Effects of relaxing therapies on patient’s pain during percutaneous interventional radiology procedures
Introduction
“Sophrology” is the study of human consciousness and the existential values of being.
The term was created by Professor Alfonso Caycedo, a neuropsychiatrist supervised by the School of Phenomenological and Existential Psychiatry, to designate a scientific method that he has devised for the study of consciousness and to control the body balance—spirit (1,2).
This method is sometimes compared to hypnosis, sometimes called psychotherapy, relaxation method or even alternative medicine.
These alternative medicines have become a valuable aid in recent years in the management of patients in oncology, indeed these soft and non-invasive techniques allow patients to better support interventional radiology procedures related to their cancer treatment by reducing anxiety and pain (3).
The objective of our study was to relate our experience in the use of sophrology techniques during interventional radiology procedures and evaluate the effects on patient’s pain.
Methods
Patient population
We present a prospective observational study on 60 consecutive patients (30 men, 30 women, mean age of 62.5 years) who underwent interventional radiology procedures in a context of cancerological management. From September 2017 to March 2018, 42 patients were enrolled and were asked if they wished to benefit from sophrology and hypnosis while their programmed interventional radiology procedure. The procedures consisted of biopsies performed under CT or ultrasound, as well as central venous catheterization under fluoroscopy. The sites to be biopsied were at the bone, pulmonary, hepatic, thyroid and lymph nodes sites. Oral information was given to the patients and written informed consent for the treatment and the use of their anonymized data for this study was obtained for each patient. A control group, including 18 patients, was also established to compare the results obtained with versus without the use of relaxation techniques during interventional procedures.
Sophrology technique and response assessment
The sophrology technique consisted in reassuring the patient before the intervention, by speaking to him gently and positively, by making him concentrate on his breathing and on positive memories. The technician then placed himself at the patient’s head during the gesture and continued to reassure him and try to put him in a state of hypnosis: a temporary state of modified attention whose characteristic is an increased suggestibility. The goal was to arrive at a mental relaxation, to make the gesture in better conditions for the patient and the doctor.
The sophrology time in minutes was evaluated before and during each procedure for all patients by the technician who practiced sophrology. Anxiety before and during the gesture was evaluated by asking each patient to assess their anxiety using the visual analog scale (VAS) with values from 0 to 10 (10 indicates the strongest anxiety ever experienced and 0 indicates absence of anxiety) by an independent evaluator. A difference in VAS >2 points was considered a clinically significant result. The pain experienced by the patients during the procedure was also evaluated after the procedure had been performed by asking the patients to quantify their perceived pain with the help of VAS. A difference in VAS >2 points was also considered a clinically significant result for pain.
The relaxing therapies were all performed by two technicians, the interventional radiology procedures were all performed by two interventional radiologists (with 7 and 3 years of experience). The benefit of the relaxing therapy procedure on the gesture was evaluated by the interventional radiologist at the end of each procedure, as low, medium or high.
Statistical analysis
The VAS score was measured before and after each procedure for anxiety evaluation, and after each procedure for pain evaluation. Pre- and post-operative scores were compared using the non-parametric Wilcoxon signed-rank test for paired data. P<0.05 was considered statistically significant. Comparisons between the two procedures in terms of anxiety or pain as carried out in using Wilcoxon rank test for unpaired data. Confidence interval were computed in bootstrapping data. Statistical analyses were performed by using R CRAN Software (version 3.1.1).
Results
Data are summarized in Tables 1 and 2.
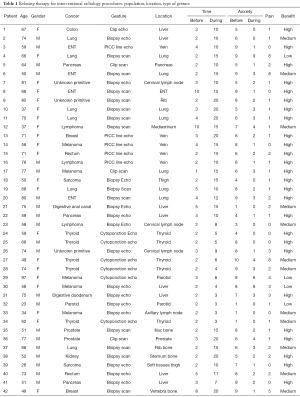
Full table
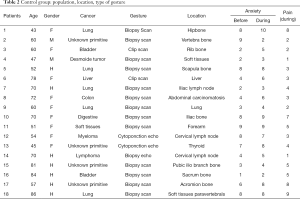
Full table
Anxiety and patient’s pain
The average evaluation of anxiety was 6.35 (95% CI, 5.84–6.81) before procedures and 2.07 (95% CI, 1.48–2.82) during procedures performed with sophrology techniques, and was 5.34 (95% CI, 4.04–6.67) before procedures and 5.94 (95% CI, 4.62–7.22) during procedures performed without relaxing therapies.
The average evaluation of pain felt during procedures was 1.83 (95% CI, 1.23–2.78) for procedures performed with sophrology techniques and was 4.16 (95% CI, 2.53–6.04) for procedures performed without relaxing therapies.
Our results show:
- In the sophrology group: a significant decrease in anxiety experienced by patients during interventional radiology procedures (P=3.318E−08) compared to before procedures (Figure 1). Ninety-five percent of patients are less anxious during intervention whereas 5% remain equally anxious. The mean difference level of anxiety was 4.31 (95% CI, 3.592–5.026).
- In the control group: a significant increase in anxiety experienced by patients during interventional radiology procedures (P=0.02) compared to before procedures. Twelve percent of patient are less anxious during intervention whereas 17% remain equally anxious and 71% are more anxious. The mean difference level of anxiety was −0.6 (95% CI, −1.66 to 0.44).
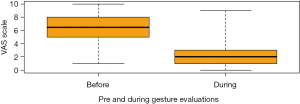
The level of anxiety during gestures in sophrology group was inferior to that of the control group (P=2.035E−06).
In average the level of anxiety was 2.07 (1.54–2.84) in the sophrology group, whereas 5.94 (4.73–7.12) in the control group.
The level of pain felt during gestures in the sophrology group was inferior to that of the control group (P=7.03E−05).
Average level of pain was 1.83 (1.23–2.78) in the sophrology group while 4.16 (2.53–6.04) in control group.
We observed no significant difference before the gesture between the 2 groups concerning the level of anxiety (P=0.197).
Benefit for patient and doctor
We reported a significant benefit felt by the doctor-operator for the optimal realization of the gesture (P<0.05) as for 26/42 of gestures, doctor-operator found sophrology highly beneficial, 12/42 found fairly beneficial and in four cases, sophrology was found poorly beneficial.
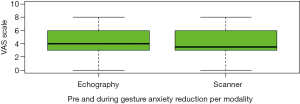
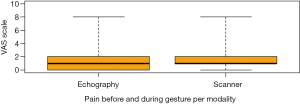
We found no significant difference in anxiety reduction depending on the embodiment of the gesture, whether using scanner or echography (P=0.906) in the sophrology group (Figure 2), also no difference in reported pain in using scanner or echography (P=0.199) for the interventional procedures (Figure 3).
The average time for sophrology before gesture was 3’8” (2’24”–4’24”) and during gesture was 11’32” (10’4”–13’1”).
In the sophrology and control group, patients were 50% male, 50% females, 62.3 and 63.4 years old in average. Age was not different in each group (P=0.95).
In the group experiencing sophrology, gender was not a factor for different anxiety before the gesture (P=0.75) or during (P=0.35) the gesture. No significant difference was found regarding the reported level of pain (P=0.92) depending on the gender.
Discussion
At our knowledge, there are only few articles in the literature demonstrating the benefit of relaxing therapies (sophrology and hypnosis) for the management of patients in oncology, our article is the first to show the benefits for patients in percutaneous interventional radiology (4,5).
Our study shows a significant decrease of patient’s anxiety during procedures performed with relaxing therapy, and a lower pain felt by patients during the procedures.
Our results match those of the literature, confirming better overall management of the pain and stress of patients in oncology, a procedure facilitated by better conditions, a better experience of the gesture by patients, allowing decrease of drug use and improving procedural safety (6-8).
These gentle noninvasive approaches revolutionize the management of patients for biopsy procedures, allowing for a reduction in patient stress and therefore less sudden movements, a calmer breathing and better access to certain difficult deep lesions for the interventional radiologist. We observed less complication during our procedures, especially less pneumothorax during lung biopsy.
Sophrology comes from three Greek words: “SOS” meaning free of diseases, balance, harmony; “PHREN” meaning diaphragm, affective soul and by extension, mind, conscience and “LOGOS” meaning science, study, speech (9).
It is based on several principles: the principle of objective reality: this way of thinking seeks to develop the adaptability of the person to the different situations of life, it is to objectively see the situation as it really is without transforming it; the principle of integration of the body diagram as a lived reality: it is simply a question of multiplying the body sensations thanks to the training in order to be in harmony with his body; the principle of positive action: it reinforces positive thinking in the body and mind, so that we can realize ourselves, be who we are (10).
The sophronic alliance is the relationship of trust established between the sophrologist and the accompanied person. It remains active and master of the success of this support (11).
It is necessary to train the technicians, nurses in these techniques for optimal efficiency. The technicians who practiced the relaxing therapy in our study had been trained for 2 years in sophrology, although shorter training times are also possible.
This technique has many applications in medicine and appears particularly effective in percutaneous oncological interventional radiology (12). Empathic attention associated with hypnosis seems to bring better results than empathic attention alone, some authors have demonstrated that it reduces pain, anxiety and medical use whereas empathic approaches without hypnosis that provide an external focus of attention and do not enhance patients’ self-coping can result in more adverse events (13).
Before an intervention, patient anxiety may be difficult to assess. It is indeed composed of “state anxiety” (emotional reaction at a given moment, tension, apprehension, nervousness) and “trait anxiety” (anxiety felt daily). The “state trait anxiety inventory” (STAI) is a test composed of 20 propositions to know what the subject feels on the moment and generally (14). We did not use it in our study because it was too long and complicated for oncology patients, as well as the Hamilton anxiety rating scale (HAM-A) consisting of 14 items, each defined by a series of symptoms, and measuring both psychic and somatic anxiety (15). We preferred a simpler quantification using a score ranging from 0 to 10, faster and more reliable in our case. Discuss with the patient before the procedure allows to estimate his receptivity to the technique, and the possible causes of failure of the technique.
The use of these relaxation techniques is varied in the medical field, they are also used in interventional senology where they have demonstrated their effectiveness (16,17). These techniques are associated with superficial and deep local anesthesia during biopsy procedures, which can be alleviated based on pain experienced by patients, some authors have experienced less use of analgesics during interventions and therefore reduced cost during interventional radiologic procedures (18).
The causes of technical failures observed were related to the misunderstanding of the patients (presence of brain metastases preventing normal communication between the technician and the patient in one case), this could also be observed in case of hearing problems of the patients (one case), finally in rare cases some patients are refractory and prefer to manage their stress alone without external help, these patients are most often easy to identify during the dialogue established before the gesture.
Our study has some limitations, first our sample remains small. Secondly, the study is not randomized because we preferred to leave the choice to the patients who suffered from heavy chronic pathologies to be able to benefit from the techniques of relaxations during their interventions, it is also for this reason that the control group is of smaller size than the group treated with sophrology. The goal being to be the least disturbing possible in the care of patients and their wishes.
The relaxing therapies can be time-consuming for some patients, nevertheless these techniques seem to bring a lot to both patients and physicians during interventional radiological procedures in cancerology.
Conclusions
Relaxing therapies, such as sophrology and hypnosis, seems to be an interesting additional tool for the management of patients in interventional oncology, inducing a decrease of stress, pain, and anxiety in patients. This allows a treatment in better conditions, both for the patients who live better the gesture and for the interventional radiologist for the technical realization of the procedure allowing a better lesion accessibility. These non-invasive techniques should be systematically proposed to all cancer patients who should benefit from a biopsy in their care. All medical and paramedical health care providers should be trained in these practices.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study has been approved by our institutional review board at center Antoine Lacassagne (No. 2018/29). Written informed consent for the treatment in this study was obtained for each patient.
References
- Caycedo A. Sophrology and psychosomatic medicine. Am J Clin Hypn 1964;7:103-6. [Crossref] [PubMed]
- Fiorletta P. Les « techniques-clés » de la Sophrologie Caycédienne®: The key techniques of sophrology. Kinésithérapie, la Revue 2010;10:31-6.
- Sicard S. Cancer et sophrologie. Psycho-Oncologie 2009;3:184-7. [Crossref]
- Barré C, Falcou MC, Mosseri V, et al. Sophrology for patients in oncology. Soins 2015.17-20. [PubMed]
- Gaide M, Surdej F, Daoud-Carrera C, et al. Sophrology for developing strategies to help patients adapt to cancer treatments. Rev Infirm 2017;66:37-9. [Crossref] [PubMed]
- Lang EV, Joyce JS, Spiegel D, et al. Self-hypnotic relaxation during interventional radiological procedures: effects on pain perception and intravenous drug use. Int J Clin Exp Hypn 1996;44:106-19. [Crossref] [PubMed]
- Schupp CJ, Berbaum K, Berbaum M, et al. Pain and anxiety during interventional radiologic procedures: effect of patients' state anxiety at baseline and modulation by nonpharmacologic analgesia adjuncts. J Vasc Interv Radiol 2005;16:1585-92. [Crossref] [PubMed]
- Viale-Nahon E. The role of hypnosis, relaxation and sophrology in the treatment of pain. Soins 1988.27-34. [PubMed]
- Pandey R. Four Decades of Sophrology and its Scientific Status. Indian Journal of Social Science Researches 2009;6:1-3.
- Caycedo N, Carsí Costas N, Van Rangelrooy K. Sofrology. Rev Enferm 2005;28:30-8. [PubMed]
- Casula C. Clinical hypnosis, mindfulness and spirituality in palliative care. Ann Palliat Med 2018;7:32-40. [Crossref] [PubMed]
- Brugnoli MP, Pesce G, Pasin E, et al. The role of clinical hypnosis and self-hypnosis to relief pain and anxiety in severe chronic diseases in palliative care: a 2-year long-term follow-up of treatment in a nonrandomized clinical trial. Ann Palliat Med 2018;7:17-31. [Crossref] [PubMed]
- Lang EV, Berbaum KS, Pauker SG, et al. Beneficial effects of hypnosis and adverse effects of empathic attention during percutaneous tumor treatment: when being nice does not suffice. J Vasc Interv Radiol 2008;19:897-905. [Crossref] [PubMed]
- Johnson DT, Spielberger CD. The effects of relaxation training and the passage of time on measures of state- and trait-anxiety. J Clin Psychol 1968;24:20-3. [Crossref] [PubMed]
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50-5. [Crossref] [PubMed]
- Boute V. Intérêt de l’hypnose en sénologie interventionnelle. Imagerie de la Femme 2013;23:149-55. [Crossref]
- Quintini D, Vitale C, Gaide M, et al. Hypnosis to fight against pain and anxiety in palliative care. Soins 2017;62:11-5. [Crossref] [PubMed]
- Lang EV, Rosen MP. Cost analysis of adjunct hypnosis with sedation during outpatient interventional radiologic procedures. Radiology 2002;222:375-82. [Crossref] [PubMed]


