation of Qingxiu district, Nanning (2019039).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The present study was approved by the ethics committee of the First Affiliated Hospital of Guangxi Medical University.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kim JS, Bonovich D. Research on Intracranial Atherosclerosis from the East and West: Why Are the Results Different? J Stroke 2014;16:105-13. [Crossref] [PubMed]
- Hao Q. Ethnic influences on neurovascular coupling: a pilot study in whites and Asians. Stroke 2010;41:383-4. [Crossref] [PubMed]
- Wang Y, Zhao X, Liu L, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke 2014;45:663-9. [Crossref] [PubMed]
- Lin J, Yi X. CTA study of Cerebral watershed infarction and artery stenosis. Journal of Qiqihar Medical College 2007;28:2066-8.
- Wang W, Jiang B, Sun H, et al. Prevalence, Incidence and Mortality of Stroke in China: Results from a Nationwide Population-Based Survey of 480,687 Adults. Circulation 2017;135:759. [Crossref] [PubMed]
- Pu Y, Liu L, Wang Y, et al. Geographic and Sex Difference in the Distribution of Intracranial Atherosclerosis in China. Stroke 2013;44:2109-14. [Crossref] [PubMed]
- Gao S, Wang YJ, Xu AD, et al. Chinese ischemic stroke subclassification. Front Neurol 2011;2:6. [Crossref] [PubMed]
- Bouthillier A, van Loveren HR, Keller JT. Segments of the internal carotid artery: a new classification. Neurosurgery 1996;38:425-32. [PubMed]
- Listed N. North American Symptomatic Carotid Endarterectomy Trial. Methods, patient characteristics, and progress. Stroke 1991;22:711-20. [Crossref] [PubMed]
- Chimowitz MI, Kokkinos J, Strong J, et al. The Warfarin-Aspirin Symptomatic Intracranial Disease Study. Neurology 1995;45:1488-93. [Crossref] [PubMed]
- Samuels OB, Joseph GJ, Lynn MJ, et al. A Standardized Method for Measuring Intracranial Arterial Stenosis. Ajnr Am J Neuroradiol 2000;21:643-6. [PubMed]
- Liu LS. 2010 Chinese guidelines for the management of hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579-615. [PubMed]
- Zhong Hua Yi Xue Hui Tang Niao Bing Xue Fen Hui. Guidelines for management of type 2 diabetes in China. Chinese Journal of Diabetes Mellitus 2014;6:447-98.
- Zhong Guo Cheng Ren Xue Zhi Yi Chang Fang Zhi Zhi Nan Xiu Ding Lian He Wei Yuan Hui. Guideline for management of adult dyslipidemia in China. Chinese Circulation Journal 2016;31:937-53.
- Lin Y, Zhang L, Bao J, et al. Risk factors and etiological subtype analysis of brainstem infarctions. Journal of the Neurological Sciences 2014;338:118-21. [Crossref] [PubMed]
- Shi HZ, Li D, Li SM, et al. Analysis of the etiologic factors in 1000 Chinese patients with ischemic in cerebrovascular disease by DSA. Chinese Journal of Cerebrovascular Diseases 2005;2:437-40.
- González RG, Lev MH, Goldmacher GV, et al. Improved outcome prediction using CT angiography in addition to standard ischemic stroke assessment: results from the STOPStroke study. PLoS One 2012;7:e30352. [Crossref] [PubMed]
- Bash S, Villablanca JP, Jahan R, et al. Intracranial vascular stenosis and occlusive disease: Evaluation with CT angiography, MR angiography, and digital subtraction angiography. Meeting of the American-Society-Of-Neuroradiology 2005;1012-21.
- Katsumata T, Nishiyama Y, Yamaguchi H, et al. Extracranial carotid plaque is increasing in Japanese ischemic stroke patients. Acta Neurol Scand 2007;116:20-5. [Crossref] [PubMed]
- López-Cancio E, Galan A, Dorado L, et al. Biological signatures of asymptomatic extra- and intracranial atherosclerosis: the Barcelona-AsIA (Asymptomatic Intracranial Atherosclerosis) study. Stroke 2012;43:2712-9. [Crossref] [PubMed]
- Wei W, Hu ZW, Zeng QH, et al. Distribution and risk factors of cerebral artery stenosis in patients with actue ischemic stroke. Intenational Journal of Cerebrovasular Diseases 2014;22:528-34.
- Chen J, Huang HT, Yuan QR, et al. Association of SNP of leukocyte differentiation antigen-CD40 gene and its serum level with ischemic stroke. Zhonghua Yu Fang Yi Xue Za Zhi 2016;50:239. [PubMed]
- Wei YS, Liu YG, Huang RY, et al. Intercellular adhesion molecule-1 gene K469E polymorphism and genetic susceptibility of ischemic stroke in Chinese Zhuang populations. Chinese Journal of Medical Genetics 2005;22:305-8. [PubMed]
- Ehret GB, Munroe PB, Rice KM, et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 2011;478:103-9. [Crossref] [PubMed]
- Pan Y, Chen W, Xu Y, et al. Genetic Polymorphisms and Clopidogrel Efficacy for Acute Ischemic Stroke or Transient Ischemic Attack: A Systematic Review and Meta-analysis. Circulation 2017;135:21. [Crossref] [PubMed]
- Chen PH, Gao S, Wang YJ, et al. Classifying Ischemic Stroke, from TOAST to CISS. CNS Neuroscience & Therapeutics 2012;18:452-6. [Crossref] [PubMed]
- Li XL, Liao XL, Bai SP, et al. Analysis of subtype of CISS in acute ischemic stroke. Modern Journal of Integrated Traditional Chinese and Western Medicine 2014;23:3084-7.
- Tan LY, Song YB, Jiao Y, et al. Analysis of the relationship between Chinese ischemic stroke subclassification and risk factors of acute cerebral ischemic stroke. Chinese Journal of Cerebrovascular Disease 2013;7:82-9.
- Wong KS, Ng PW, Tang A, et al. Prevalence of asymptomatic intracranial atherosclerosis in high-risk patients. Neurology 2007;68:2035-8. [Crossref] [PubMed]


