Placebo effect of acupuncture on insomnia: a systematic review and meta-analysis
Introduction
Insomnia is the most common clinical sleep disorder with an increasing prevalence (1). Long-term insomnia greatly affects the daytime function, thereby damaging the memory and attention of the patient (2), while increasing the incidence of many common chronic diseases and the risk of comorbidity of neuropsychiatric diseases (3,4). The treatment of insomnia mainly includes cognitive behavioral therapy for insomnia (CBT-I) and pharmacotherapy (including BZ and BZRAs, antidepressants, antipsychotics, antihistamines, phytotherapeutic substances, and melatonin). In complementary and alternative medicine, several treatments for insomnia, including acupuncture, aromatherapy, meditative movement therapies, music therapy, and yoga, have been suggested (1). In the present meta-analysis, we explored the efficacy of acupuncture and its placebo effect in the treatment of insomnia.
Acupuncture is a traditional Chinese medicine therapy that uses sterile needles to penetrate specific points in the body to treat specific diseases. These acupoints are considered to be the reaction points of the viscera on the body surface; the same visceral acupoints are connected in the series to form the meridians and spread throughout the body. The principle of acupuncture is that a needle is used to act on specific acupoints, with some reinforcing-reducing methods to achieve the effect of “De qi.” “Qi” is a type of energy that maintains the body functions which follows the meridian and nourishment of the whole body, and the acupoints are the points where the “qi” flows in, gathers, and flows out. According to the theory of Yin and Yang, “qi” also exhibits the difference in yin and yang, and the basic pathogenesis of insomnia in Chinese medicine is the imbalance of yin and yang. Furthermore, acupuncture can stimulate specific acupoints to regulate the qi by reinforcing-reducing methods and balance yin and for treating insomnia.
In recent years, a large number of standardized randomized controlled trials (RCTs) have been carried out on the acupuncture treatment of insomnia, and a series of high-quality articles have been published (5,6). Some meta-analyses confirmed the efficiency of acupuncture in the treatment of insomnia (7,8). Consecutively, whether the efficacy of acupuncture is equivalent to placebo, and even the acupuncture treatment can be termed as “mega-placebo” (9). Unlike the targeted intervention of pharmacology, acupuncture treatment of diseases is a multi-system, multi-target self-regulation process. Moreover, “De qi” is often considered as the judgment of whether acupuncture is effective or not, which is a virtual concept and cannot be detected objectively. In order to study the placebo effect of acupuncture, sham acupuncture was used in clinical RCTs. It primarily included invasive acupuncture at the non-effective points (minimal acupuncture) and non-invasive acupuncture for the special needle (placebo acupuncture). Thus, this study analyzed the clinical RCTs of acupuncture and sham acupuncture for insomnia to further elucidate the clinical efficacy of acupuncture for insomnia and its placebo effect.
Methods
This review was registered in PROSPERO (CRD42015025013; http://www.crd.york.ac.uk/PROSPERO) in July 2019 (not yet registered, ID: 141446).
Search strategy and study selection
We searched the literature from May to July, 2019 in the following English and Chinese databases: (I) PubMed, (II) Embase, (III) Web of Science, (IV) The Cochrane Library, (V) China Knowledge Resource Integrated Database (CNKI), (VI) Chongqing VIP Information, (VII) Wanfang Database. English search terms, based on the medical subject headings thesaurus were “insomnia” OR “sleeplessness” OR “sleep disorder” and “acupuncture” OR “electroacupuncture” OR “needle.” The Chinese search strategy was adjusted for Chinese medical terms and their usage in the literature. The following terms were searched in the Chinese database: SHI MIAN (“insomnia”), BU MEI (“insomnia”), SHUI MIAN ZHANG AI (“insomnia”), ZHEN JIU (“acupuncture”), ZHEN CI (“acupuncture”), DIAN ZHEN (“electroacupuncture”), and the Medical Subject Headings were “Dyssomnias” and “Acupuncture Therapy.” The reference lists of relevant articles were examined to identify the citations not captured by the electronic searches. The corresponding authors were contacted for missing information.
The two authors (C Liu, H Xi) independently screened the titles and abstracts of the searched literature based on prespecified inclusion and exclusion criteria and assessed the full text of the potentially eligible studies. The prespecified inclusion criteria were (I) type of studies: randomized controlled trials and blinding and allocation concealments were not limited; (II) types of participants: clear diagnosis of insomnia, age >18 years, the gender and case source were not limited; (III) types of interventions: acupuncture (including electroacupuncture) for the treatment group and sham acupuncture for the control group; (IV) types of outcomes: the primary outcome was PSQI, and the secondary outcomes were ISI, PSG, and actigraphy monitoring results. At each stage of screening and assessing the eligibility of studies, we excluded the trials that did not fulfill the prespecified inclusion criteria in the event of duplicated or missing data. All the steps were performed independently and cross-checked by two reviewers (C Liu, H Xi). Any disagreement in the process was resolved by consensus or arbitration by one of other three experienced and authoritative reviewer (W Wu, X Wang, S Qin).
Data extraction and quality assessment
The reviewers independently extracted and assessed the data from all eligible studies into a standardized data extraction form. The following specific characteristics were extracted from each study: study details (first author, date, published language); baseline information (age, sample size, main diagnosis or population, baseline sleep quality); methodology (randomization, allocation concealment, blinding); intervention; outcome; study conclusion. The corresponding authors were contacted by email for missing information, and if still not available, the study was excluded.
The quality of studies was assessed using the Cochrane risk of bias assessment tool (10), which served as a qualitative tool to evaluate the following domains: (I) random sequence generation; (II) allocation concealment; (III) blinding of participants and personnel; (IV) blinding of outcome assessment; (V) incomplete outcome data; (VI) selective reporting; and (VII) other bias (we assessed trials with no reported monitoring of self-acupressure procedures with a high risk of compliance bias).
Data synthesis and statistical analysis
Review Manager (RevMan) version 5.3 (Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was utilized to qualitatively summarize the eligible studies. (I) Combination of effects: the scores of PSQI, ISI, PSG, and actigraphy constituted the enumeration data and relative ratio (RR), and the results were expressed as 95% confidence interval (CI). (II) Heterogeneity test: the test level was set to α=0.05. The degree of heterogeneity was judged by subgroup and sensitivity analyses. If statistical homogeneity was detected in each study (P<0.05, I2<50%), the fixed-effect model was used for analysis, while if heterogeneity was observed between each study (P≤0.05, I2>50%), the source of heterogeneity was analyzed by random-effects model and combined with the subgroup or sensitivity analysis. If the heterogeneity was extremely large to conduct a meta-analysis, descriptive analysis was performed. (III) Sensitivity analysis: the articles were removed sequentially to observe the changes in the heterogeneity, and the combined effect value WMD and RR value change were recorded. If the heterogeneity altered after removal of one article, it could be the source of heterogeneity; then, the underlying reason was analyzed. However, the unchanged heterogeneity indicated stable results. (IV) Subgroup analysis was performed based on the choice of different sham acupuncture schemes and patient characteristics.
Results
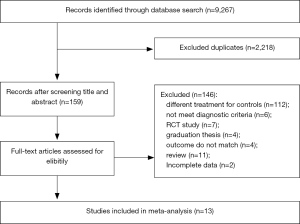
A total of 9,267 articles were acquired from 7 databases, and 2,218 duplicate studies were identified and excluded. Irrelevant documents were excluded after screening the titles and abstracts, and 159 full-text articles were assessed to extricate those that met the eligibility criteria (Figure 1). Based on the prespecified inclusion/exclusion criteria, we obtained a qualitative summary of 13 studies with a total of 1,061 participants eligible for meta-analysis. In to complete the missing information, we contacted two authors but did not receive any response.
Study characteristics
The baseline information of the thirteen studies included in this systematic review and meta-analysis is summarized in Table 1; four were published in English and nine in Chinese. However, all the studies were conducted in China.
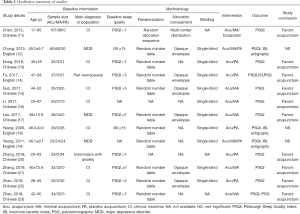
Full table
Of the 13 included studies, one study was conducted on perimenopausal women (12), three ha patients with major depression (14,18,19), one was based on insomniacs with anxiety (23), and the other eight studies were conducted on chronic insomnia patients (11,13,15-17,20-22).
All studies measured the outcome with subjective scale PSQI, except for one article (18), which only had baseline information; the other studies measured the outcome before and after the treatment. Consecutively, four studies (12,17-19) used the subjective scale ISI. Five studies used PSG (12,20) and actigraphy (17-19) as objective outcome indicators. Of all the studies, eight used only the PSQI (11,13-16,21-23) as the outcome indicator, one used PSQI combined with PSG (20), three combined the subjective scales PSQI and ISI with objective tool actigraphy (17-19), and one used PSQI and ISI combined with PSG (12).
A PSQI >7 at baseline was used as a criterion for enrollment of patients in four studies (11,13,20,23), PSQI ≥7 in two studies (14,23), and PSQI >5 in the other three studies (12,15,22). An ISI ≥15 was used as a sleep quality baseline in two studies (17,18), while eligibility criteria were not reported in two studies (16,19).
Regarding the selection of sham acupuncture methods, six studies (11,14-16,20,21) used minimal acupuncture and five studies (12,13,17,22,23) used placebo acupuncture, while two studies (16,19) used both methods.
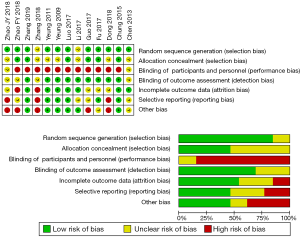
Risk of bias
Risk of bias across the studies in the meta-analysis is summarized in Figure 2. A total of 11 studies (11-15,17-22) used the computer random number table method, while seven (11,12,14,15,18,21,22) introduced the detailed allocation and blinding methods. Owing to the specificity of acupuncture operation, the studies display a high risk of bias at blinded participants and personnel. Except for the three studies (11,16,20) that did not elaborate on the blind method, the rest were blinded to the participants only, and the blinding methods were used to assess the outcomes. All the studies reported the outcomes; two (22,23) had attrition bias, and three (13,20,23) presented reporting bias.
Risk of bias.
Meta-analysis findings
This meta-analysis summarizes the results of 13 RCTs with a total of 1,061 participants. From all the twelve eligible studies (11-17,19-23), there were two did not show a significant change in PSQI score in the experimental groups as compared to the minimal (19) and placebo groups (17). Compared to both minimal and placebo group, one (18) of the four (12,17-19) studies did not show any significant difference in the ISI score in the acupuncture group. One PSG (12) report showed that acupuncture significantly increases the sleep stage N1 and reduces the R stage in comparison with sham acupuncture. Withdrawal due to adverse effects was not reported in any of the reviewed trials.
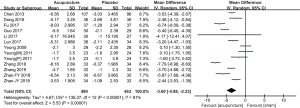
Since all the studies measured the outcome using subjective scale PSQI, except for one article (18) with only baseline information, we combined the score changes from the baseline and the post-intervention scores of continuous variables to assess the unstandardized mean differences (MD), as recommended by the Cochrane handbook for systematic reviews of interventions (10) (MD =−3.60, 95% CI: −4.88, −2.33) (Figure 3).
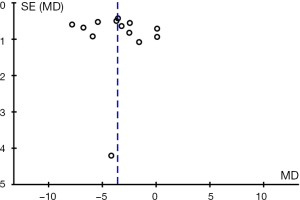
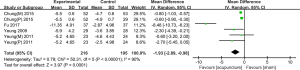
The funnel plot of publication bias (Figure 4) shows that all studies are equally distributed on both sides. However, since that most of the literature was in Chinese and the sample size was not large, we hypothesized a potential publication bias.
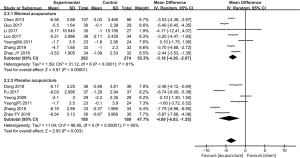
We observed considerable statistical heterogeneity between studies with I2=91%. The sensitivity was analyzed using the one article removed method. After sequential exclusion of each the studies, the results of the effect estimate, I2, P value, and P value for the overall effect did not alter greatly, indicating that the evaluation results of the meta-analysis were stable and reliable. In order to investigate the sources of heterogeneity, we performed prespecified subgroup analyses. First, we focused on the control groups to observe the contribution of minimal and placebo acupuncture to the change in the results (Figure 5). It showed that, irrespective of the type of sham acupuncture, acupuncture can significantly decreased the PSQI score (minimal: MD =−3.18, 95% CI: −4.30, −2.07; I2=81%; placebo: MD =−4.09, 95% CI: −6.83, −1.35; I2=95%). Moreover, the impact of different crowd characteristics of the results was analyzed (Figure 6). A subgroup of two trials with a total of 141 participants with major depressive disorder did not show any significant reduction in the total PSQI scores (MD =−1.65, 95% CI: −3.70, 0.40, I2=76%, P=0.11). The other two subgroups consisted of perimenopausal and anxiety participants in only one trial, and the data was sparse to statistically infer the treatment efficacy.
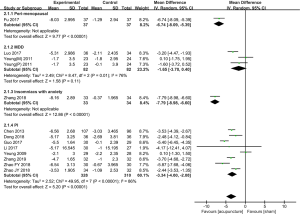
Concurrently, we analyzed the ISI score and the data of objective evaluation indicators: PSG and actigraphy. A total of four trials (12,17-19) with 352 participations showed a significant decrease in the total ISI score while comparing acupuncture with sham acupuncture (Figure 7) (MD =−1.93, 95% CI: −2.89, −0.98; I2=90%). Both PSQI and ISI are subjective sleep evaluation indicators; then, we observed the objective evaluation index PSG and actigraphy (Table 2). Next, the data of PSG (12,20) and actigraphy (17-19) were utilized to select the common sleep indicators for analysis: total sleep time (TST), wake after sleep onset (WASO), sleep efficiency (SE). However, no statistically significant difference was detected in these three sleep indicators (TST, P=0.09; WASO, P=0.32; SE, P=0.47).

Full table
Discussion
PSQI is a self-reported questionnaire used to measure the general sleep quality with a total score >5, indicating insufficient sleep quality (24). ISI is a scale that assesses the severity of symptoms of insomnia and related functional impairment. PSQI and ISI are the primary assessment tools for insomnia that are widely used in clinical and experimental applications (25). According to this meta-analysis, we concluded that both acupuncture and sham acupuncture can reduce the PSQI and ISI scores, and the decrease in the acupuncture group differed significantly as compared to the sham group (PSQI: MD =−3.60, 95% CI: −4.88, −2.33; I2=91%) (ISI: MD =−1.93, 95% CI: −2.89, −0.98; I2=90%). Comparison to the sham group showed an estimated overall reduction of 2.33–4.88 points (11–23%) in the PSQI score, which was considered a clinically meaningful improvement in the sleep quality (26). The subgroup analysis revealed that there was no significant differences in the reduction of the total scores of PSQI between acupuncture and sham acupuncture in the participants with major depressive disorder; this phenomenon might be related to MDD being a severe mental disorder. Both PSQI and ISI are subjective self-rating scales. Therefore, in order to comprehensively evaluate the effects of acupuncture and sham acupuncture on insomnia, we analyzed the research data of objective indicators, PSG, and actigraphy, and selected their common parameters: TST, WASO, SE. However, no significant difference was detected in the changes of TST (P=0.09), WASO (P=0.32), and SE (P=0.47) between acupuncture and sham acupuncture, which might be related to the small sample size.
We also observed that sham acupuncture improves the sleep quality, and its reduction in PSQI or ISI scores may be statistically different, albeit without any clinical effect. Currently, the implementation of real sham acupuncture is controversial globally. There are two main kinds of sham acupuncture used in clinical trials. One is the minimal acupuncture, in which, the needle at non-effective acupoints superficially avoids De qi, and the other is placebo acupuncture which uses retracting needle (mainly including Streitberger and Park) to perform an invasive simulated acupuncture therapy (27,28). Herein, we performed a subgroup analysis of the two sham acupuncture methods and did not detect any marked difference in their contribution to the reduction in PSQI.
Nevertheless, both methods had some limitations. The sticking points in the sham acupuncture consist of the choice of acupoints and the needle insertion methods. Regarding the choice of acupoints, in addition to 362 regular points, there are thousands of extra points all over the body (29), and hence, it is difficult to find a non-effective surface point. In terms of the choice of needle insertion methods, either the superficial or retracting needle stimulates the peripheral nerves. As a result, the corresponding active area of the brain is affected that produces an “edge contact effect,” which is not an inert placebo (30,31). Furthermore, some investigators speculated that De qi indicates a feeling of pain, heaviness, or swelling in patients during acupuncture therapy. However, in addition to the subjective feeling of the patients, the acupuncturists’ feeling under their fingers is also crucial. Some different reinforcing-reducing methods after “De qi” are the major determinants of the therapeutic effect.
Subsequently, the characteristic of acupuncture therapy is that it is not only a simple intervention but the verbal communication and the environmental atmosphere of the diagnosis and treatment process provide the patients with the attached physical and mental treatment (32). This, in turn, can stimulate the reward center of the brain, making the patients comfortable and improving the treatment effect (33,34).
Previous meta-analysis of acupuncture treatment of insomnia primarily analyzed the different acupuncture methods (scalp acupuncture, electroacupuncture, and warm acupuncture) (35) or acupuncture with different control groups (drugs and acupuncture combined drugs) (36). In some meta-analyses, sham acupuncture was also compared in the control group, but only in one of the different control groups (37). The current study compared the acupuncture with sham acupuncture, with a focus on clarifying the placebo effect of acupuncture for insomnia. As a result, the number of articles was more than that retrieved previously.
However, this meta-analysis also had some deficiencies. The number of studies eventually included was small, and due to the language restriction, we only selected Chinese and English databases, which might miss out on some excellent articles published in other languages. Some of those published in Chinese lacked full reporting and varied greatly in terms of RCT designs, treatment protocols, and outcome measures; hence, their results could only be used for the qualitative assessment of the acupuncture effect. Since 3/13 of the included studies did not show any effect, and they were published in English, potential publication bias could attenuate our results. However, while assessing the quality of these studies, we found that the clinical RCT is rather standardized due to the continuous efforts of the clinicians and their contributions to evidence-based medicine.
Conclusions
Taken together, this meta-analysis showed that acupuncture treatment of insomnia might have a placebo effect, but in comparison to the sham acupuncture, the efficacy of the two differed significantly, thereby indicating that acupuncture treatment of insomnia is efficacious. Thus, the placebo effect of acupuncture therapy should be investigated further. Different from the “reverse role” in pharmacological research, the placebo effect of acupuncture was recognized as the therapeutic effect of the acupuncture. It incarnates the psychosomatic co-governance of Chinese medicine and also conforms to modern biological-psychological-social-medical philosophy. For the selection of sham acupuncture, both methods performed similarly in a clinical setting. Moreover, insomnia patients with major depression disorder were not recommended to use only acupuncture treatment.
Acknowledgments
The authors thank Hao Chen MD Lectorate from the Nanjing University of Chinese Medicine for his help in the methodology.
Funding: This study was supported by the Jiangsu Provincial Administration of Traditional Chinese Medicine (grant number: JD201810) and the Jiangsu Provincial Department of Human Resources and Social Security (grant number: WSN-015).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Riemann D, Baglioni C, Bassetti C, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res 2017;26:675-700. [Crossref] [PubMed]
- Shekleton JA, Flynnevans EE, Miller B, et al. Neurobehavioral performance impairment in insomnia: relationships with self-reported sleep and daytime functioning. Sleep 2014;37:107-16. [Crossref] [PubMed]
- Jarrin DC, Alvaro PK, Bouchard MA, et al. Insomnia and hypertension: A systematic review. Sleep Med Rev 2018;41:3-38. [Crossref] [PubMed]
- Bei B, Asarnow LD, Krystal A, et al. Treating insomnia in depression: Insomnia related factors predict long-term depression trajectories. J Consult Clin Psychol 2018;86:282-93. [Crossref] [PubMed]
- Guo J, Wang LP, Liu CZ, et al. Efficacy of Acupuncture for Primary Insomnia: A Randomized Controlled Clinical Trial. Evid Based Complement Alternat Med 2013;2013:163850. [Crossref] [PubMed]
- Yin X, Gou M, Xu J, et al. Efficacy and safety of acupuncture treatment on primary insomnia: a randomized controlled trial. Sleep Med 2017;37:193-200. [Crossref] [PubMed]
- Guo T, Jia M, Jin Y, et al. Acupuncture for perimenopausal insomnia: A systematic review and meta-analysis protocol. Medicine (Baltimore) 2018;97:e11083. [Crossref] [PubMed]
- Dong B, Chen Z, Yin X, et al. The Efficacy of Acupuncture for Treating Depression-Related Insomnia Compared with a Control Group. A Systematic Review and Meta-Analysis. Biomed Res Int 2017;2017:9614810. [Crossref] [PubMed]
- Solomon S. Acupuncture for Headache. It’s Still All Placebo. Headache 2017;57:143-6. [PubMed]
- Tarsilla M. Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Handbook for Systematic Reviews of Interventions. [updated February 2008].
- Chen XH, Li Y, Kui Y, et al. Sleep disorder treated mainly with flying needling therapy: a clinical randomized controlled research. Chinese Acupuncture 2013;33:97-100. [PubMed]
- Chung KF, Yeung WF, Yu YM, et al. Acupuncture for residual insomnia associated with major depressive disorder: a placebo-and sham-controlled, subject-and assessor-blind, randomized trial. J Clin Psychiatry 2015;76:e752-60. [Crossref] [PubMed]
- Dong B, Chen Z Q, Ma J, et al. Clinical Curative Observation of Applying Acupuncture at Yintang (EX-HN3), Baihui (Du20) and Dazhui (Du14) with Periosteal Puncture Method in the Treatment of Primary Insomnia. Sichuan Traditional Chinese Medicine 2018;36:176-8.
- Fu C, Zhao N. Acupuncture Improves Peri-menopausal Insomnia: A Randomized Controlled Trial. Sleep 2017;40:11. [Crossref] [PubMed]
- Guo J, Tang CY, Wang LP. Effect of Tiaoshen Acupuncture Therapy on Sleep Quality and Hyperarousal State in Primary Insomnia. Acupuncture Clinical Journal 2017;33:1-4.
- Li HQ, Zhou YH, Guo J, et al. 30 Cases of Primary Insomnia treated with “Zhou's Acupuncture Method”. Global Traditional Chinese Medicine 2017;17:112-5.
- Luo D, Wu YN, Cai L, et al. Clinical Effect of ShuganTiaoshen Acupuncture on Depression-related Insomnia. Chinese Journal of Gerontology 2017;37:3837-9.
- Yeung WF, Chung KF, Zhang SP, et al. Electroacupuncture for Primary Insomnia: A Randomized Controlled Trial. Sleep 2009;32:1039-47. [Crossref] [PubMed]
- Yeung WF, Chung KF, Tso KC, et al. Electroacupuncture for Residual Insomnia Associated with Major Depressive Disorder: A Randomized Controlled Trial. Sleep 2011;34:807-15. [Crossref] [PubMed]
- Zhang LX, Zhou SY, Zhen QH, et al. Clinical Randomized Control Study of Acupuncture Treatment for Insomnia with Anxiety. World Chinese Medicine 2018;13:1570-4.
- Zhang F, Tang QS, Guo J, et al. Effect of “Old Ten Needles” acupuncture on sleep quality and excessive arousal in patients with chronic insomnia. Chinese Medicine Journal 2019;60:671-4.
- Zhao FY, Zhang ZY, Xia XJ, et al. Memory response to manual acupuncture in chronic insomniacs: evidence from event-related potentials. Journal of Acupuncture and Tuina Science 2018;16:382-8. [Crossref]
- Zhao JY, Wang FC. Effects of acupuncturing Sanyinjiao (SP6) on PSQI and PSG in patients with primary insomnia. Chin J Biotechnol 2018;33:413-6.
- Backhaus J, Junghanns K, Broocks A, et al. Test–retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res 2002;53:737-40. [Crossref] [PubMed]
- Mollayeva T, Thurairajah P, Burton K, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev 2016;25:52-73. [Crossref] [PubMed]
- Waits A, Tang YR, Cheng HM, et al. Acupressure effect on sleep quality: A systematic review and meta-analysis. Sleep Med Rev 2018;37:24-34. [Crossref] [PubMed]
- Tan CW, Christie L, St-Georges V, et al. Discrimination of Real and Sham Acupuncture Needles Using the Park Sham Device: A Preliminary Study. Arch Phys Med Rehabil 2009;90:2141-5. [Crossref] [PubMed]
- White P, Lewith G, Hopwood V, et al. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomised, single-blind, cross-over pilot trial. Pain 2003;106:401-9. [Crossref] [PubMed]
- Liu Y. Zhonghua Qixue Dacheng. Shanghai: Shanghai Science and Technology Literature Publishing House 2001:1.
- Lund I, Näslund J, Lundeberg T. Minimal Acupuncture is not a Valid Placebo Control in Randomised Controlled Trials of Acupuncture: A Physiologist's Perspective. Chinese Medicine 2009;4:1. [Crossref] [PubMed]
- Campbell A. Point specificity of acupuncture in the light of recent clinical and imaging studies. Acupunct Med 2006;24:118-22. [Crossref] [PubMed]
- Liu T. Role of Acupuncturists in Acupuncture Treatment. Evid Based Complement Alternat Med 2007;4:3-6. [Crossref] [PubMed]
- Bausell RB, Lao L, Bergman S, et al. Is acupuncture analgesia an expectancy effect? Preliminary evidence based on participants' perceived assignments in two placebo-controlled trials. Eval Health Prof 2005;28:9-26. [Crossref] [PubMed]
- Lundeberg T, Lund I, Naslund J. Acupuncture - self-appraisal and the reward system. Acupunct Med 2007;25:87-99. [Crossref] [PubMed]
- Xu H, Shi Y, Xiao Y, et al. Efficacy Comparison of Different Acupuncture Treatments for Primary Insomnia: A Bayesian Analysis. Evid Based Complement Alternat Med 2019;2019:8961748. [Crossref] [PubMed]
- Kim SH, Jeong JH, Lim JH, et al. Acupuncture using pattern-identification for the treatment of insomnia disorder: a systematic review and meta-analysis of randomized controlled trials. Integr Med Res 2019;8:216-26. [Crossref] [PubMed]
- Liu F, You J, Li Q, et al. Acupuncture for Chronic Pain-Related Insomnia: A Systematic Review and Meta-Analysis. Evid Based Complement Alternat Med 2019;2019:5381028. [Crossref] [PubMed]