Traditional Chinese medicine in the treatment of symptoms in patients with advanced cancer
Introduction
The various malignant tumors can occur at different locations and result in complicated conditions in their advanced stages. About 80% of cancer patients are diagnosed at advanced stages and therefore are not eligible for surgery or radio-chemotherapy. Advanced cancer patients will experience physical wasting; also, due to the effect of vicious toxins, the patients can develop systemic metabolic disorders and then cachexia. Along with the invasion and distant metastasis of tumors in the surrounding tissues and organs, the patients can develop various complicated symptoms, which can even be fatal. From the perspective of TCM, tumor is not only the morphological changes of a specific tissue or organ but also, and more importantly, the functional changes of tissues or organs. The pathological changes of tumors are clinically presented as dampness, toxin, phlegm, stasis (obstruction), and deficiency. Therefore, from the perspective of TCM, the mechanism of tumor can be summarized as: stagnation of toxin and heat, obstruction of phlegm/dampness, Qi stagnation and blood stasis, and imbalanced yin and yang in viscera and bowels. Patients often have the dysfunction of viscera and bowels (e.g., deficiency in liver, spleen, and kidney) and deficiency of the original qi. In addition, pathological changes can also occur due to the emotional impairment. The imbalance between yin and yang in viscera and bowels can be particularly obvious in patients with advanced cancers. According to the ancient Chinese physicians, the development of tumors is often associated with the dysfunction of viscera and bowels, particularly the spleen and kidney deficiencies. Kidney is the root of innate endowment, and spleen is the root of acquired constitution. Spleen and kidney deficiencies can result in the weak healthy qi, and the insufficient defense qi can not prevent the invasion of pathogen. If the healthy qi can not effectively eliminate the pathogen, it will easily spread inside body. As mentioned in the classic books, “When there is sufficient health qi inside, the pathogenic qi have no way to invade the health body”; or, “Where pathogenic factors accumulate, the parts of the body must be deficient in the vital-qi”.
TCM has a long history and rich experiences in treating malignancies. The initial step is to enhance the healthy qi, so as to improve tumor-bearing survival by preventing disease progression and alleviating symptoms. The largest difference between TCM and modern medicine in terms of efficacy is: after TCM treatment, the tumor does not shrink remarkably, but the patient has longer survival and dramatically improved subjective symptoms; after treatment with modern therapies, on the contrary, the tumor may obviously decrease in size but can recur rapidly, along with unprolonged survival and impaired quality of life. TCM is based on holism, focusing on the macro-regulation of the patient’s physiological functions. Pattern identification is a featured and essential concept in TCM. In fact, it refers to the identification of the internal environment of an imbalanced human body. The fundamental purpose of TCM treatment for tumors is to restore the balance of the internal environment by adjusting the internal environment, enhancing the anti-pathogen capability, so as to inhibit the growth and metastasis of tumors (1). It is particularly important to replenish the healthy qi and strengthen the body resistance for patients with advanced malignancies. On the basis of pattern identification, it is important to use traditional Chinese drugs that are capable of reinforcing the healthy qi, strengthening the body resistance, and treating wasting/deficiency to adjust the yin/yang/qi/blood of human body and the physiological function of organs and meridians, so as to improve the quality of life, enhance the inherent disease resistance, adjust immune function; by doing so, the TCM treatment may help the cancer patients to strengthen the general conditions, remove the disease/pathogen, inhibit tumor progression, alleviate symptoms, and prolong survival (2).
Patients seeking for TCM treatment are often in the advanced stages or have experienced relapses, and often have already received surgical treatment and multiple radio-chemotherapies. For these patients, any treatment is not able to eliminate the tumors. The treatment priorities have become how to relieve the patient’s pain, improve quality of life, and prolong survival. A prolonged survival should be based on the improved quality of life. Without satisfactory quality of life, the so-called “prolonged survival” has limited value. While the vast majority of patients with advanced malignancies have strong desire to survive, they suffer from both physical and psychological pain during the treatment. These patients often suffer from deficient vital Qi, which is clinically presented as cancer-related pain, anorexia, nausea/vomiting, fatigue, fever, indigestion, and constipation, which severely lower the quality of life and even shorten the survival of these patients. Fortunately, TCM has shown good efficacy in symptomatic treatment. In this article, we will discuss the role of TCM treatment in alleviating three major symptoms and improving the overall quality of life in patients with advanced malignancies; also, we will elucidate the TCM-based emotional care for these patients.
Cancer symptoms in TCM
Cancer symptoms in TCM refer to the pain or discomfort felt by the patients themselves and the signs/conditions that can be identified after examinations. The “symptom” is the individual objective phenomenon arising from and accompanying a disease or other pathological condition. Any disease or syndrome has its specific symptoms. The clinicians must carefully analyze all symptoms before making a diagnosis. As a major feature of the TCM palliative care, the clinicians must elucidate the mechanism, clinical features, and diagnostic method of a specific symptom (particularly, the major symptom) to differentiate diseases and syndromes and treat them accordingly. Ten common symptoms of cancer have been proposed (3): pain, nausea/vomiting, loss of appetite, constipation, fever, diarrhea, bloating, pressure ulcers, depression/anxiety, and sleep disorders. Alternatively, 36 common symptoms of cancer have been categorized: infection, difficulty swallowing, nausea/vomiting, anorexia, dry mouth, constipation, diarrhea, intestinal obstruction, ascites, malnutrition, coughing, breathing difficulties, hiccough, flu-like syndrome, urinary tract infections, urinary incontinence, headache, anxiety, insomnia, delirium, convulsions, anxiety, depression, thrombosis, disseminated intravascular coagulation, anemia, edema, hypercalcemia, spasms, pimple rash, fatigue, muscle atrophy, thrush, massive bleeding, acute pain, and suffocation. Meanwhile, these common symptoms of cancer are classified into the following diseases according to TCM classifications: loss of consciousness, convulsions, blood syndromes, cough, asthma disease, pleural fluid retention, vomiting, hiccough, dysphagia-occlusion, constipation, diarrhea, mouth sores, strangury disease, urinary incontinence, palpitations, insomnia, coma, abdominal retension, headache, consumptive disease, edema, and fever due to internal injuries. The classifications slightly differed among different ancient Chinese physicians. For instance, Li Yan (4) divided the common symptoms into 41 types for pattern identification. His detailed descriptions for these symptoms were highly informative for clinical practices. Identification and treatment of the major symptoms is an essential component and also the basis of pattern identification.
TCM-based pattern identification has shown great advantages in controlling cancer symptoms. During the symptomatic treatment, it can manage both the systemic conditions and local symptoms. After treatment based on pattern identification, the cancer symptoms and quality of life were improved in about 70% of patients with advanced cancers (5). According to a data from Shanghai Medical University (6), the 1-3-month symptom response rate after TCM treatment among patients with advanced liver cancers were as follows: upper abdominal fullness, 82.4%; anorexia, 72.6%; weight loss, 70.6%; liver pain, 46.2%; and fatigue, 62.7%. The 1-year survival was 10.8% in the TCM group and only 0.8% in the control group (P<0.05). In some patients with isolated and small liver tumors, the survival could be as long as over ten years after the application of spleen-nourishing and qi-regulating therapies.
According to Yu Er-xin from Shanghai Medical University Cancer Hospital, three principles may be applied in controlling cancer symptoms: (I) To investigate the regular pattern of cancer symptoms. According to the TCM theory, the rhythmical symptoms are related with the 24-hour rhythm. The common cancerous fever and pain often shows such a rhythm; (II) To use drugs on time (rather than “when required”) according the regular pattern of cancer symptoms. The medication should be changed when the symptom rhythm changes. For example, if the cancerous fever occurs at 14 p.m., the medication may be scheduled at 12 or 13 p.m., so as to achieve a good symptom control; And, (III) the symptoms and their rhythms may be altered along with the treatment and with tumor progression. Once new rhythm is found, the medications should be adjusted accordingly. In summary, the TCM-based symptomatic treatment is proactive. A passive or perfunctory attitude towards symptomatic treatment should be avoided. The aim of symptomatic treatment is to alleviate the symptoms and help the patients rest and work as a normal person. In addition to surgery, radiotherapy, chemotherapy, and other modern therapies, the TCM-based treatment can dramatically alleviate the clinical symptoms and improve the quality of life.
TCM improves pain
According to World Health Organization (WHO), an estimated 10 million people were newly diagnosed with cancer across the world and about 6 million people die from cancer. Notably, about 50% of these patients had cancer-related pain symptoms, and up to 70% of patients with advanced cancers with pain as their major symptom. About 50-80% of patients with pain did not have their pain effectively controlled due to various reasons (7). Thus, cancer pain has seriously affected the quality of life in patients with advanced cancer. Cancer pain has become the most horrific clinical manifestation for the majority of patients with cancer, particularly among those with advanced diseases. The cancer pain causes or aggravates other symptoms including loss of appetite, insomnia, weakness, forced posture, and bedsores in these patients. Compared with other symptoms, pain is more likely to cause emotional disorders. Proper and timely treatment of pain is helpful to improve the behavioral status and provide the required conditions for the treatment of primary disease. The three-step “ladder” for cancer pain relief developed by WHO has been widely accepted. If the proper drugs are appropriately used in terms of types, dosage, interval, and route, about 90% of cancer pain can be satisfactorily controlled. Therefore, medical therapy has widely accepted as the key approach for resolving cancer pain. However, cancer pain has never been well controlled due to various reasons. Even in the developed countries, 50-80% of cancer pain was not alleviated. Furthermore, although the three-step “ladder” strategy has been proven to be effective, the adverse effects (e.g., addiction and tolerance) of narcotics limit their usage. In recent years, TCM-based treatment for cancer pain has witnessed great advancement in laboratory experiments and clinical practices.
From the perspective of TCM, the etiology and mechanism of cancer pain can be categorized as “stagnation” and “cachexia”, which are presented as two syndromes- “excess” and “deficiency”. Nevertheless, there is no absolute difference between them. The development of cancer pain, in nature, is resulted from the interaction of multiple factors. Also, the mechanism of disease differs in the different phases and stages of tumors, and the “excess” or “deficiency” may clinically manifested in a diverse or mixed manner. In general, the cancer pain is mainly “excess pain” in the early and middle stage of a tumor and “deficiency pain” or “mixed pain” in the advanced stages. The clinical treatment should be based on the mechanism of the cancer pain, rather than just for relieving pain. Also, the drugs or therapies should be applied in a flexible way. In short, the principles of TCM treatment for cancer pain fundamentally differ from those of western medicine. The TCM treatment, from the perspective of holism, trace the etiology by syndrome differentiation, treat based on syndrome differentiation and in accordance with three categories of etiologic factors, and thus realize the targets of “strengthening healthy qi to eliminate pathogens and treating both the symptoms and pathogens”. Since TCM treatment for cancer pain has mild side effects and will not result in addiction, and some traditional Chinese drugs can shrink tumor size, they have been warmly welcomed by cancer patients. For example, Liu (8) used topical Toad venom extract to treat 117 patients with cancer pain. The effectiveness rate reached 92.65%, and the pain-relieving effect typically seen within 15-30 min. Also, he used Xiaozhong Zhitong plaster (topical cream for alleviating swelling and pain) to treat 300 patients with cancer pain, and the effectiveness rate was 75.7% for severe pain, 90.7% for moder pain, and 96.7% for mild pain.
Wu (9) used traditional Chinese drugs together with the 3-step “ladder” approach to treat the advanced colorectal cancer in 178 cases. Step one: regulating qi to stop level I pain, using prescriptions including Chaihu Shugan powder, Tiantai Wuyao powder, Jinlingzi powder; step two: removing stasis to stop level II pain, using prescriptions including Taohong Siwu decoction; and step three: detoxing to stop level III pain, using prescriptions including Gexiazhuyu decoction and Xinfang Huoming decoction. The total response rate reached 86.1%. Wang (10) treated cancer pain using drugs including Rehmanniae 18 g, Scrophulariaceae 18 g, Radix Asparagi 18 g, honeysuckle 18 g, forsythia 18 g, Red peony 30 g, Cortex moutan 30 g, Radix isatidis 30 g, and gypsum 30 g, which were decocted and administered together with centipede (n=4, powdered) and buffalo horn powder 20 g. The prescription was taken one dose (twice) per day, which achieved highly effective (the patients did not experience obvious pain after the withdrawal of other analgesics) in 19 cases, effective in 36 cases, and ineffective in 13 cases, yielding a total response rate of 81.4%. The therpay typically became effective within 1-3 days. Table 1 lists the common prescriptions for treating cancer pain.
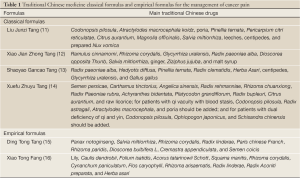
Full Table
Plaster therapy is another tropical therapy. Typically, traditional Chinese drugs with penetrating and strong odors are applied together with a medium (or added with transdermal agent). The medium can be water, vinegar, wine, bile, oil, honey, petrolatum, or glycerin. The transdermal agents include azone, which is most often used, propylene glycol, urea, and dimethyl sulfoxide. The common drugs included Radix aconiti, Radix aconiti kusnezoffii, Asarum, borneol, Angelica dahurica, Dragon’s Blood, mastic/myrrh, Rhizoma corydalis, Arisaema amurense maxim, peach kernel, safflower, ferula, Semen strychni, realgar, alum, indigo, musk, Venenum bufonis, pangolin, cantharides, and centipede. Plaster therapy has shown ideal effectiveness in treating cancer pain. For example, Han (17) used raw Capcjasmine 30 g, Radix aconiti 15 g, Faeces trogopterori 15 g, leech 15 g, eupolyphaga 15 g, gecko 15 g, Dioscorea bulbifera L 15 g, Semen strychni 15 g, centipede 8 g, camphor 8 g, and borneol 8 g for treating cancer pain. The drugs were powdered, mixed with vinegar, and then applied in the center of painful area, which was a bit larger than the pain area. The acupoints were selected according to the disease causes. Sustained, good analgesic effect was achieved, particularly for chest pain and rib pain. The total response rate was 81.8% (100% for mild pain, 81.8% for moderate pain, and 66% for severe pain). Clinical practices have demonstrated that TCM therapies can not only alleviate the cancer pain but also minimize the toxicity of anesthetic drugs by reducing or avoiding the use of these drugs.
In addition to traditional Chinese drugs, acupuncture also has a good effect on cancer pain. According to TCM theories, “unblocking the meridian/channel and regulating qi/blood” is the key to resolving pains including cancer pain. The acupoints should be carefully selected and coordinated according to the clinical symptoms/signs. Li (18) treated 113 patients with different types of cancer pain using acupuncture together with WHO 3-step “ladder” approach. Compared with the medication group (response rate: 50.00%), the acupuncture group has a significantly higher response rate (72.95%), yielding an overall response rate of 95.24%.
TCM improves nausea/vomiting
According to TCM, vomiting occurs when stomach loses its harmony and downbearing. The gastric disorders due to any reason can cause the stomach qi ascending counterflow, which is presented as vomiting (19). Vomiting can be the complications or associated symptoms of malignancies including gastrointestinal tumors and intracranial space-occupying masses. Cancer patients upon chemotherapy can also experience nausea or vomiting, which can result in or be accompanied with decreased appetite, malnutrition, low immunity, and increased cachexia. This condition can decrease the patients’ quality of life, shorten their survival, and even be fatal. TCM-based therapies can improve chemotherapy-associated nausea/vomiting by “strengthening vital qi and consolidating the constitution”, “fortifying the spleen and resolving dampness”, “regulating qi and resolving phlegm”, “warming stomach and relaxing the bowels”, and “regulating stomach and calming down the adverse-rising energy”.
Chemotherapy drugs can induce nausea and vomiting, which is mainly because these drugs can directly impair the spleen and stomach, and thus affect their transportation capabilities. The key mechanisms include damage to the spleen and stomach, exhausted healthy qi, abnormal transportation, and disordered gastric harmony and downbearing. Clinically the treatment principles include “fortifying the spleen and replenishing qi” and “harmonizing the stomach and downbearing counterflow”. Yang et al. (20) applied prescriptions targeting “fortifying spleen and resolving dampness” and “harmonizing stomach and stopping vomiting” for patients upon chemotherapy. These prescriptions successfully lowered the incidence of vomiting. Chen (21) used Xiaobanxia decoction that is able to fortify spleen, harmonize stomach, resolve dampness, and stop vomiting to treat symptoms related with disordered spleen and stomach such as vomiting, loss of appetite, and pale tongue, and the therapeutic effectiveness was satisfactory. Based on the principles of pattern identification, Dou et al. (22) divided the chemotherapy-related vomiting into several types: the type of “spleen-stomach vacuity weakness” was treated with Liujunzi decoction and other drugs; the type of “qi & yin dual vacuity” was treated with modified Radix Ophiopogon decoction and Orange peel-Caulis bambusae decoction; the type of “liver qi invading the distension stomach” was treated with modified Chaiping decoction; the type of “phlegm-dampness retention” was treated with modified Linggui-Zhugan-Xiaobanxia decoction; and the type of “ spleen-kidney yang deficiency” was treated with Guifu Li Zhong decoction. Qian (23) found that the modified Xuanfu Daizhe decoction combined with 5-HT3 receptor antagonist was superior to 5-HT3 receptor antagonist alone in treating chemotherapy-associated gastrointestinal reactions such as nausea and vomiting. The common orally administered TCM prescriptions are listed in Table 2.
The tropical application of traditional Chinese drugs is rapid, simple, and safe, and therefore has many advantages in preventing and alleviating chemotherapy-induced vomiting. Currently, the common tropical therapies for vomiting include acupuncture, acupoint injection, auricular acupressure, acupoint plaster therapy, and moxibustion. Meridians/collaterals/acupuncture points and acupuncture theories are the basis for the tropical TCM therapies. The tropical TCM therapies for chemotherapy-induced vomiting are usually applied in meridians, collaterals, acupoints including stomach meridian, spleen meridian, large intestine meridian, and conception vessel, with an attempt to mediate meridians and vessels, enhance the essential roles of meridians for “connecting organs and limbs”, and thus achieve the goal of “adjusting organs’ qi, harmonizing stomach, and downbearing counterflow” Peng et al. (38) observed 60 patients undergoing PE chemotherapy and found patients in the treatment group using conventional antiemetic method plus Zu Sanli acupoint block had remarkably milder gastrointestinal reactions than the conventional antiemetic group. Wu et al. (39) treated the chemotherapy-induced gastrointestinal adverse reactions by Zu Sanli and Shou Sanli acupoints injection with metoclopramide injection, vitamin B injection and vitamin D2 and calcium colloidal injection. Upon the dual stipulation of drugs and acupoint stimulation, the overall response rate reached 87.5%. As mentioned in The Songs of Four Major Acupoints, “the abdominal diseases are related with Zu Sanli”. Zu Sanli is the acupoint where the stomch meridian connects. With the capabilities of “invigorating the stomach and hamonizing the middle” and “treating counterflow and regulating qi”, it is a key acupoint for stopping vomiting. Fan (40) found that blocking the bilateral Neiguan with Vit B1 and vitamin B6 injections and acupuncture of Zhongwan, Jianli, bilateral Neiguan, and Shenmen could effectively treat chemotherapy-induced vomiting.
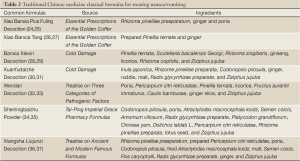
Full Table
TCM improves cancer-related fatigue
From the perspective of TCM, fatigue is a condition reflecting the Yin and yang imbalance due to the damaged physiological balance of “calm yin and sound yang” by a particular pathogen. It is often disease-related. Cancer-related fatigue is a subjective feeling of weakness and tiredness. The disease-related fatigue can be classified as “consumptive disease”. Consumptive disease is a general term for chronic deficiency diseases due to consumption of yin, yang, qi and blood. It is roughly equal to the chronic wasting diseases (e.g., advanced tumors) in modern medicine. However, there is no corresponding TCM term for cancer-related fatigue, which can be treated as a consumptive disease based on its clinical manifestations including weakness, tiredness, depression, lethargy, and gloominess. Clinically it can be divided into four types: syndrome of qi and blood deficiency, syndrome of weak spleen and stomach, syndrome of liver and stomach disharmony, and syndrome of Qi and blood stagnation (Table 3). Based on the principles of “pattern identification” and “treating different disease with the same therapy”, the TCM therapies apply the combined approaches including “tonifying qi and activating blood”, “strengthening spleen and harmonizing stomach”, “soothing the liver and regulating qi”, “directing qi downward to stop vomiting”, “activating blood and resolving stasis”, and “removing toxin and fighting against cancer” to alleviate symptoms and improve the patients’ quality of life. Meanwhile, fatigue is not only a physical problem; rather, it is involved with obvious emotional, psychological and social consequences. Furthermore, the mental and emotional depression is often more common than the physical presentation. Therefore, psychotherapy is particularly important for the patients and even their care providers.
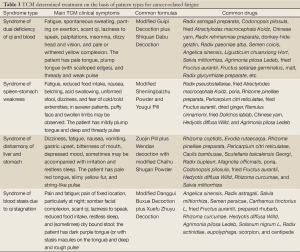
Full Table
Many cancer patients experience fatigue due to senility, mental disorders, qi/blood stagnation, and spleen/stomach weakness (41), whereas repeated surgery, chemotherapy, and multiple chemotherapy cycles may make the patients become qi/blood deficiency and thus suffer from increased fatigue. Qi et al. (42) found that TCM-based adjuvant therapy can not only delay tumor progression and enhance immune function but also enhance the sensitivity to chemotherapy, reduce the chemotherapy-induced side effects (e.g., gastrointestinal symptoms such as diarrhea, nausea, and vomiting and respiratory infections), and protect liver function, so as to alleviate radiotherapy or chemotherapy-induced fatigue. Chen (43) divided 60 breast cancer patients into intervention group and control group. The intervention group received Buzhong Yiqi decoction as adjuvant therapy, which showed remarkably better effectiveness than the control group in alleviating cancer-related fatigue, which may be explained by the fact the TCM diet can not only meet the nutritional requirements but also alleviate cancer-related symptoms and treat-induced adverse reactions. Xu et al. (44) integrated the TCM and western medicine including self-acupressure and abdominal breathing training for the management of 80 patients who had undergone modified radical mastectomy, and the results showed that the integrated management could effectively alleviate cancer-related fatigue.
In recent years, some active extracts of traditional Chinese drugs have been applied in the clinical management of cancer-related fatigue: (I) Ginseng: a Mayo Clinic research group reported in the ASCO annual meeting that ginseng contains saponins, the steroid-like compounds, which are helpful to ease the sense of fatigue; (II) Acanthopanax: Guan et al. (45) confirmed that the eleutherosides and other extracts of acanthopanax showed exciting effect in the mouse rope-climbing test, with the exciting unit ranging from 2,000 to 8,000. Acanthopanax can promote the biosynthesis of protein and DNA-RNA and prevent the decrease of protein and nucleic acid synthesis; (III) Shengmai and Shenqi injections: Gu et al. (46) used Shengmai and Shenqi injections to treat cancer-related fatigue. Shenqi Fuzheng injection, with Codonopsis pilosula and Radix astragali as the main raw material, can tonify qi, restore deficiency, and enhance immunity. The Shengmai Injection contains Codonopsis pilosula, Schisandra chinensis, and Ophiopogon japonicus. It can nourish yin and restore pulse. Codonopsis pilosula can tonify and replenish the middle qi and regulate the spleen and stomach. Modern pharmacological experiments have proved that the polysaccharides from Radix codonopsis can promote the formation of thymic T lymphocytes. Schisandra chinensis can excite the nerve center, make the tired brain waves return normal, improve the intellectual activity and endurance, and enhance the human body’s defense against the non-specific stimuli; (IV) Tanshinone: Ge et al. (47) found that the tanshinone injection had good effectiveness in treating cancer-related fatigue. Tanshinone can promote the rapid oxidation of nicotinamide adenine dinucleotide (NADH) in mitochondria and thus alleviate the accumulation of injury factors (e.g., the inhibition of glycolysis, suppression of citric acid cycle, excessive production of oxygen free radicals, and sodium lactate accumulation) due to the deposition of NADH.
TCM improves the general conditions
For advanced cancer patients who are not eligible for surgery, radiotherapy, or chemotherapy and those were are only eligible for symptomatic palliative radio-chemotherapy, TCM-based pattern identification and anti-tumor treatment must be carefully scheduled to improve the general symptoms/signs, enhance the immunity, and maintain the tumor in a stable status. For example, the spleen-fortifying and qi-regulating prescriptions can relieve abdominal pain; yin-fortifying and qi-replenishing medicinals can enhance the immunity; heart-nourishing, tranquilizing, liver-soothing, and qi-regulating medicinals can adjust the mental status, improve sleep, and reduce the occurrence of depression; Brucea javanica cream can treat brain metastases; Fuzheng Yangyin decoction (Radix rehmanniae, Radix rehmanniae preparata, Ophiopogon japonicus, Scrophularia ningpoensis, raw Radix astragali, Rhaponticum uniforum, Houttuynia cordata thunb, and Cimicifuga foetida) has shown certain efficacy in regulating spleen and stomach in patients with non-small cell carcinoma or advanced liver cancer. It can alleviate the symptoms to varying degrees in a significant proportion of patients, prolong survivals in some patients, and even achieve long-term survival in a few patients. In a prospective study, Liu et al. (48) used yin-nourishing, fluid-nourishing, qi-tonifying, and yang warming medicinals to treat 304 patients with advanced primary cancers. Compared with the chemotherapy group, the TCM group significantly prolonged the survival, resolved or stabilized tumors, improved quality of life, and adjusted the immune functions. Zhou et al. (49), based on the features of lung cancer including phlegm, stasis, deficiency, and toxin, developed two prescriptions—Yachan tablets and Gujin Mojin tablets. After medication, symptom improvements were observed in 61.7-68.8% of patients; although the tumor inhibition rate was only 6-10%, the survival reached 8 months and 10 months, respectively, which was significantly superior to the chemotherapy group, realizing the targets of “alive with tumor” and “improved quality of life” for patients with advanced tumors. Chen et al. (50) investigated the effectiveness of TCM in treating primary non-small cell lung cancer in a meta-analysis of 7 trials, which showed that the median survival was 335.4 days in the TCM group and 231.8 days in the chemotherapy group, indicating that although the TCM is superior to chemotherapy in terms of long-term survival, although with low effectiveness. It was found that the symptomatic TCM treatment could remarkably improve the quality of life in frail patients with advanced cancers. According to Yin (51), TCM therapies can adjust qi by adjusting liver, fortifying spleen, and tonifying kidney; thus, they can improve the accompanied symptoms of malignancies, improve the quality of life, and meanwhile reflect the concepts of humane care.
Emotional care in TCM
Concept of “Seven emotions” in TCM
According to TCM, the seven emotions refer to seven emotional activities including joy, anger, worry, anxiety, sadness, fear and fright. The seven emotions are believed to be the normal mental status of human beings. Normally, the seven emotions don’t cause diseases and only when the emotional stimulations are too abrupt, violent, and prolonged and beyond one’s adaptability or when there is diminished adaptability due to imbalanced yin-yang, qi and blood of viscera, can they turn into pathogenic factors, thus causing or aggravating diseases. Since the seven emotions can hurt viscera and cause the disorders of visceral functions, they are considered to be one of the main pathogenic factors from the perspective of TCM, which is known as “internal injury due to seven emotions”. As noted in Inner Canon of Huangdi, “excessive anger impairs the liver, excessive joy impairs the heart, excessive contemplation impairs the spleen, excessive grief impairs the lung, and excessive fear impairs the kidney; also, rage leading to qi ascending, excessive joy leading to qi loose, excessive sorrow leading to qi consumption, fear leading to qi sinking, fright leading to qi turbulence, pensiveness leading to qi knotting, and worry leading to qi accumulation”. Therefore, emotions can cause diseases by directly affecting the related organs or by indirectly causing disordered qi and making the organs can’t exert their normal physiological functions. According to the Orthodox Medical Records, “the seven emotions are matched with the five viscera. Excessive emotions hurt the five viscera. The internal injuries due to the seven emotions are difficult to treat. Therefore, it is important to identify the damaged viscera by observing its color, checking its pulse, observing its morphology, and determining its excess or deficiency. Then a proper treatment can be applied”. The emotional care is roughly equal to the psychological care in modern medicine. The purpose of emotional care is to provide various care to eliminate the poor mental status of the patients, making the mental factors become positive factors that may help to resolve the disease. Emotional care has a long history in China. The Inner Canon of Huangdi, which was compiled in Spring and Autumn/Warring States Period, noted that “Keep the mind free from avarice. In this way the Genuine-Qi in the body will be in harmony, the essence and spirit will remain inside, and diseases will have no way to occur” (52); and, “loss of spirit and willingness results in the poor prognosis of a disease” (53). These statements fully elaborate the importance of spirit and emotions in disease prevention and treatment as well as health care, which lays a foundation for the TCM-based emotional care. In the coming centuries, doctors further elucidated this concept and developed unique emotional care approaches.
Emotional care for patients with advanced cancers
With physical symptoms such as pain, most patients with advanced cancers will be depressed and are often fearful of death. Therefore, the medical staff must have good virtues, know the concept of “Seven Emotions”, and grasp the basic principles of “emotion-related diseases”. Also, the medical staff must be noble, nice, reliable, friendly, and skillful, so as to encourage the patients to be optimistic and mobilize their cortex and viscera to actively adjust body functions and thus improve the therapeutic effectiveness. Dr. Sun Simiao [581-682] of the Tang Dynasty is one of the founders of psychotherapy in China. Throughout his life, he paid great attention to the moral cultivation of medical practitioners. He believed that the good psychological communication could enhance the patients’ response to treatment. In his book Da Yi Jing Cheng (also named Mastership Lies in Excellence and Honesty), he writes (52), “When treating a patient, a great doctor must calm himself down and be free of desire or requirement; he must be with mercy and swear to save those who are suffered. If a patient come to ask for help, the doctor should treat him/her equally as his own family members, no matter the patient is poor or rich, young or old, friend or foe, Chinese or foreigners, wise or foolish.. The patient’s pain is just as the doctor’s. With deep mercy, the doctor must visit the patient’s house to rescue the patient wherever the condition is dangerous, dark, cold or whenever the doctor himself is hungry, thirsty, or tired. Never just try to show off himself.” This is exactly the same as the modern theory that good doctor-patient relationship and good virtues of medical staff can help the patients to maintain a good stress status to receive the treatment, so as to achieve the optimal treatment and nursing effectiveness.
Counseling
Counseling is a basic treatment method by patiently explaining the conditions to the patients. According to Ling Shu Jing - Shi Zhuan, “Normally, people hate death and are willing to survive, telling the patients the severity of disease, explaining the good outcomes of the disease, introducing the effective treatment, and conciliating their pain. Even the most unreasonable person will listen to the doctor”. Person’s character is varied. For brash patients, the medical staff should patiently tell them that “eager produces anger, and anger impairs the liver”, making the disease more severe. The patient should be advised to control his/her temper to nourish the liver; when the liver qi becomes smooth, the disease will be cured. For depressed patients, they should be repeated comforted; meanwhile, they should be explained that pensiveness leading to qi knotting, and worry hurts lung. The patient should be relaxed to nourish the lung. “Lung dominates the qi throughout the body and regulates the water”. The harmonized qi and good qi/blood circulation help the patient recover from the disease. In addition, the disease severity also varies among patients. For example, some patients have life-threatening diseases, which may make the patients become despaired. Then, it is important to provide counseling to the patients to explain the disease conditions and the importance of maintaining a cheerful, optimistic, and open-minded mood. For the critically ill patients, the medical staff should keep calm and avoid using irritating language, encouraging the patients to establish the confidence to overcome the disease.
Transference of attention
Transference of attention is applied to help the patients to pay less attention on their diseases and achieve better mental status, so as to promote their recovery from disease. As mentioned by Medical Records for Clinical Guidance, “A depressed emotion is caused by the unresolved, twisted feelings, and the cure of disease should be based on the transference of attention”. Therefore, the emotion-related diseases can be treated by the transference of attention. Also, the Li Yu Pian Wen (the Corpus Text of Disease Management) noted, “Diseases related with the seven emotions can be cured by reading books or watching an opera, which may be better than medications”. Playing chess, playing musical instrument, reading book, painting, fishing, and tourism can achieve the transference of attention, change the patients’ psychopathological status, and thus achieve good therapeutic effectiveness. In fact, transference of attention is designed to utilize the good external environment to change the patients’ attention on disease, so as to minimize the bad stimulation of poor emotions.
The emotional care in TCM is an integration of science and art. By observing and analyzing the patients’ psychological activities, it provides flexible and feasible care for the patients, so as to restore the imbalanced psychological and physiological functions and promote the cure of diseases. It reflects a dynamic holistic view of health and is also a key component of TCM (54).
Conclusions
Based on the principles of holism and pattern identification, TCM is a key component of the multidisciplinary treatment for advanced tumors. As shown in a large number of studies, the proper use of TCM-based therapies can enhance immune function, speed up recovery, alleviate radiochemotherapy-related toxicities, relieve pain, improve quality of life, and extend survival. TCM has shown unique advantages in treating malignancies when compared with modern medicine. However, as shown in many clinical reports, TCM-based treatment is targeted at improving symptoms, improving quality of life, and extending the survival. Therefore, it can be categorized as palliative therapy. From the perspective of modern medicine, palliative therapy is mainly targeted at cancer cells and a few life-threatening symptoms. Few palliative therapies are specially designed for the common discomforts/symptoms related with malignancies, although the symptomatic management is also very common. Although TCM has not made breakthrough in the radical treatment of malignancies, the “pattern identification” and other principles of TCM have shown many advantages in improving cancer-related symptoms. Nevertheless, the role of TCM in treating malignancies remains controversial. The rules of pattern identification for malignancies, the summarization of relevant experiences, and the interpretation of its clinical effectiveness warrant further exploration.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Zhang J. Clinical values of Traditional Chinese medicine in improving the quality of life of cancer patients. Zhong Hua Yi Xue Xie Zuo Za Zhi 2000;7:735.
- Liu JX. The role of Traditional Chinese medicine in maintaining QOL of cancer patients. Zhong Hua Zhong Liu Za Zhi 2002;24:309-10.
- Zhang BC. Treatment of symptoms and root causes of disease-management of the top ten symptoms in cancer patients. Fang Ai Tian Di 2007;20:17-8.
- Li Y. eds. Clinical experience on treatment of tumors. Beijing: People’s Medical Publishing House, 1996.
- Xu L, Chen XY. The application and status of Traditional Chinese Medicine in palliative care in cancer. Nan Jin Zhong Yi Yao Da Xue Xue Bao 2004;20:88-90.
- Liu LM. Chinese Traditional medicine treatment for advanced cancer. Shi Yong Zhong Liu Za Zhi 1997;12:152.
- Li SR, Tian J. The current research status of cancer pain. He Bei Yi Yao 2011;33:437-8.
- Luo XQ. The current research status of Traditional Chinese medicine treatment for cancer pain. Jiang Xi Zhong Yi Yao 2002;33:47.
- Wu LC, Lin SY. The three-step “ladder” of Traditional Chinese medicine treatment for colorectal cancer. Zhe Jiang Zhong Xi Yi Jie He Za Zhi 1994;4:5.
- Wang GP, Wang HW. Recent developments of Traditional Chinese medicine for cancer pain relieving. Shang Dong Zhong Yi Za Zhi 2003;22:188.
- Du YG. Modified Liujunzi decoction for liver cancer pain in 65 cases. Jiang Su Zhong Yi 1997;18:23.
- Liu CF. Xiaojianzhong decoction for abdominal cancer pain of deficiency cold type in 38 cases. Shi Yong Zhong Yi Yao Za Zhi 2000;16:17.
- Liu MX. 42 cases of advanced cancer patients with pain treated by peony and licorice decoction. Guo Yi Lun Tan 2005;20:5-6.
- Ren HP. 38 cases of advanced cancer patients with pain treated by xuefuzhuyu decoction. Zhong Yi Yan Jiu 2002;15:40.
- Chen DH. 45 cases of cancer pain treated by Dingtong decoction. Hu Bei Zhong Yi Za Zhi 2002;24:33.
- Peng HY, Zhang YH, Wang RP, et al. Clinical observation on the treatment of Dingtong decoction for cancer pain. Si Chuan Zhong Yi 2003;21:46.
- Han ZM. 44 cases of cancer pain by acupoint plaster therapy. Zhong Ri You Hao Yi Yuan Xue Bao 1998;12:310.
- Li PW. eds. Postoperative treatment of malignant tumor. Beijing: People’s Medical Publishing House, 2001.
- Ling Y, Yang D, Shao W. Understanding vomiting from the perspective of traditional Chinese medicine. Ann Palliat Med 2012;1:143-60.
- Yang P, Wang DJ, Qi JK. Clinical effect of integrative medicine therapy on gastroenteric reaction induced by chemotherapy prevention and treatment. Xi Bu Yi Xue 2009;21:237-8.
- Chen SK. Treatment experience of minor pinellia decoction for vomiting induced by chemotherapy. Zhong Yi Za Zhi 1994;12:18.
- Dou YQ, Feng Y, Gao LP. Traditional Chinese medicine treatment for gastrointestinal reaction induced by chemotherapy. Zhong Hua Lin Chuan Yi Xue Za Zhi 2005;6:11.
- Qian XX. Decoction of Xuanfu-Daizhe for the treatment of digestive symptoms during tumor chemotherapy in 63 cases. Zhong Guo Zhong Yi Yao Xian Dai Yuan Chen Jiao Yu 2011;9:96.
- Liu X, Wang JH. Clinical effect of Minor Pinellia Decoction Plus Poria in prevention of chemotherapy-induced nausea and vomitus. Zun Yi Yi Xue Yuan Xue Bao 2008;31:607-9.
- Guo TL. Clinical observation on Minor Pinellia Decoction Plus Poria in treating delayed nausea and vomit caused by cisplatin-based chemotherapy. Zhong Guo Wu Zhen Xue Za Zhi 2008;8:4841-2.
- Liu BY. Clinical observation on Minor Pinellia Decoction in treating vomit in 38 cases. Shan Xi Zhong Yi Xue Yuan Xue Bao 2007;8:40.
- Li XL, Huang JL, Hu X. Clinical observation of minor pinellia decoction in the treatment of 121 cases of vomiting induced by chemotherapy. Chuan Bei Yi Xue Yuan Xue Bao 1999;14:59-60.
- Liu Y, Zhang SF. Banxiaxiexin decoction for the treatment of gastrointestinal reaction induced by chemotherapy. He Nan Zhong Yi 2004;24:12.
- Zhang XL, Wang GF. Banxiaxiexin decoction for the prevention of nausea/vomiting induced by Cisplatin plus chemotherapy in 90 cases. Jiang Xi Zhong Yi Yao 2007;38:28.
- Jia RM, Song JS. Randomized, controlled trials of decoction of Xuanfu-Daizhe in the prevention of vomiting caused by chemotherapy: a meta-analysis. Ji Lin Zhong Yi Yao 2010;30:218-9.
- Zhou YQ, Han ZY. Clinical observation of decoction of Xuanfu-Daizhe in the prevention of vomiting caused by chemotherapy. Shang Hai Zhong Yi Yao Da Xue Xue Bao 2005;19:27-8.
- Xu YF. Prevention and treatment of nausea and vomiting after chemotherapy by wendan decoction. Zhe Jiang Zhong Yi Yao Da Xue Xue Bao 2009;33:349-50.
- Sun BQ, Wei ZM. A crossover and comparative study on traditional Chinese medicine and granisetron in the treatment of vomiting caused by cisplatin-based chemotherapy. Zhong Guo Shi Yan Fang Ji Xue Za Zhi 2007;13:70-1.
- Chen W, Wan YJ, Liang YH, et al. Clinical observation on shenlingbaizhu powder and metoclopramide in treating 49 cases of nausea and vomiting after chemotherapy. Shi Zhen Guo Yi Guo Yao 2007;18:1992.
- Rong SF, Xu ZG. Observation on curative effect of shenlingbaizhu powder to treat 49 patients with nausea and vomiting after chemotherapy. Zhong Guo Xian Dai Yi Sheng 2009;47:61-103.
- Huang ZR. Clinical observation on xiangshaliujunzi decoction for nausea and vomiting caused by cisplatin. Fu Jian Zhong Yi Yao 2008;39:8-9.
- Zhang KM. Prevention of vomiting after chemotherapy by xiangshaliujunzi decoction and metoclopramide. Xian Dai Zhong Liu Yi Xue 2009;17:1989.
- Peng YT, Zhang YM, Pan GY. Prevention and treatment of gastrointestinal reactions after chemotherapy by injecting in Zusanli point in 30 cases. Shan Xi Zhong Yi Xue Yuan Xue Bao 2009;32:33-34.
- Wu GW, Yang XY. Clinical observation of acupoint injection in improving gastrointestinal reactions after chemotherapy in tuberculosis patients. Guo Ji Yi Yao Wei Sheng Dao Bao 2007;13:58-60.
- Fan YS. Acupuncture and acupoint injection treatment for vomiting induced by chemotherapy. Zhong Guo She Qu Yi Shi 2005;7:58-9.
- Lu W. Traditional Chinese medical treatment by differentiating syndromes for cancer-related fatigue during chemotherapy. Ji Lin Zhong Yi Yao 2010;30:1054-5.
- Qi F, Li A, Inagaki Y, et al. Chinese herbal medicines as adjuvant treatment during chemo- or radio-therapy for cancer. Biosci Trends 2010;4:297-307. [PubMed]
- Chen LC. Clinical observation of 30 cases of postoperative Cancer-Related Fatigue of breast cancer by nursing intervention and Traditional Chinese Medicine. Zhong Yi Yao Dao Bao 2011;17:89-90.
- Xu JJ, Gu LX, Qiao H. Effect of Traditional Chinese and Western Medicine Joint Exercise Therapy on Cancer-Related Fatigue after Operation of Mammary Cancer. Zhong Guo Quan Ke Yi Xue 2010;13:3225-6.
- Guan FS, Li ZX, Liao YM. Clinical investigation of acanthopanax root injection for improving the postoperative fatigue syndrome of the patients with gastrointestinal tumors. Guo Ji Yi Yao Wei Sheng Dao Bao 2008;14:78-81.
- Gu YQ, Xu HB, Jiang YG, et al. Clinical effect of Shenqi Fuzheng Injection (SQFZI) on cancer-related fatigue. Zhong Guo Zhong Xi Yi Jie He Za Zhi 2009;29:363-4.
- Ge JH, Zhang YL, He HX. Clinical observation on TanshinoneIIA Sulfonic Sodium injection combined with thymosin in the treatment of cancer-related fatigue. Lin Chuan Yi Yao 2009;18:56.
- Liu JX, Shi MZ, Sun ZH. Clinical research of primary lung adenocarcinomas by nourishing Yin, tonifying Qi and warming Yang. Zhong Yi Za Zhi 1995;36:55.
- Zhou DH. eds. Case collection of cancer treatment. Guangzhou: Guangdong Higher Education Press, 1997.
- Chen ZF, Wu WJ. A meta-analysis of traditional Chinese medicine treatment on non-samll cell lung cancer. Zhong Yi Za Zhi 1999;40:287.
- Yin DF. eds. Clinical research on the improvement of survival quality of patients with malignant tumors by adjusting the Qi movement. Beijing: Beijing Union Medical University Press, 2007.
- Chen SD. eds. Hand out of Nei Jing. Shanghai: Shanghai Scientific and Technical Publishers, 1984.
- Wang YK. eds. Promotion guidance for doctor of Traditional Chinese medicine (Canon parts). Hebei: Hebei science and technology publishing house, 1985.
- Chen WS, Chen WQ. History and application of traditional Chinese medicine nursing. Liao Ning Zhong Yi Yao Da Xue Xue Bao 2007;9:172-3.


