A cross-sectional study on the attitudes and perceptions of outpatients towards palliative care at the Hong Kong Queen Mary Hospital Hospice Centre
Introduction
Background/rationale
According to the World Health Organisation (WHO), palliative care is an approach in medicine that aims to improve the quality of life and care for patients and their families, by helping them to cope with problems associated with life-threatening illness (1). This is achieved by means such as the management of suffering, of pain, as well as of physical, psychosocial, and spiritual health (1). Being multi-disciplinary in nature, palliative care offers a range of services including inpatient, outpatient and home support care. It also involves a multitude of professionals including physicians, physiotherapists, nurse specialists, and social workers, all of whom work together to provide a support system for the patient (2).
Having been recognised as a specialty in Hong Kong since 1998, palliative care has since expanded in the public health sector (2). The city has a unique approach by integrating clinical oncology and palliative care to form a combined specialty, which is supported by the European Society for Medical Oncology (ESMO) program of Designated Centre of Integrated Oncology and Palliative Care (3). Although additional training and resources are needed to face the high demand, such a concept facilitates the seamless incorporation of palliative care for cancer patients. At present, the Department of Clinical Oncology at the Queen Mary Hospital is listed as one of the three ESMO-accredited centres in Hong Kong (4).
The Hong Kong Queen Mary Hospital Hospice Centre (HKQMHHC) runs as part of the Li Ka Shing Foundation “Heart of Gold” Hospice Service Programme (5). This hospice centre is dedicated to offering outpatient palliative care services to cancer patients and represents the Hong Kong West Cluster region (6). Having opened in October 2007, it has developed with a wide range of services including medical consultation, activities for physical and mental development, education seminars, general counselling, and family grief counselling (5).
The importance of palliative care cannot be underestimated. Evidence on patient outcomes suggests that for a population of adults with advanced cancer, early palliative care may improve health-related quality of life slightly and alleviate symptom intensity (7).
Despite Hong Kong’s rapid advancements in palliative care, there are still challenges that need to be addressed, as well as major gaps in the knowledge and understanding of this field locally. Palliative care is still looked upon as luxury and non-essential by both the public and the government, making the process of obtaining more resources for expansion and development a difficult one (2). Additionally, current palliative care services are largely limited to cancer patients (6). Finally, most literature on palliative care is often limited to the perspectives of health officials and professionals, and there is a need to explore the perception from the perspective of patients.
In the Hospital Authority’s “Strategic Service Framework for Palliative Care” recently published, one of the major framework strategies for adult palliative care is to “Enhance palliative care in the ambulatory and community settings to support patients and reduce unnecessary hospitalisation” (6). Hence, in order to appraise palliative care services currently being offered in Hong Kong, it is crucial to consider the views of receiving patients.
Objectives
This study aims to investigate the perspectives of patients receiving palliative care services at the Hong Kong West Cluster Queen Mary Hospital Hospice Centre. Patients receive outpatient services there and are mainly ambulatory.
The primary objective of the study is to examine patient views towards palliative care. In specific, their attitudes on and perceptions of current services and their parameters will be observed. Their knowledge on the definitions of palliative care will be assessed. In looking at their beliefs, their views on the development and progression of care will be noted. We will also focus on whether these services adequately meet patients’ priorities and needs.
We hypothesize that patients’ understanding of palliative care will largely be limited. Given the extensive development on such care in Hong Kong, we predict that the levels of satisfaction in services and care will be high. Furthermore, we foresee a negative relationship between the number and severity of symptoms experienced as well as patient satisfaction.
The outcome of the study is to gain a better understanding of the nature of palliative care services offered in a local setting as seen from the perspective of patients. Such information is used to evaluate the current quality of palliative care services and whether the system required any improvement. Ultimately, this culminates in an overall analysis that may be used for future evaluation and development of palliative care in this specific region in Hong Kong.
Methods
Participants and setting
The present analysis was performed as an observational cross-sectional study. There were no comparison groups allocated, no medical products used, nor any interventions assigned.
Only patients fulfilling these inclusion criteria were included: (I) receiving palliative care services in an outpatient setting at HKQMHHC; (II) able to read, comprehend, and complete the questionnaire having given informed consent. Patients were excluded if they were under 18 years of age, if they were receiving terminal care and physically or mentally incapable to conduct the questionnaire study; and/or if they would be following up at centres and/or clusters for palliative care services other than at the HKQMHHC.
Patients were identified by their attendance at the outpatient clinic at HKQMHHC at the specified time period as stated below. After being approached and assessed for eligibility, they were then informed of the study and asked for informed consent for participation.
Study design
Supplementary details the English and Chinese versions of the questionnaire. The questionnaire consists of 29 questions divided into the following four sections: (A) patients’ backgrounds; (B) knowledge and perceptions of palliative care; (C) objective assessment of symptoms; and (D) attitudes, beliefs, and future direction.
(A) Patients’ backgrounds
Patients’ basic demographic characteristics including age and sex, as well as their experience with palliative care such as duration and frequency of visits to the hospice centre, were documented.
(B) Knowledge and perceptions of palliative care
Their knowledge was assessed by their understanding of which aspects of health palliative care targets. Regarding patient perceptions, they were asked when they thought palliative care should be initiated, as well as whether they believed palliative care was sufficient in Hong Kong.
(C) Objective assessment of symptoms
The Edmonton Symptom Assessment Scale (ESAS) was used to objectively assess patient symptoms (8). It assesses nine symptoms common in cancer patients including pain and nausea; the severity is rated from 0 to 10 on a numerical scale, with 0 being absence of symptom and 10 being that it is of the worst possible severity. This assessment tool was selected for its simplicity, convenience and usage in palliative care patients (9).
(D) Attitudes, beliefs, and future direction
Finally, their attitudes towards the various services offered at the HKQMHHC were evaluated on a scale of 0 to 10 with 0 being extremely inadequate and 10 being extremely adequate. Their priorities of services based on their needs and experiences were also recorded. Open-ended questions such as “What additional services or improvements would you like to see for palliative care at this hospice centre?” were asked to determine how development of palliative care may be shaped in the future.
Data collection
The study was conducted in form of a patient questionnaire. The period of data collection took place over 18 afternoon clinic sessions of Thursdays and Fridays from December 2017 to February 2018 at the HKQMHHC, which is under the Department of Clinical Oncology, Queen Mary Hospital.
Participation in the study consisted of the completion of a single paper-based questionnaire survey. No follow-up was necessary. The questionnaire was distributed to patients and fulfilled either independently or with the assistance of the investigators, depending on the patient’s personal preference. Assistance by investigators denoted that the investigator would read the questions aloud without any additional interpretation, and mark down the patients’ verbal answers.
Data analysis
All completed questionnaires were included in analysis for the study. Data was prospectively collected and inputted into a standardised database, with statistical analysis performed with SPSS (all data will be prospectively collected and input into the IBM SPSS Statistics software package (version 23.0, SPSS < INC, Chicago, IL, USA). Univariate analysis was also conducted, and the distribution, proportion and central tendencies were presented. Correlation was performed with Pearson’s coefficient. Qualitative data was examined with content analysis.
Ethical considerations
The study protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. The IRB reference number is UV17-437. No personal data was collected, and patients’ status of anonymity was maintained. Only authorised persons have access to the data, and the dataset will be destroyed after 2 years.
Results
Patient demographics
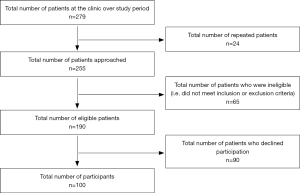
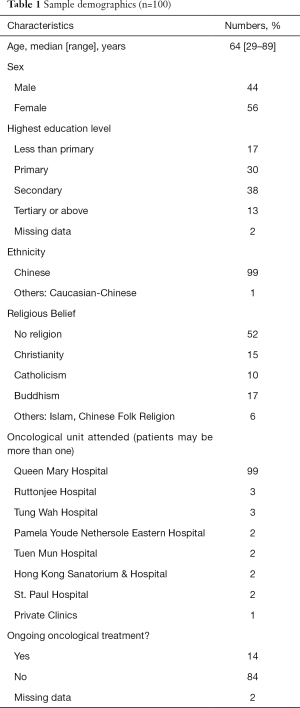
Figure 1 shows a flow chart of the participant selection process in this study. The sample size was 100 participants with a response rate of 52.6%.
The most common cancer types were colorectal (25%), lung (20%) and breast (9%) cancers. These trends are consistent with the pattern of most common cancers in Hong Kong (10). Fifty-one percent respondents had been diagnosed with cancer for more than 5 years; 30% had been diagnosed within 1 to 3 years. Slightly more than half (51%) did not have concomitant medical illnesses, reflecting previous good health (Table 1).
Full table
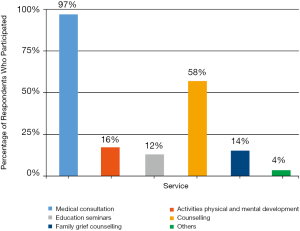
Sixty percent of respondents had received palliative care at the HKQMHHC for less than 2 years, while 19% had done so for more than 5 years. A majority (89%) had regular follow-ups between once every month and once every 3 months, suggesting that this is the usual follow-up frequency at HKQMHHC. Eighty-three percent indicated that the time taken for the referral process to the clinic was within 3 months. In Figure 2 regarding respondents’ participation in various services offered, the two most common were medical consultation (97%) and counselling services (58%). The rest of the services had less attendance: physical and mental development (16%), family grief counselling services (14%), education seminars (12%), other activities including Tai Chi classes and music therapy (4%).
Patients’ knowledge and perceptions
Upon asking respondents which needs they believed palliative care addresses, each respondent answered an average of 1.82 out of the 4 aspects (i.e., physical, psychological, social, and spiritual). Half were able to recognise two or more aspects of palliative care (Figure 3).
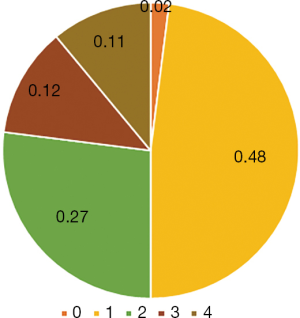
Eighty-seven percent of respondents were able to identify physical needs as a component of palliative care, followed by 51% for psychological needs. Social needs and spiritual needs were only picked by 20% and 24% respectively.
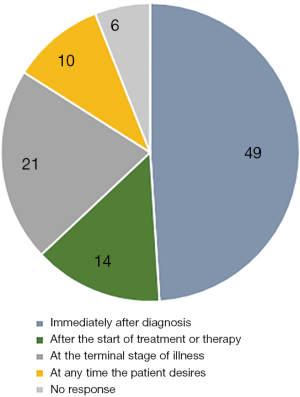
The majority of respondents (88%) first heard of palliative care through doctor referral; only 9% had heard about it from family and friends, and 2% from the internet and media. Forty-nine respondents believed that palliative care should be initiated immediately after diagnosis, followed by 21% who believed that it should be started at the terminal stage of illness (Figure 4).
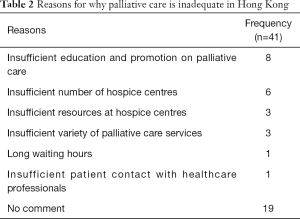
Nearly half the respondents believed that palliative care is sufficient in Hong Kong, while 38% felt that it is not. Table 2 summarises their reasons for this inadequacy.
Full table
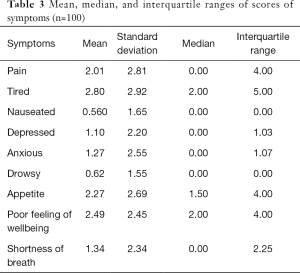
Objective assessment of patients’ symptoms
Based on the ESAS, respondents were asked to score various symptoms experienced in the past 24 hours from 0 to 10, with 0 being no symptom experienced and 10 being most severe. Table 3 shows the average score and score distribution for each symptom. The average score for tiredness was the highest (2.80), followed by poor feeling of wellbeing (2.49), and poor appetite (2.27).
Full table
Patients’ attitudes, beliefs, and future directions
As shown in Table 4, respondents were asked how adequately various aspects of palliative care met their needs on a scale from 0 (extremely inadequate) to 10 (extremely adequate) to reflect their attitudes. Overall, the mean scores for all aspects were over 8. In particular, the aspects of “Staff and healthcare professionals in palliative care” and “Environment and atmosphere of the hospice centre” scored the highest with averages of 8.87 and 8.86, respectively; “Location and convenience of access” had the poorest result. Furthermore, 83% respondents agreed that there is an adequate range of services offered at HKQMHHC.

Full table
Table 5 illustrates the features most enjoyed by respondents; the most common responses were the staff members and their counselling, the positive atmosphere and environment of the centre, and the quality of medical consultations. When asked for suggestions for improvement, 65% expressed that there were no further areas of improvement needed; the suggestions are shown in Table 6.
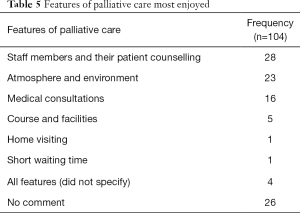
Full table
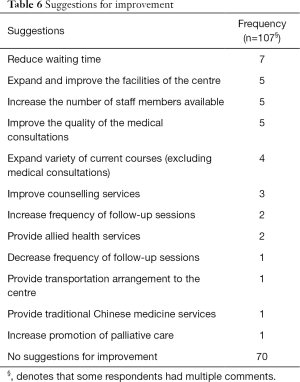
Full table
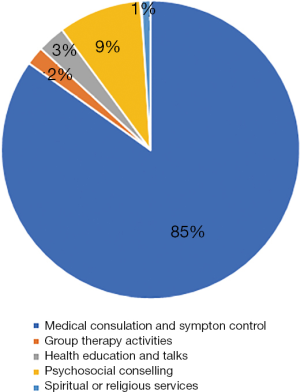
The services offered at HKQMHHC can be expressed as 7 different categories; respondents were asked to prioritise these categories. Figure 5 illustrated the categories which the patient placed as rank one. Majority (85%) placed ‘Medical consultation/symptom control’ as their first priority, followed by ‘Psychosocial counselling’ (9%). Other services were considered less important. Regarding respondents’ preferred form of palliative care service, majority (80%) favoured outpatient services, followed by inpatient (11%) and home visits (9%).
Correlation between symptom intensity and satisfaction for services
In examining possible correlations between factors that were assessed as shown in Table 7, a negative association with a Pearson correlation coefficient of −0.197 (P<0.05) was found between the overall extent of symptoms experienced by patients (i.e., the number and severity of symptoms experienced) and their satisfaction towards services provided.
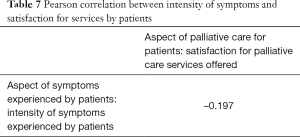
Full table
Discussion
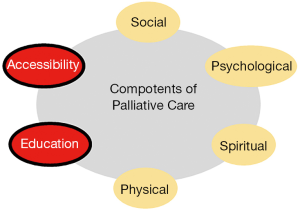
This analysis in a cohort of outpatients receiving palliative care at the HKQMHHC suggested that while patients held generally positive attitudes and perceptions of palliative care, their rather limited knowledge of this topic may have potentially restricted their perspectives to a largely superficial level as most viewed palliative care to be simply targeting physical health with medical consultations. As such, the addition of components such as accessibility and education to Hong Kong’s current system of palliative care are crucial in the betterment of such services for patients.
Patient perceptions towards palliative care
Patients’ attitudes, as shown by their rating of the components of palliative care at HKQMHHC, were extremely positive. All mean scores were over 8, indicating that patients were generally very satisfied. Even the lowest-scoring category, “Location and convenience of access”, had a score of 8.09, with realistic suggestions for improvement concerning increasing the number of hospice centres around Hong Kong and arranging alternative transportation for patients. In interviews, many patients noted the high quality of staff and peaceful, soothing environment; indirectly, such positive aspects may also have favourable effects on patients’ psychosocial state, particularly for those under stress from their health. Furthermore, a striking majority of patients were satisfied with the range of services offered, and half expressed no further improvements needed, which suggests that patients’ needs are met.
Regarding patient perceptions of palliative care, there was a majority of 87% of respondents who identified physical needs as a component of palliative care, indicating that there is great priority placed on bettering patients’ physical wellbeing. On the other hand, only 20% and 24% selected social and spiritual needs respectively, this suggests that there may be lesser priority placed on the latter two aspects, perhaps owing to a lack of awareness on these often-underrated parts of palliative care.
Patients’ knowledge and expectations
The demographics and experiences of this population sample may be linked to their attitudes and perceptions. The large majority of respondents remarked that they had only found out about palliative care from their oncologist who had informed them that the next follow-up session would be at HKQMHHC. During this referral process, there may also have been insufficient explanations to patients on palliative care. These factors could have largely set the tone for patients to view this palliative care centre as a place for regularly monitoring their physical health instead of as one to help cope with all aspects of illness, not just physical. Furthermore, most respondents had already finished their active treatments and were in a stable condition. As such, most did not have active symptoms according to the ESAS, further supporting the idea that their visits to HKQMHHC were purely seen as standard follow-up procedure.
Diversity of palliative services
While there was a high participation rate for medical consultations and counselling services, there were smaller turnouts for other non-medical palliative care services, such as educational and spiritual talks, art workshops, and group outings. As many respondents were of relatively stable health, there may have been less urgency for them to learn about or tend to other aspects of health that palliative care includes. For those who were aware of such services, their non-participation may have been due to several reasons: some respondents expressed they already had adequate social support, some could not participate due to work obligations or inconvenience of time and location. Therefore, of the diverse range of services that HKQMHHC, medical consultation and counselling services had the most participation; it is noted the latter is often initiated by staff at the clinic.
Patients’ symptom intensity
From the ESAS, there was only a small number of patients who had experienced each symptom. As such, the effect of palliative care on symptom management was difficult to determine given the small sample size. There are multiple potential reasons for this phenomenon: (I) patients may already be in a stable state of health, thereby improvements in symptoms from palliative care services may be negligent; (II) palliative care aims to improve illness in the long run; as the ESAS only assesses symptoms active in the past 24 hours, any changes in patient symptoms may not be seen in such a short time period. Nevertheless, external literature has demonstrated vastly improved outcomes associated with outpatient palliative care not only in physical outcomes but also in psychosocial symptoms and quality of life (11-13).
Palliative care service model
The Strategic Service Framework for Palliative Care recently published in 2018 by the Hospital Authority points out four key directions for future development in Hong Kong, which are primarily in line with this study’s results (6). One of the directions is to “Enhance palliative care in the ambulatory and community settings to support patients and reduce unnecessary hospitalization” (6). Given respondents’ attitudes and suggestions for improvement of waiting times and location, progress in this area could greatly target their concerns, especially through expansion of palliative care support to elderly homes and community centres by NGOs and other support groups. Another direction is to “Strengthen performance monitoring for continuous quality improvement” (6), which has been demonstrated by this very study in examining patient perspectives; this may be further expanded to include patients from other clusters for a more well-rounded view. Finally, the generally positive attitudes that patients hold towards HKQMHHC largely support the remaining two directions of the framework, which are to “Enhance governance by developing cluster-based services with the collaboration of medical and oncology palliative care specialists” as well as to “Promote collaboration between palliative care and non-palliative care specialists through shared care model according to patients’ needs” (6). Since patients feel positively about the services currently being offered, this may be a favourable sign for palliative care to be expanded to various hospitals in different clusters, as well as non-oncological patients. Such care could also be integrated at the early stages of illness which is in line with patients’ desires for earlier initiation of palliative care.
Correlation between symptom intensity and satisfaction for services
Additionally, the newfound discovery of the relationship between extent of symptoms experienced and patients’ satisfaction towards services provided is a new direction for future study. These two components are crucial aspects to consider for patient care and can be further explored, such as whether satisfaction of services provided may causally improve their symptoms experienced. If there is a causal relationship present, this may support policies with greater emphasis on the provision of high-quality services for symptom alleviation in order to achieve a better clinical outcome.
Future directions for palliative care in Hong Kong
The findings from this study have reflected a need for patients to explore other aspects of palliative care apart from simply physical needs. From interviewing the outpatients at HKQMHHC, many reflected their wishes to expand the horizons of palliative care; specifically, of the patients who felt that palliative care was inadequate in Hong Kong, the most common reason given was “Inadequate education and promotion”. As well, accessibility to palliative care services is currently quite limited as they are only offered to oncology patients. Therefore, the components of education and accessibility are proposed as additions to the current model of palliative care in Hong Kong as illustrated in Figure 6.
Considering the WHO model of palliative care, the following specific improvements are suggested to further enhance palliative care; their positions in the model are shown in Figure 7:
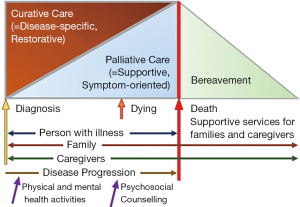
- More comprehensive and accessible promotion and education within the greater community, via means such as social media;
- Increased coverage of palliative care centres, such as more outpatient satellite clinics in each cluster to facilitate convenience of access to patients;
- Continued spectrum of services aside from medical consultation, such as psychosocial counselling, health education discussions, and group therapy activities.
Study strengths and limitations
One of the greatest strengths of this study was the collection of both objective and subjective feedback from individual patients through the questionnaire survey, which allowed more comprehensive review of patients’ perspectives. Additionally, this topic has not been explored sufficiently for this population and setting, and so the study’s findings may prove to be useful for future health developments in Hong Kong.
Retrospectively, there were multiple limitations to the study. Selection bias was potentially introduced by the location and the specific time periods of data collection. Data collection took place during the 18 afternoon clinic sessions on Thursdays and Fridays at the HKQMHHC. The limited time periods at only one of the eight clinics offering palliative care may not accurately reflect the views of the entire population of patients in Hong Kong. In the future, both outpatients and inpatients may be considered for participation to reflect the different types of patients receiving palliative care. More diverse time periods at multiple centres offering such care could be used for data collection. Additionally, there may have been potential recall and reporting biases by participants. Although it was clarified that this study was performed independently to the clinic, patients may not have been accurately reflected their perspectives, regardless of whether this was intentional or not, such as understating or omitting complaints about the centre’s palliative care services. Furthermore, some patients had limited understanding of their own medical history, which may have resulted in further inaccuracies in the data. To improve, investigators may consider cross-checking each participant’s electronic patient record to ascertain basic patient profile.
Conclusions
In conclusion, this study has shown that a great majority of outpatients currently receiving palliative care perceive the physical aspect of care, including medical consultations, to be the most important; they also have highly positive attitudes towards the services experienced. Patients’ lack of comprehensive understanding towards the definition and goals of palliative care may be attributed to the lack of promotional and educational activities through accessible means such as social media. As such, the newly proposed palliative care model has incorporated the aspects of accessibility and education, as well as the early introduction of comprehensive care such as psychosocial counselling and physical and mental activities, as essential parts of palliative care to better help patients cope with illness.
Acknowledgments
We would like to acknowledge the Department of Clinical Oncology, Queen Mary Hospital, for their kind permission to conduct the study in the Queen Mary Hospital Hospice Centre. We also acknowledge the staff from the Queen Mary Hospital Hospice Centre for their kind assistance during the data collection process at the centre. We acknowledge Mr. John Fong for his assistance in statistical data processing. Last but not least, we extend thanks to Dr. Michael Ni, Dr. Felix Cheung and Mr. Eric Chen from the School of Public Health for their advice and support.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Rebecca Yeung and Tai Chung Lam) for the series “Integrating Palliative Medicine in Oncology Care: The Hong Kong Experience” published in Annals of Palliative Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/apm.2019.10.06). The series “Integrating Palliative Medicine in Oncology Care: The Hong Kong Experience” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the Institutional Review Board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster. The IRB reference number is UV17-437. Individual informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- WHO Definition of Palliative Care. World Health Organization. 2019. Accessed 1 Jan 2019. Available online: http://www.who.int/cancer/palliative/definition/en/
- Subcommittee in Palliative Medicine, Hong Kong College of Physicians. Palliative Care: Setting the scene for the future. Hong Kong College of Physicians. 2008. Available online: http://www.hkcp.org/docs/News/Position paper in Palliative Medicine.pdf
- Yeung R, Wong KH, Yuen KK, et al. Clinical oncology and palliative medicine as a combined specialty--a unique model in Hong Kong. Ann Palliat Med 2015;4:132-4. [PubMed]
- ESMO Designated Centre of Integrated Oncology and Palliative Care. Queen Mary Hospital, Hong Kong S.A.R., China | ESMO. 2019. Accessed 2 Jan 2019. Available online: Queen-Mary-Hospital-Hong-Kong-S.A.R
- Li Ka Shing Foundation “Heart of Gold” National Hospice Service Programme. Hospice Home. 2013. Available online: http://www.hospicehome.hk/aboutHospice.php?lang=ENG. Accessed 2 Jan 2019.
- Strategic Service Framework for Palliative Care. Hospital Authority. 2018. Accessed 1 Jan 2019. Available online: http://www.ha.org.hk/haho/ho/ap/PCSSF_1.pdf
- Haun MW, Estel S, Rücker G, et al. Early palliative care for adults with advanced cancer. Cochrane Database Syst Rev 2017;6:CD011129. [Crossref] [PubMed]
- Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care 1991;7:6-9. [Crossref] [PubMed]
- Richardson LA, Jones GW. A review of the reliability and validity of the Edmonton Symptom Assessment System. Curr Oncol 2009;16:55. [PubMed]
- Overview of Hong Kong Cancer Statistics of 2015. Hospital Authority. 2017. Accessed 2 Jan 2019. Available online: http://www3.ha.org.hk/cancereg/pdf/overview/Summary%20of%20CanStat%202015.pdf
- Zimmermann C, Swami N, Krzyzanowska M, et al. Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 2014;383:1721-30. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Yennurajalingam S, Atkinson B, Masterson J, et al. The impact of an outpatient palliative care consultation on symptom burden in advanced prostate cancer patients. J Palliat Med 2012;15:20-4. [Crossref] [PubMed]
- WHO Guide for Effective Programmes: Cancer Control - Knowledge into Action. World Health Organization. 2007. Accessed 1 Jan 2019. Available online: https://www.who.int/cancer/media/FINAL-PalliativeCareModule.pdf