
Clinical parameters of wound healing in patients with advanced illness
Introduction
Patients with advanced illnesses are at high risk for pressure injuries because of their increased dependency and deteriorating clinical condition. Pressure injuries are also common clinical parameters of patient care outcomes in hospital and community care. Many factors increase the risk of patients with advanced illness to pressure injuries and difficult wound healing. Despite careful wound management, the pressure wounds of patients with advanced illness are more difficult to heal compared with those of patients with relatively good physical condition (1). Pressure injuries are always a problem in palliative care because the suffering of patients is intensified, their quality of life is reduced and healthcare costs are increased (2).
Factors affecting wound healing
Pressure injury results from prolonged pressure exerted on human tissue, causing tissue breakdown. Pressure injuries are categorised into different stages. Stage 1 describes any area of persistent skin redness or discoloration; stage 2 includes the partial loss of skin layers, a pink, shallow but open wound bed or an open or ruptured pus-filled blister; stage 3 is characterised by deep craters on the skin, whereby subcutaneous tissue may be observed; stage 4 typifies muscle or bone exposure; and unstageable shows full thickness or tissue loss, in which the wound base is covered by slough or eschar (3,4).
Circulation, oxygenation, mechanical stress, temperature, humidity, infection, chemical stress on wounds, medications, disease, alcohol, smoking, nutrition, age and body build are common risk factors of pressure injuries (4,5). In terminally ill patients, a majority of these risk factors are unavoidable, and their physical condition becomes irreversible.
Goal of care and care plan
The quality of life and wound healing probability are decreased in patients with advanced illnesses (6). Pressure injuries that occur near the end of life are often not preventable, and efforts to prevent them are complicated because of the frail condition of such patients (7). Most health care professionals participate in a system involving quality and safety management and benchmarking with different hospitals. People still focus on wound healing as a treatment choice rather than fulfill the other needs of patients, which not only causes frustration of the patient, family members and health professionals but also increases patient discomfort and treatment costs (8).
Hughes et al. (6) suggested three common wound care directions for patients with advanced illnesses: (I) treatment that must be provided; (II) treatment that must not be provided; and (III) treatments that vary depending on the needs and condition of the patient. Treatment must not be provided if the competent patient refuses the treatment, the treatment is considered futile or clinically inappropriate or the burden of treatment outweighs potential benefits.
Palliative health workers reported that a lack of prognostic indicators is one of the common difficulties in initiating clinical triggers for shifting the goal of care. As health care workers and family members tend to overestimate the wound healing probability of their patients, the opportunity to identify an appropriate, realistic goal of care for patients and their families may be lost.
Purpose of this study
This study aimed to identify the relationships between the functional status, systemic factors and wound condition of patients and the healing probability of pressure injury in palliative care in-patient setting. Identifying the association specific to palliative care patients is important for goal setting and care plan formulation. The findings of this study may help to improve the quality of life of patients and reduce the stress of family members by providing appropriate care and emotional support.
Methods
Study design
A descriptive study was conducted through retrospective analysis of the clinical records of patients with advanced diseases by reviewing patient documents. Patients with pressure injuries admitted from July 2014 to December 2015 were included in the study. The study sample included all palliative care in-patients with pressure injury upon admission. Data analysis was performed using SPSS Version 23.
Inclusion criteria
- Patient age ≥18 years;
- Suffering from at least one advanced illness;
- In-patient of the Palliative Medical Unit of the study hospital within July 2014–December 2015;
- Presence of at least one pressure injury during the above period of hospitalization.
Exclusion criteria
- Presence of only fungating wounds.
Data collection
Apart from the demographic data of the patients, a palliative performance scale (PPS) was used to measure the functional status of each patient. Norton scale, which evaluates the risk of developing pressure injuries, healing probability assessment and pressure ulcer healing scores were determined for the prediction of wound healing.
PPS
The PPS is a tool for measuring performance status in palliative care. It provides a common language on performance status for the concise reporting of functional status, which aids in communication among palliative healthcare workers. PPS ranges from 0% to 100%, according to the best fit of five areas, namely, ambulation, activity and extent of disease, self-care, oral intake and conscious level. A score of 0% indicates death, whereas 100% corresponds to full ambulation, normal activity and work, no evidence of disease, full self-care, normal intake and full consciousness. Decrease in scores may indicate a progressing condition (9).
Norton scale
The Norton pressure sore risk-assessment scale scoring system is a tool for estimating the risk of a patient for developing pressure ulcers. The Norton score for pressure ulcer risk calculator comprises five parameters relevant to skin condition, with each parameter involving various choices weighing a different number of points. Those parameters include physical condition, mental condition, activity, mobility and incontinence. The score ranges from 5 (maximum risk) to 20 (minimum risk). The lower the score, the higher the risk. Scores <14 and ≥14 indicate a high risk and a relatively low risk of pressure injuries, respectively (10).
Healing probability assessment
The healing probability assessment tool provides a foundation for estimating the probability of success in aggressive local intervention for closing any skin wound. A total of 20 unfavourable factors of wound healing are included. The greater the number of checked items, the lesser the likelihood for wounds to achieve a sustainable complete closure (11).
Pressure ulcer healing score
The pressure ulcer healing score categorises an ulcer with respect to surface area, exudate and wound tissue type by recording a sub-score for each of these ulcer characteristics. The sub-scores are added to obtain a total score from 0 to 17. Increasing scores may indicate a progressing condition (12).
Other systemic factors, including white blood cell count and haemoglobin, glucose, albumin, creatinine, urea, bilirubin and alanine aminotransferase (ALT) levels, were reviewed if data were available.
Data analysis
Descriptive measures of demographic information were calculated. Spearman’s correlation coefficient was used to measure the relationship among demographic data, risk of injury, healing factors and systemic factors.
Results
Characteristics of participants
The study was approved by the Institutional Review Board of the involved hospital. A total of 127 clinical records of patients with pressure injuries during the period of 18 months were analyzed. Eligible patients were those with incurable illnesses and pressure injuries during hospitalisation.
In retrospect, more than half of the participants (50.8%) died within 17 days from the time of the first assessment. The length of survival from the first assessment date ranged from 2 to 289 days. The mean length of survival was 29.42±36.80 days. The majority (92, 72.4%) of patients died within the same episode of admission, 30 (23.6%) possessed unhealed wounds upon discharge and only 5 (3.9%) exhibited healed wounds before discharge.
Demographic characteristics
Among all participants, their ages ranged from 40 to 97 years. The majority of patients were diagnosed with cancer, whereas the rest suffered from end-stage organ failure and degenerative illnesses. More than half of the patients were transferred from an acute hospital, nearly one-fourth were transferred from convalescent hospitals, and the rest of the them were admitted mainly from home and old-age homes.
The retrospective review involved the evaluation of PPS during the initial assessment upon admission and showed that the majority of patients exhibited 30–40% PPS, which indicates that this group of patients spent most of the time in bed with increasing debility and requirement for total care. Moreover, the rest of most patients demonstrated 10–20% PPS, reflecting that this group of patients were very ill and were fed only through sips of oral intake. Details on the characteristics of patients with pressure injuries upon admission are shown in Table 1.
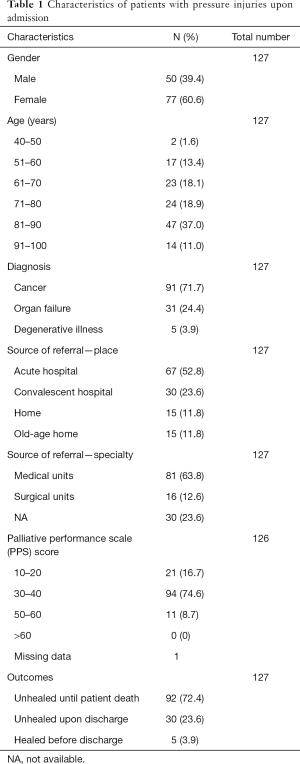
Full table
The most common location of wound injures were the sacrum or coccyx areas, followed by the iliac crest, hip or ischial tuberosity areas and ankle or heel areas. The rest were found in separate pressure points. Details on the characteristics of patients with pressure injuries upon admission are shown in Table 2.
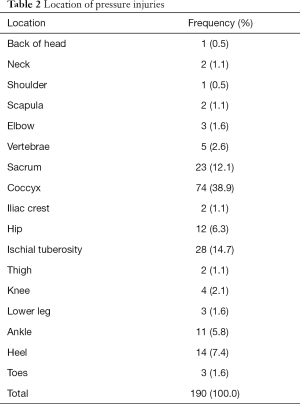
Full table
The total number of wounds per patient ranged from 1 to 9. Only one or two wounds were found in majority of patients. The mean number of wounds per patient was 1.57±1.12.
Two-third of the patients suffered from stage 2 pressure injury, whereas other patients exhibited various staging and even unstageable pressure injury. The size of wounds ranged from tiny to huge. Details on wound characteristics are shown in Table 3.
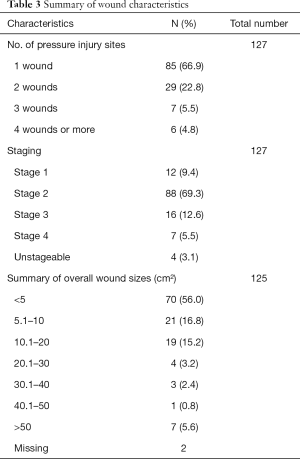
Full table
Relationship among demographic data, risk of injury and healing factors
Spearman’s correlation coefficients (Table 4) revealed that healing probability was significantly positively correlated with age (r=0.348, P=0.000) and negatively correlated with PPS score (r=−0.486, P=0.000) and Norton score (r=−0.427, P=0.000). Moreover, Norton score was positively correlated with PPS (r=0.589, P=0.000) and negatively correlated with age (r=−0.241, P=0.006) and healing score (r=−0.258, P=0.004). Wound staging was positively correlated with pain (r=0.283, P=0.001) and healing score (r=0.507, P=0.000) and negatively correlated with Norton score (r=−0.217, P=0.015). Other demographic data were unrelated to the risk of injury and healing factors of the patients.
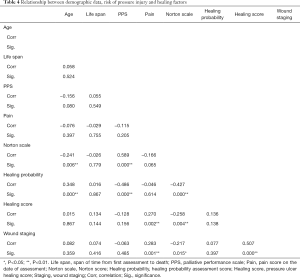
Full table
Relationship between demographic data and systemic factors
Spearman’s correlation coefficients (Table 5) revealed that haemoglobin level was significantly positively correlated with albumin level (r=0.308, P=0.001) and negatively correlated with creatinine level (r=−0.242, P=0.010). Urea level was positively correlated with creatinine level (r=0.647, P=0.000) and negatively correlated with PPS score (r=−0.223, P=0.017). ALT level was positively correlated with bilirubin level (r=0.310, P=0.001) and negatively correlated with age (r=−0.207, P=0.028). Creatinine level was also positively correlated with saturated oxygen level (r=−0.199, P=0.042).
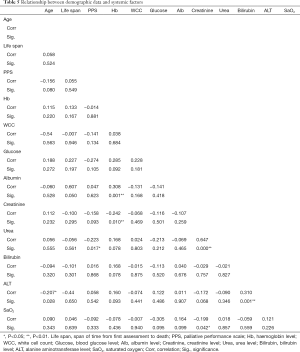
Full table
Spearman’s correlation coefficients also showed positive correlation between healing probability and creatinine level (r=0.230, P=0.015).
The results showed that the PPS, Norton, healing probability assessment and pressure ulcer healing scores deteriorated when patients were approaching death. The overall mean values of PPS, Norton, healing probability and ulcer healing scores of patients upon admission were 33.70%±10.09%, 11.39±2.10, 9.77±2.46 and 8.27±4.13, respectively. In retrospective review, patients obtained decreased PPS and Norton scores and increased healing probability assessment and pressure ulcer healing scores during the last week of life (Table 6).
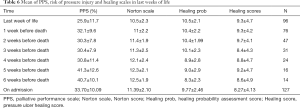
Full table
Discussion
Pressure wound care is complicated in palliative care patients owing to their advanced illnesses. Maida et al. (13) found that young age and increased PPS score are associated with both complete healing before death and prolonged survival. In the current study, the healing probability assessment score was positively correlated with age and creatinine level and negatively correlated with PPS and Norton scores. Pressure ulcer healing score was positively correlated with wound stage and negatively correlated with Norton scores. Wound staging was positively correlated with pain and negatively correlated with Norton scores. The results concur with the findings of Langemo (14), who found that the skin of patients is vulnerable to breakdown and less able to heal in the palliative care setting. The findings of the current study showed that patients exhibiting old age, high creatinine level, advanced wound stage, reduced PPS and low Norton score, which indicates a high risk of pressure injuries, are prone to possess unhealed wounds.
Goals of care
A majority of palliative care patients are at a very high risk of pressure-induced skin damage that is difficult to heal because most of the unfavourable factors are commonly found in patients with advance illnesses. According to Brink et al. (3), pressure injuries be can one of the visible indicators and consequence of further deterioration of patient condition rather than the ineffective outcome of basic nursing care. Aggressive interventions always increase the cost of care and reduce the quality of life (6) by further increasing the severity of pain and prolong patient’s suffering. For example, ineffective debridement only escalates the painful experiences without improving wound condition. Some people may boost up patient’s nutritional status by artificial feeding, but patient’s circulation & absorption doesn’t improvement. Furthermore, enteral feedings at the end of life increase gastrointestinal adverse symptoms (15). In non-healing wounds, aggressive interventions that focus on wound healing may no longer be appropriate.
Patients may experience wounds that are difficult to treat and may not be responsive to healing near the end of life (16). Health care professionals and the family members of patients may feel guilt and a sense of failure when the wound condition of patients shows no improvement or even further deteriorates. When wound healing becomes impossible, the goal of care must shift from curative to palliative treatment. The goals of palliative treatment of wounds at the end of life include managing exudate, controlling odour, maximizing mobility and function, preventing infection and controlling pain and other symptoms (16,17). Holistic care and symptom management helps improve the sense of control of patients and emotionally prepares them for changes in their condition and the possibility of further deterioration.
Care for dying patients
Prior to the death of patients, body systems and blood circulation usually begin to shut down within the last 2 weeks. Changes in the PPS score of patients represent additional independent predictors of survival (6,18). The results of this study demonstrate that low PPS, low Norton scores, poor healing probability and high-pressure healing ulcer scores in patients during their last 3 weeks of life are commonly found. It shows that patients with low PPS with progression pressure injury and high-pressure healing scores are prone to have poor healing probability and near the end of their life. This finding provides healthcare professionals with general ideas on when to shift the focus of care to symptom control and prepare patients and their families on the possibility of further deterioration and impending death rather than spending effort on ineffective treatment for wounds that cannot be healed.
Wound pain is one of the common factors affected patient’s quality of life. Comprehensive wound assessment, adequate pain control, use of appropriate dressings and professional manner can improve the patient’s tolerance to wound pain (19). Prevent maceration of surrounding skin by controlling wound exudates with absorbent dressing, such as, foams or hydrocolloid dressings are important to prevent further damage of the surrounding tissues (20). Unpleasant odour not only affects the smelling sense, but also patient’s self-image. Topical gel or ointment, e.g., metronidazole & charcoal are commonly use in palliative care setting for wound odour control (21,22). For the environment, an effective deodorizer would be considered. Apart from the above measures, skillful dressing technique and wise use of appropriate dressing materials can help to improve patient’s general comfort, sense of security and increase mobility. Appropriate psychological support and nursing care in holistic approach should be provided at the same time.
Implications for practice
Pressure injuries occurring at the end of life are often unavoidable because the condition of patients is usually too frail (7). Once pressure wounds are identified in the presence of undesirable factors, such as old age, high creatinine level, advanced wound stage and reduced PPS and Norton scores, preparing patients and their families to accept the situation, establishing realistic expectations and reducing the guilt and sense of incompetence of caregivers are crucial. Using the clinical parameters identified in this study may help healthcare professionals discuss realistic goals of care along with appropriate treatment plans (13). The fact that pressure injury development may be a consequence of declining health and dying process instead of failure must be explained. Frontline nurses must be educated about the common clinical parameters which indicate an increased probability of unhealed wound, and methods to address the emotional needs of patients and their families are highly important.
Reasonable treatment options can be outlined by focusing on realistic outcomes in light of advanced disease (16). When wound healing ceases to be the aim of care, the comfort, skin condition related to erythematous maceration and skin stripping from dressing, peri-wound irritation, presence of necrotic tissue, leakage of exudate and odour of patients will be the focus of physical care in wound management (17,23). By facilitating patients and their family members to have smooth transition into a care plan with a palliative approach, the personal goals and quality of life can be maximised in the remaining time of the patients.
Apart from physical care and the psychological preparation of patients and their families, developing practical clinical guidelines to ensure standard care in daily application is important in order to guide nursing colleagues to provide holistic and effective care to patients with unhealed wounds. This approach can help in balancing the choice of treatments between aggressive treatment and comfort care.
Limitation and recommendation
This study specifically focuses on patients with pressure injury upon admission in hospice and palliative care setting. The applicability of the findings to other patients with palliative care needs who are still under care in an acute setting is uncertain. The recruitment of patients in early stage with increased PPS may help to achieve a clear picture of the relationship between wound healing and clinical parameters. The study is limited by the retrospective use of cross-sectional data. Thus, the use of prospective design for future research must be considered.
Conclusions
The aim of palliative care is to achieve the best quality of life for patients with debilitating disease. When the aim of care is no longer curative, the goal of care must be focused on symptom control and comfort care. This study provides an idea of the clinical parameters of wound healing in palliative care patients in local hospice setting. Pressure injuries are prone to non-healing in patients with old age, high creatinine level, advanced wound stage, low PPS and low Norton scores. In such situation, the focus of care must be shifted from curative to symptom management, which includes managing exudate, controlling odour, maximizing mobility and function, preventing infection and controlling pain and other symptoms.
Healthcare professionals need to facilitate the families of patients in performing meaningful events with patients to improve their quality of life near their death. Further prospective studies involving patients in early stages can help to achieve a clear understanding of the situation, which may help develop evidence-based guidelines for unhealed wound management in holistic aspects at the end of life care.
Acknowledgements
The authors wish to thank Ms. WL So, Ward Manager, and colleagues of Palliative Medical Unit of Grantham Hospital for their work on data collection.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of HKU/HA HKWC (No. UW 16-261).
References
- Alvarez OM, Kalinski C, Nusbaum J, et al. Incorporating wound healing strategies to improve palliation (symptom management) in patients with chronic wounds. J Palliat Med 2007;10:1161-89. [Crossref] [PubMed]
- The American College of Wound Healing & Tissue Repair, and the Angiogenesis Foundation. Patient-centered Outcomes in wound care. Massachusetts: The Angiogenesis Foundation, 2013.
- Brink P, Smith TF, Linkewich B. Factors associated with pressure ulcers in palliative home care. J Palliat Med 2006;9:1369-75. [Crossref] [PubMed]
- Yuska C. Understanding risk factors in pressure ulcer development and wound healing. healthVIE.com 2010;2:86-92. Available online: https://www.medline.com/media/assets/pdf/Understanding-Risk-Factors-in-Pressure-Ulcer-Development-and-Wound-Healing.pdf
- Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res 2010;89:219-29. [Crossref] [PubMed]
- Hughes RG, Bakos AD, O'Mara A, et al. Palliative wound care at the end of life. Home Health Care Management and Practice 2005;17:196-202. [Crossref]
- Langemo DK, Black J. National Pressure Ulcer Advisory Panel. Pressure ulcers in individuals receiving palliative care: a National Pressure Ulcer Advisory Panel white paper. Adv Skin Wound Care 2010;23:59-72. [Crossref] [PubMed]
- Fife CE, Carter MJ. Wound Care Outcomes and Associated Cost Among Patients Treated in US Outpatient Wound Centers: Data From the US Wound Registry. Wounds 2012;24:10-7. [PubMed]
- Anderson F, Downing GM, Hill J, et al. Palliative performance scale (PPS): a new tool. J Palliat Care 1996;12:5-11. [PubMed]
- Norton D, McLaren R, Exton-Smith AN. An investigation of Geriatric Nursing Problems in the Hospital. London: Churchill Livingstone, 1962.
- Frail Palliative Wound care. Palliative Wound Care and Healing Probability Assessment Tool, 2009. (accessed on 12.12.17). Available online: http://www.frailcare.org/images/Palliative%20Wound%20Care.pdf
- National Pressure Ulcer Advisory Panel. The Pressure Ulcer Scale for Healing (PUSH Tool), 1998. (accessed on 09.12.17). Available online: http://www.npuap.org/resources/educational-and-clinical-resources/push-tool/
- Maida V, Ennis M, Kesthely C. Clinical parameters associated with pressure ulcer healing in patients with advanced illness. J Pain Symptom Manage 2014;47:1035-42. [Crossref] [PubMed]
- Langemo DK. When the goal is palliative care. Adv Skin Wound Care 2006;19:148-54. [Crossref] [PubMed]
- Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol 2014;20:8505-24. [Crossref] [PubMed]
- Letizia M, Uebelhor J, Paddack E. Providing palliative care to seriously ill patients with nonhealing wounds. J Wound Ostomy Continence Nurs 2010;37:277-82. [Crossref] [PubMed]
- Browne N, Grocott P, Cowley S, et al. Woundcare Research for Appropriate Products (WRAP): validation of the TELER method involving users. Int J Nurs Stud 2004;41:559-71. [Crossref] [PubMed]
- Chan EY, Wu HY, Chan YH. Revisiting the Palliative Performance Scale: change in scores during disease trajectory predicts survival. Palliat Med 2013;27:367-74. [Crossref] [PubMed]
- Brown A. Strategies to reduce or eliminate wound pain. Nurs Times 2014;110:12-5. [PubMed]
- Cutting KF, White RJ. Avoidance and management of peri-wound maceration of the skin. Prof Nurse 2002;18:33-35-36. [PubMed]
- Paul JC, Pieper BA. Topical metronidazole for the treatment of wound odor: a review of the literature. Ostomy Wound Manage 2008;54:18-27. [PubMed]
- Swezey L. Wound Odor Management: Charcoal wound dressings. Wound Source. (accessed on 06.12.18). Available online: https://www.woundsource.com/blog/wound-odor-management-charcoal-wound-dressings
- Woo KY, Krasner DL, Kennedy B, et al. Palliative wound care management strategies for palliative patients and their circles of care. Adv Skin Wound Care 2015;28:130-40. [Crossref] [PubMed]


